[box type=”bio”] Learning Point of the Article: [/box]
Artificial bone grafting technique using the novel unidirectional β-tricalcium phosphate impregnated with bone marrow blood collected from normal unfractured vertebral bodies could promote formation of new bone in a case of non-union of otsteoporotic vertebral fracture with severe vertebral instability.
Case Report | Volume 9 | Issue 6 | JOCR November – December 2019 | Page 50-53 | Toru Funayama, Hiroshi Noguchi, Kentaro Mataki, Masashi Yamazaki. DOI: 10.13107/jocr.2019.v09.i06.1584
Authors: Toru Funayama[1], Hiroshi Noguchi[1], Kentaro Mataki[1], Masashi Yamazaki[1]
[1]Department of Orthopedic Surgery, Faculty of Medicine, University of Tsukuba, Tennodai, Tsukuba 3058575, Japan.
Address of Correspondence:
Dr. Toru Funayama,
Department of Orthopedic Surgery, Faculty of Medicine, University of Tsukuba, Tennodai, Tsukuba 3058575, Japan.
E-mail: funatoru3@md.tsukuba.ac.jp
Abstract
Introduction: For the treatment of non-union of osteoporotic vertebral fractures with severe instability, we developed an artificial bone grafting technique using a novel unidirectional β-tricalcium phosphate (Affinos®, Kuraray, Co., Ltd., Tokyo, Japan) impregnated with bone marrow blood collected from normal unfractured vertebral bodies to promote the formation of new bone.
Case Report: An 87-year-old woman exhibited gait disturbance due to delayed leg paralysis secondary to non-union of an osteoporotic fracture of the T12 vertebral body. Artificial bone grafting was performed with 7.5 g of the β-tricalcium phosphate granules impregnated with 12 mL of bone marrow blood collected from normal vertebral bodies, where pedicle screws would be inserted. Three months after surgery, the cortex of the anterior vertebral wall was regenerated, and bone union was completed. For up to 1 year after surgery, absorption of the artificial bone and formation of new bone had been observed.
Conclusion: Artificial bone grafting technique using the novel unidirectional β-tricalcium phosphate impregnated with bone marrow blood collected from normal unfractured vertebral bodies is a useful and innovative surgical technique for the treatment of non-union of osteoporotic vertebral fractures with severe vertebral instability.
Keywords: Osteoporotic vertebral fracture, non-union, unidirectional porous β-tricalcium phosphate.
Introduction
To treat non-union of osteoporotic vertebral fractures with severe instability, vertebroplasty is generally performed through a posterior transpedicular approach, in combination with pedicle screw fixation [1]. Autologous bone is an ideal prosthetic material for the treatment of this disorder. However, harvesting autologous bone from elderly patients with osteoporosis is limited by the amount and quality of available autologous bone, need for another incision for harvesting, time required for harvesting, and possible post-operative development of donor site pain, as well as skin and neurological disorders. Thus, we developed an alternative bone grafting technique. Newly developed β-tricalcium phosphate bone substitute with a unique unidirectional porous structure and porosity of 57% (Affinos®, Kuraray Co., Ltd., Tokyo, Japan) is impregnated with bone marrow blood collected from unfractured (normal) vertebral bodies and used in the bone grafting procedure. We report our first case treated with our technique, along with the analysis of post-operative temporal changes on imaging. The patient was informed that data from the case would be submitted for publication and gave her consent.
Case Report
An 87-year-old woman did not respond to conservative therapy for an osteoporotic fracture of the T12 vertebral body. After 2 months of conservative therapy, she exhibited delayed union and gait disturbance due to delayed leg paralysis. She was referred to our institution from a neighborhood hospital. The strength of the lower limbs (knee extension and ankle dorsiflexion) was rated manual max muscle test (MMT) 4 in the left limb and MMT 1 in the right limb. Old osteoporotic vertebral fractures were observed at levels L2 and L3. Plain radiography in flexion position revealed a markedly compressed T12 vertebral body (Fig. 1a), and T2-weighted magnetic resonance imaging in the supine position revealed a large bony defect in the vertebral body (Fig. 1b). 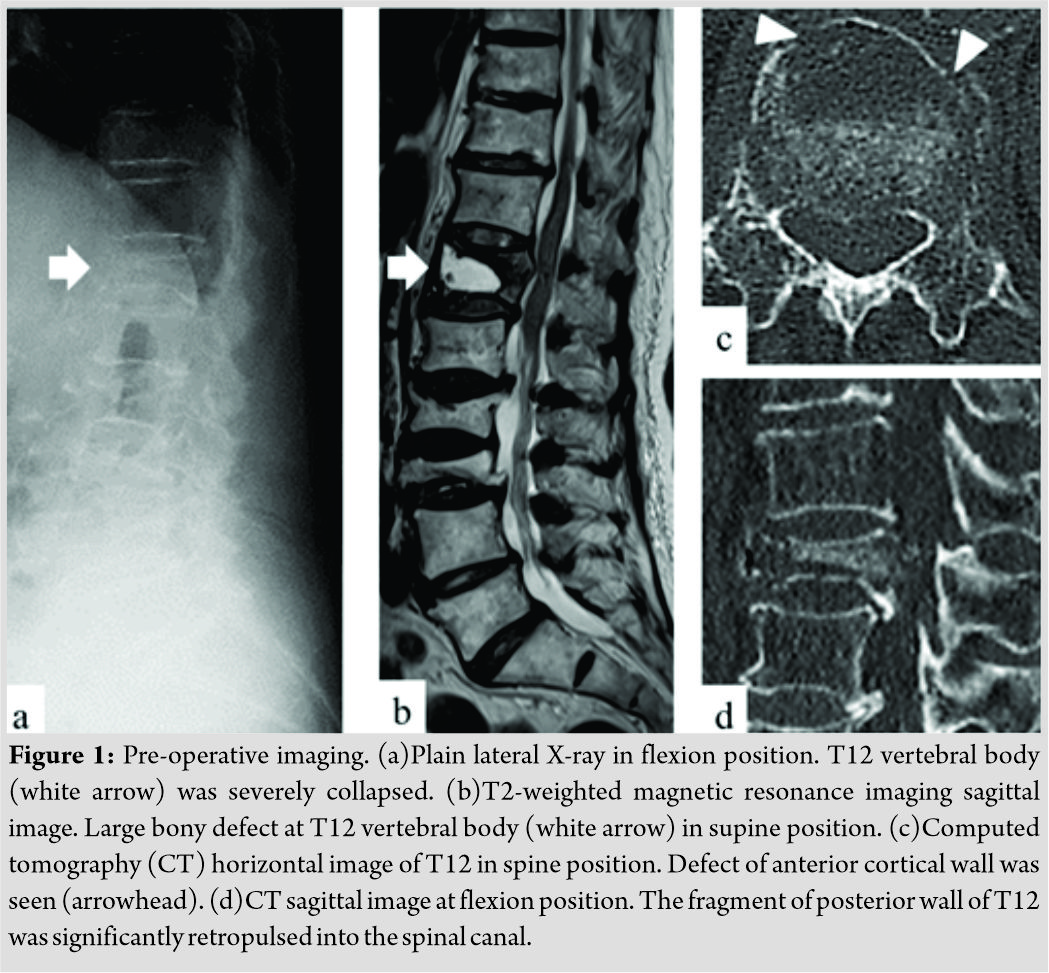
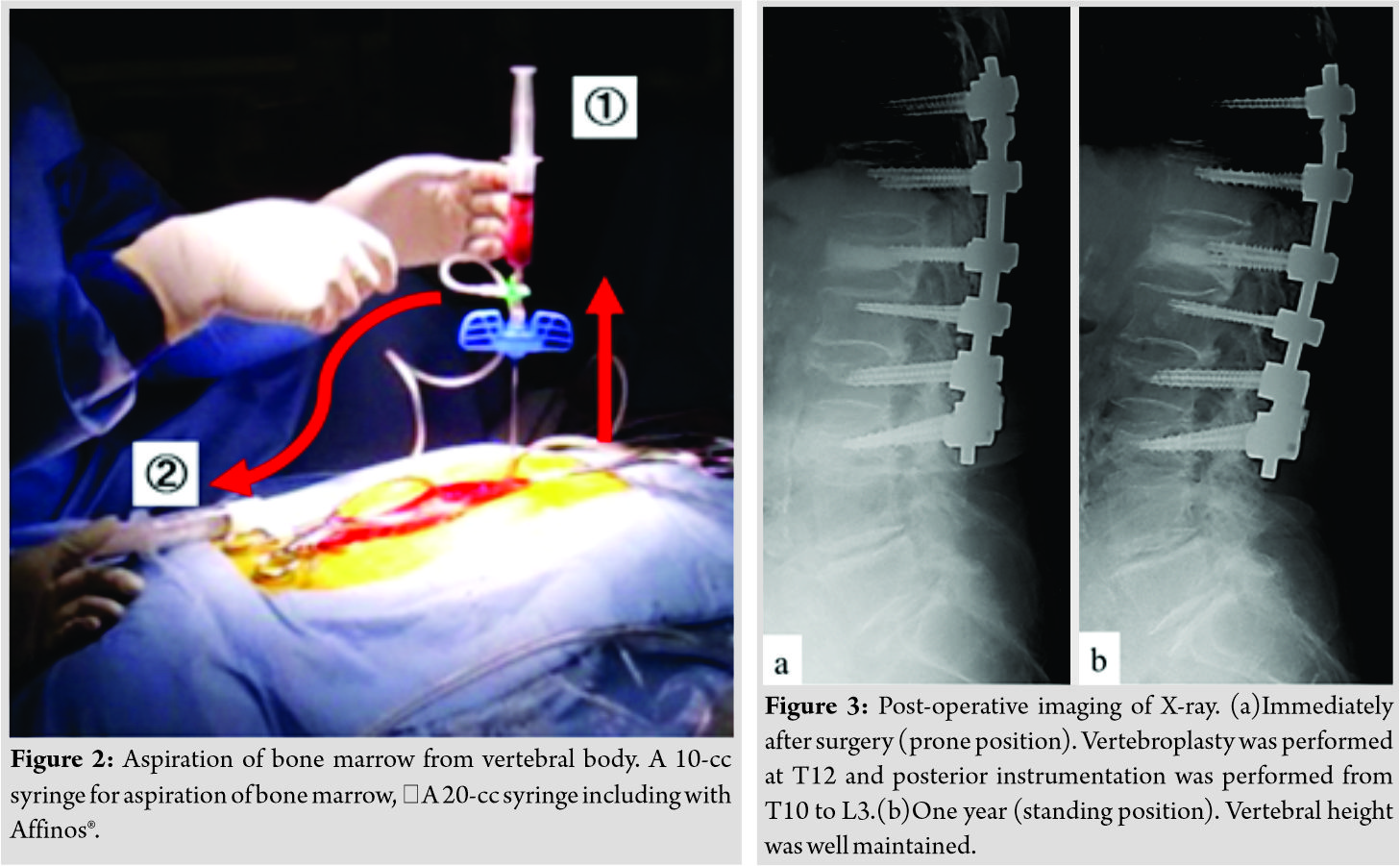
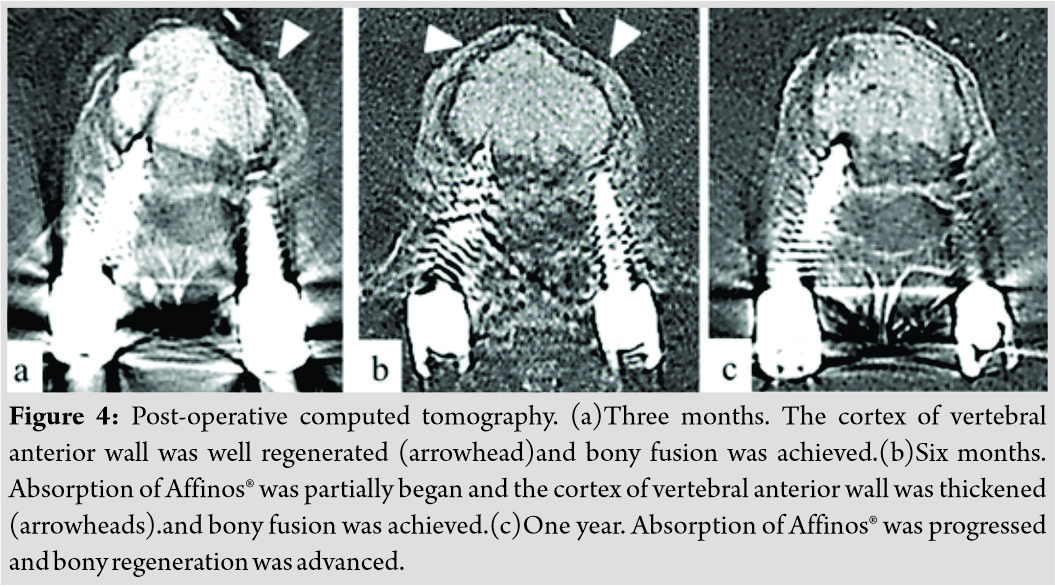
Surgery was performed with the patient in the prone position under general anesthesia. We selected vertebroplasty in combination with pedicle screw fixation instead of balloon kyphoplasty, which was often indicated painful osteoporotic vertebral fracture, due to the large cortical defect in the anterior vertebral wall. An 11-gauge guide needle was inserted from the left pedicle into a vertebral body under fluoroscopic guidance. Then, a 10-cc syringe was attached to the guide needle. Bone marrow blood (2–3 mL/vertebral body) was collected with high-pressure aspiration (Fig. 2①). The bone marrow blood was transferred into another 20-cc syringe filled with Affinos® granules to impregnate them (Fig. 2②). Next, a guidewire was inserted through the guide needle sheath and placed in a vertebral body. Then, the guide needle was removed, and hollow cannulated pedicle screws (Solera®, Medtronic Sofamor Danek, MN, USA) were inserted along the guidewire with conventional technique. In this manner, a total of 12 mL of fresh bone marrow blood werecollected from normal vertebral bodies between the levels T10 and L3. Subsequently, a 5-mm inserter for vertebroplasty (Kuraray Co., Ltd., Tokyo, Japan) was transpedicularly attached to the T12 vertebral body under fluoroscopic guidance, and Affinos® granules impregnated with bone marrow blood were injected under C-arm fluoroscopic guidance until the bone defect was completely filled. Finally, short pedicle screws were also inserted into the T12 vertebral body, and rods exactly reproducing the spinal alignment in the prone position were locked to the pedicle screws (Fig. 3a). To prevent screw back-out due to osteoporosis, two 5-mmwidth super-high-molecular-weight polyethylene tapes (Nesplon®, Alfresa Pharma, Osaka, Japan) each were passed under the laminae of T12T10and L3 to fasten the rods for reinforcement. Finally, the resected spinous process was ground into chips and implanted posteriorly on the laminae. The operative time was 290 min, and the volume of blood loss was 480 g.
Post-operative management included the use of a Jewett-type hard corset, and ambulation was allowed as early as possible. Teriparatide, which had been administered since the onset of this fracture, was continued for the treatment of osteoporosis. After surgery, leg paralysis resolved, and the patient was able to walk. Three months after surgery, mild correction loss was observed in the affected vertebral body height; however, CT revealed regeneration of the cortex of the anterior vertebral wall. We determined that bone union was completed (Fig. 4a). Six months after surgery, Affinos® granules were absorbed and became nearly as bright as adjacent autologous bone. Simultaneously, the cortex of the anterior vertebral wall was found to be further regenerated (Fig. 4b). One year after surgery, X-ray in the standing position revealed that vertebral height was well maintained (Fig. 3b). CT revealed that Affinos® granules were further absorbed. Meanwhile, the gap between the synthetic bone mass and the anterior vertebral wall, which had been observed at 6 months after surgery, had become unclear. Autologous bone was found to be further regenerated in the vertebral body (Fig. 4c).
Discussion
When delayed union or pseudarthrosis affects vertebral bodies after osteoporotic vertebral fractures, severe instability persists as the present case. Moreover, the inside of affected vertebral bodies is filled with necrotic or fibrous tissue [2]. In vertebral bodies associated with clefts, it is thought that blood flow into the vertebral bodies is blocked because thrombosis is frequently observed in the segmental arteries of the affected vertebral body [3]. To achieve favorable bone union in vertebral bodies under a combination of adverse conditions with such local instability and aseptic necrosis-like pathological conditions, filling of bone defects with prosthetic materials having excellent regeneration capacity is necessary, in addition to achieving local stability using instrumentation, such as pedicle screws. There is no dispute that autologous bone is essentially an ideal prosthetic material. However, in patients with severe osteoporosis, the amount and quality of autologous bone that can be harvested are limited. Affinos® bone substitute consists of β-tricalcium phosphate with unidirectional porous structure and high porosity of 57%. These have been demonstrated in animal experiments to be characterized by a fine balance between absorption of bone substitute and formation of new bone, as well as replacement by autologous bone [4, 5]. Only few clinical studies evaluating its implantation characteristics in humans have been reported [6, 7]. The present case is the first report of Affinos®used as an artificial bone grafting for spine surgery. Initially, when β-tricalcium phosphate was applied to the inside of vertebral bodies, in which the bone union process was delayed or paused as in our case, there was a concern that the bone substitute was only absorbed but not replaced by autologous bone. However, in our case, it was confirmed overtime that more than the expected amount of new bone was formed as the bone substitute was absorbed. This artificial bone substitute with a unique unidirectional porous structure can be rapidly impregnated with bone marrow blood containing cells through capillary action [5]. Although bone marrow blood is commonly collected from the ilium, it can also be collected from vertebral bodies [8]. The advantage of collecting bone marrow blood from vertebral bodies is that completely fresh blood can be collected from each vertebral body. Moreover, it has been reported that bone marrow blood collected from the elderly still has the capacity to form new bone [9]. It is also thought that the first 2–3 mL of collected bone marrow blood contains abundant myelocytes, regardless of age [10]. Recent reports have indicated that minimally invasive procedures using bone marrow blood have been performed for aseptic necrosis (e.g., femoral head necrosis) and pseudarthrosis of the long bones of the extremities [11, 12]. Thus, it seems logical to use bone marrow blood collected from normal vertebral bodies in combination with the novel unidirectional β-tricalcium phosphate bone substitute granules for the treatment of vertebral bodies affected by non-union due to pathological conditions similar to aseptic necrosis or pseudarthrosis, as in our case. In our surgical procedure, bone marrow blood is collected from vertebral bodies during the process of inserting pedicle screws so that little additional time is required to collect the bone marrow blood. Furthermore, because our technique does not require harvesting of bone grafts and does not cause bleeding, operative time and the volume of blood loss are reduced. Because there is no limit to the availability of artificial bone substitute, a sufficient amount can be injected to completely fill bone defects. This might also have contributed to reduction in time to bone union. Although the present case was the preliminary trial case and many basic aspects remain to be elucidated, Affinos® granules impregnated with bone marrow blood collected from normal vertebral bodies exerted excellent effects, even in implantation under one of the most unfavorable pathological conditions for bone regeneration, that is, non-union of osteoporotic vertebral fracture. Our technique appears to be an acceptable alternative to transplantation of autologous bone and can be applied in the treatment of this disorder.
Conclusion
Artificial bone grafting technique using the novel unidirectional β-tricalcium phosphate impregnated with bone marrow blood collected from normal unfractured vertebral bodies could promote the formation of new bone in a case of non-union of osteoporotic vertebral fracture with severe vertebral instability.
Clinical Message
Artificial bone grafting technique using the novel unidirectional β-tricalcium phosphate impregnated with bone marrow blood collected from normal unfractured vertebral bodies is a useful and innovative surgical technique for the treatment of non-union of osteoporotic vertebral fractures with severe vertebral instability.
References
1. KatsumiK, HiranoT, WatanabeK, OhashiM, YamazakiA, ItoT, et al. Surgical treatment for osteoporotic thoracolumbar vertebral collapse using vertebroplasty with posterior spinal fusion: A prospective multicenter study.Int Orthop2016;40:2309-15.
2. HasegawaK, HommaT, UchiyamaS, TakahashiH. Vertebral pseudarthrosis in the osteoporotic spine. Spine (Phila Pa 1976)1998;23:2201-6.
3. KimYC, KimYH, HaKY. Pathomechanism of intravertebral clefts in osteoporotic compression fractures of the spine.Spine J2014;14:659-66.
4. Sakane M, Tsukanishi T, Funayama T, Kobayashi M, Ochiai N. Unidirectional porous β-tricalcium phosphate bone substitute: Examination of balance between new bone formation and absorption. Key Eng Mater 2012;493-4:132-4.
5. Makihara T, Sakane M, Noguchi H, Yamazaki M. The balance between bone formation and material resorption in unidirectional porous β-tricalcium phosphate implanted in a rabbit tibia. Key Eng Mater 2016;696:177-82.
6. Ikumi A, Funayama T, Tsukanishi T, Noguchi H, Yamazaki M. Novel unidirectional porous β-tricalcium phosphate used as a bone substitute after excision of benign bone tumors of the hand: A case series.J Hand Surg Asian Pac Vol2018;23:424-9.
7. Izawa S, Funayama T, Iwasashi M, Tsukanishi T, Kumagai H, Noguchi H, et al. The use of unidirectional porous β-tricalcium phosphate in surgery for calcaneal fractures: A report of four cases. Foot Ankle Online J 2017;10:2.
8. MinWK, BaeJS, ParkBC, JeonIH, JinHK, SonMJ, et al. Proliferation and osteoblastic differentiation of bone marrow stem cells: Comparison of vertebral body and iliac crest.Eur Spine J2010;19:1753-60.
9. BeaneOS, FonsecaVC, CooperLL, KorenG, DarlingEM. Impact of aging on the regenerative properties of bone marrow, muscle, and adipose-derived mesenchymal stem/stromal cells.PLoS One2014;9:e115963.
10. HustedtJW, JegedeKA, BadrinathR, BohlDD, BlizzardDJ, GrauerJN. Optimal aspiration volume of vertebral bone marrow for use in spinal fusion.Spine J2013;13:1217-22.
11. YoshiokaT, MishimaH, AkaogiH, SakaiS, LiM, OchiaiN. Concentrated autologous bone marrow aspirate transplantation treatment for corticosteroid-induced osteonecrosis of the femoral head in systemic lupus erythematosus.Int Orthop2011;35:823-9.
12. SugayaH, MishimaH, AotoK, LiM, ShimizuY, YoshiokaT, et al. Percutaneous autologous concentrated bone marrow grafting in the treatment for nonunion.Eur J Orthop Surg Traumatol2014;24:671-8.
 |
 |
 |
 |
| Dr. Toru Funayama | Dr. Hiroshi Noguchi | Dr. Kentaro Mataki | Dr. Masashi Yamazaki |
| How to Cite This Article: Funayama T, Noguchi H, Mataki K, Yamazaki M. A Novel Unidirectional Porous β-tricalcium Phosphate Grafting Impregnated with Bone Marrow Blood Collected from Unfractured Vertebral Bodies for Non-union of Osteoporotic Vertebral Fracture: A Preliminary Case Report. Journal of Orthopaedic Case Reports 2019 Nov-Dec;9(6): 50-53. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com