[box type=”bio”] Learning Point of the Article: [/box]
In cases that are determined to be amenable to limb salvage for a mangled foot, if the patient wanted it, limb salvage should be the first-line treatment. It is essential to cooperate with experienced plastic surgeons from an early phase to achieve limb salvage.
Case Report | Volume 9 | Issue 6 | JOCR November – December 2019 | Page 58-61 | Takahiro Oda, Keisuke Oe, Atsushi Sakurai, Tomoaki Fukui, Takahiro Niikura, Ryosuke Kuroda. DOI: 10.13107/jocr.2019.v09.i06.1588
Authors: Takahiro Oda[1], Keisuke Oe[1], Atsushi Sakurai[2], Tomoaki Fukui[1], Takahiro Niikura[1], Ryosuke Kuroda[1]
[1]Department of Orthopaedic Surgery, Kobe University Graduate School of Medicine, 7-5-1, Kusunoki-cho, Chuo-ku, Kobe 650-0017, Japan,
[2]Department of Orthopaedic Surgery, Hyogo Prefectural Awaji Medical Center, Awaji 656-0021, Japan.
Address of Correspondence:
Dr. Keisuke Oe,
Department of Orthopaedic Surgery, Kobe University Graduate School of Medicine, 7-5-1, Kusunoki-cho, Chuo-ku, Kobe 650-0017, Japan.
E-mail: keisuke-oe@mtf.biglobe.ne.jp
Abstract
Introduction: It remains controversial whether amputation or limb salvage is the best approach for mangled foot cases because there are no clear criteria for treatment. We report a case of successful limb salvage for a mangled foot, with good outcomes.
Case Report: The patient was a 30-year-old man who sustained a crush injury to his left foot and ankle and lower legs in a car crash; he had severe open left foot and ankle fracture and bilateral open tibial shaft fractures. Blood flow was maintained by the posterior tibial artery, and the tibial nerve was intact. We stabilized the ankle using Kirschner wires on the day of injury. Plastic surgeons were consulted for early soft tissue coverage. Final fixation was performed 12 weeks after flap grafting; we grafted an autologous bone on the defect, according to the Masquelet technique. Four months after the final surgery, fullweightbearing gait was initiated. The patient is now capable of walking independently, with no pain, and is highly satisfied.
Conclusions: Limb salvage can be successfully performed even in a patient with a severely mangled foot. For successful salvage surgery with good outcomes, such patients should be managed by a team of experienced orthopedic and plastic surgeons from an early stage to achieve appropriate bone alignment and soft tissue coverage.
Keywords: Mangled foot, soft tissue injury, limb salvage.
Introduction
A mangled foot is characterized by injury to multiple organ systems, such as the bone, muscle, vascular system, nerves, and soft tissue, around the foot. It often occurs in severe traffic crashes,and the patients commonly experience compound fractures with significant soft tissue loss. Therefore, surgeons often have to make the difficult choice between amputating and salvaging the limb [1, 2]. In addition, limb salvage does not necessarily lead to good results [3,4]. No scoring system has been established regarding the methods of treating a mangled foot. In addition, it remains controversial whether amputation or limb salvage is the bestapproach because there are no clear criteria for treatment. If limb salvage is selected, the goal is to reconstruct the foot to enable the patient to walk without pain and to wear shoes. To achieve this, the surgical team must include experienced orthopedic and plastic surgeons. Selecting the appropriate reconstruction method and timing are also important. We describe the case of a patient with a mangled foot who was successfully treated with limb salvage, with good outcomes.
Case Report
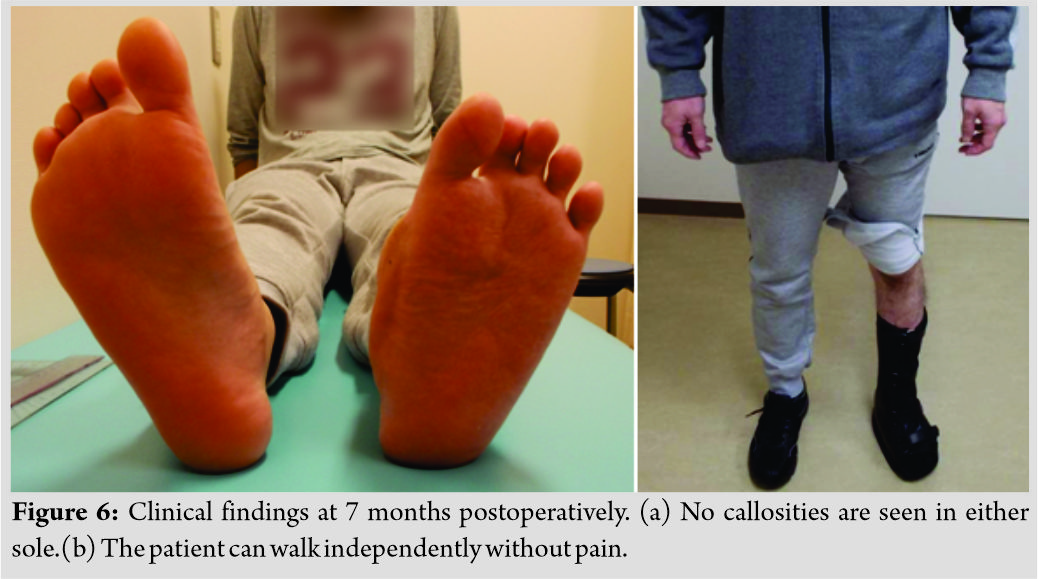
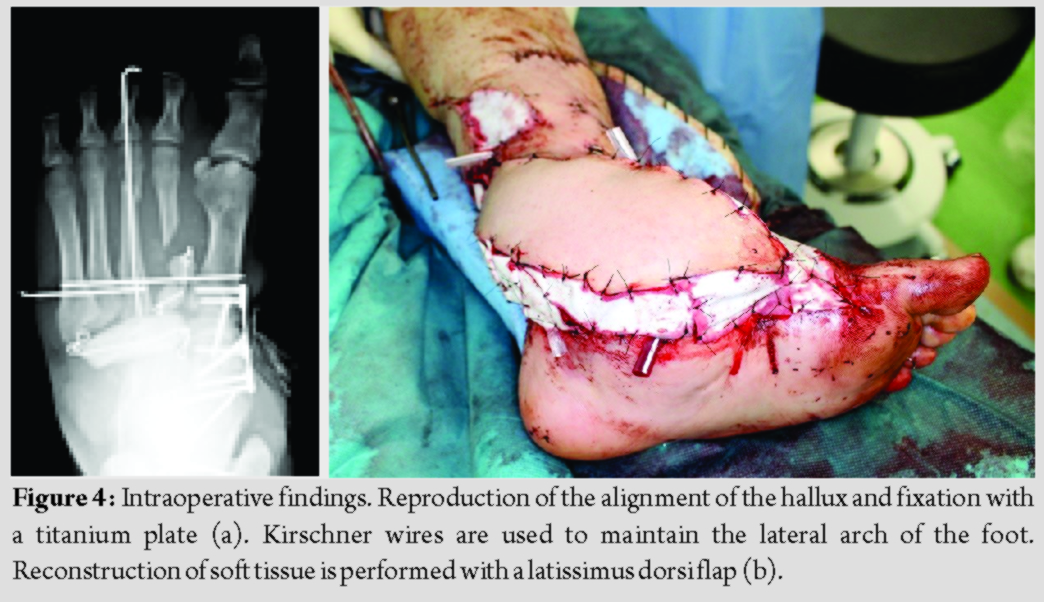
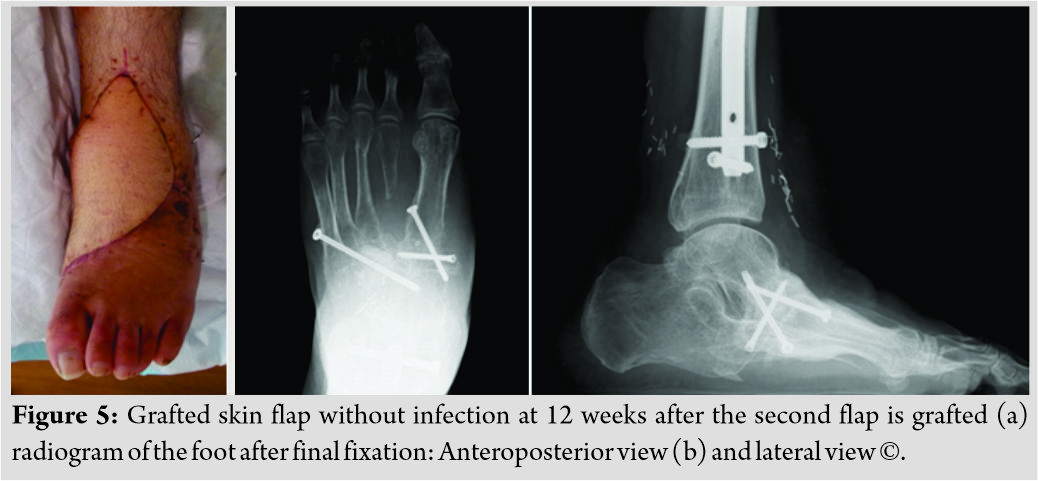
We informed the patient that data from his case would be submitted for publication, and he provided consent. A 30-year-old man with no underlying disease sustained a crush injury to his foot and ankle and lower legs in a car crash. He was brought to our hospital in an ambulance. He sustained open fractures to the left foot and ankle (Gustilo Anderson classification Type IIIB) and bilateral open tibial shaft fractures (the right was a TypeI and the other was a TypeII). The tarsal bones were crushed, and a part of the bone protruded from the wound (Fig. 1). There was no damage to important internal organs, such as the brain or heart, and his physical status was stable. The radiograph and computed tomography scan showed dislocation of the ankle joint; severe foot and ankle instability were seen (Fig. 2a and b). The mangled extremity severity score (MESS) was six and the limb salvage index (LSI) was five on arrival. Amputation is recommended when the MESS is ≥7 and LSI is ≥6 [5,6]. We opted to perform limb salvage, because the blood flow was maintained by the posterior tibial artery and the sensory nerve in the foot sole was intact. (Table 1) summarizes the lesion characteristics. The ankle and foot were stabilized using Kirschner wires (K-wire) on the day of injury. We maximally removed the necrotic tissue and bone. We also provided temporary fixation for both open tibial shaft fractures with external fixators and covered the soft tissue defect with artificial dermis. On the next day, we performed second-look surgery and started negative pressure wound therapy(NPWT). After several debridement procedures, a wide bone defect had developed in the midfoot (Fig. 3a and b).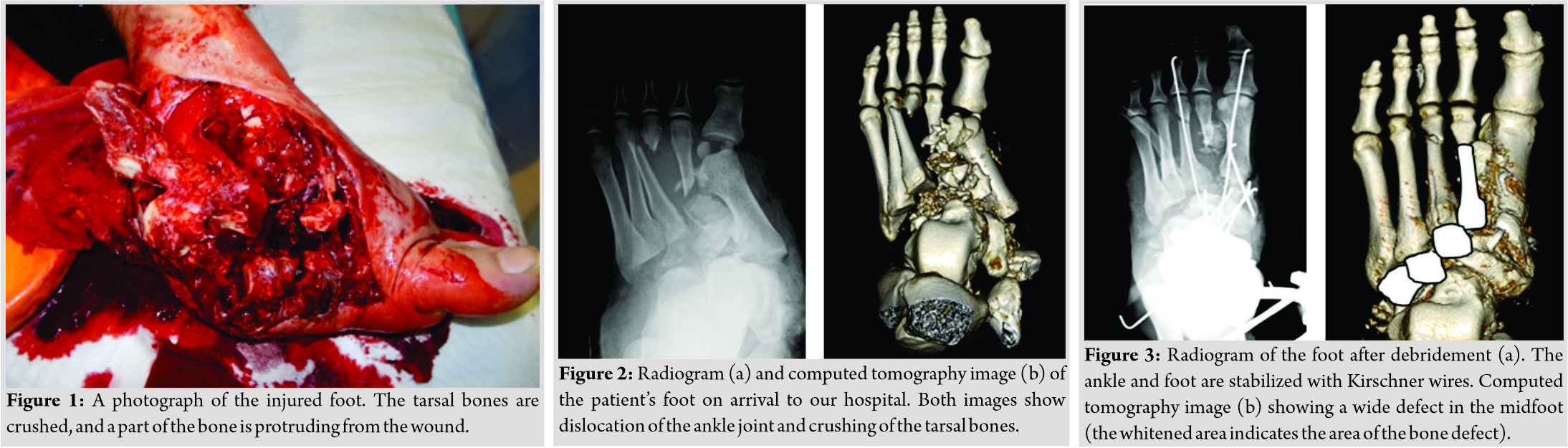
Discussion
Several scoring systems have been suggested for evaluating the severity of a mangled extremity, and some guidelines have been proposed[1,6].However, to the best of our knowledge, no scoring system has been established regarding methods of treatment of a mangled foot. Absolute indications for primary amputation of the mangled extremity are complete anatomical disruption of the posterior tibial nerve or crush injuries with a warm ischemia time longer than 6 h. These indications were not applicable to the current patient. We evaluated this case with the MESS [2, 5] and LSI. No scoring system recommended limb salvage. Due to the patient’s young age, we opted to perform limb salvage. In this case, the most important factors for successful salvage were the timing and method of reconstruction of soft tissues and bones. Ellington et al. reported no significant differences between the amputation group and the salvage group in terms of pain, walking speed, and return-to-work rate at 2 years, despite a longer time to full weight-bearing in the salvage group [3]. Shawen et al. reported that 75% of patients with failed limb salvage would have selected primary amputation in retrospect [4]. Limb salvage as the initial treatment should be selected after careful consideration. Limb salvage is primarily aimed at enabling the patient to walk without pain and to wear shoes. Early reconstruction of the soft tissue and stabilization of the bones are necessary to achieve these goals. Previously, Godina suggested that the optimal timing of free-flap transfer is the first 72 h after injury, reporting that the flap failure rate was significantly lower than that with reconstruction at later stages [7]. However, performing free-flap transfer within 72 h is often impossible because of the patient’s condition or the hospital’s situation. A recent study reported that NPWT reduces the complication rates of infection or osteomyelitis in open fractures in patients with delayed soft tissue coverage [8]. Steiert et al. reported that in the patients in whom soft tissue reconstruction was performed more than 72 h after the trauma, using NPWT before soft tissue coverage yielded similar results to those of immediate reconstruction [9]. The timing and method of soft tissue coverage are also very important. Therefore, it is essential to cooperate with experienced plastic surgeons from the early phase [10]. The latissimus dorsi muscle and ALT flap are considered graft sources for reconstruction. In our case, the latissimus dorsi flap was used first, and the ALT flap was then used since the former necrosed. The choice of flap also depends on the case; however, use of the ALT flap is generally a good technique for covering the foot, as it allows for thin, pliable coverage, enabling easy wear of shoes. During the reconstruction of the bones of the foot, we were careful to maintain not only the fundamental longitudinal arch but also the lateral arch to achieve an anatomical position as close to normal as possible. Several studies have reported that the induced membrane technique (Masquelet technique) is an effective treatment for post-traumatic bone defects [11, 12]. The Masquelet technique is adapted to patients with large diaphyseal defects undergoing bone reconstruction. It is performed in two stages. The first stage is the insertion of a cement spacer into the bone defect to induce a membrane. The second stage is the reconstruction of the defect autologous cancellous bone. The membrane prevents the resorption of the graft and favors its vascularity and corticalization [13]. In this case, there were large bone defects in the midfoot. We grafted a corticocancellous autologous bone from the iliac crest into the induced membrane; this is called the modified Masquelet technique [14]. Then, we fixed it using a CCS that passed through the fifth metatarsal, autologous bone, and talus for reconstruction. Moreover, we grafted cancellous bone chips around the other bone defect. Consequently, we achieved fixation of the forefoot and hind foot. After fixation, we fixed the ankle in a neutral position with a plaster cast for 8 weeks and allowed walking with partial weight-bearing after removing the cast. Full weight bearing gait was initiated 4 months after the final surgery. The rocker bottom shoe improves functional mobility and energy expenditure in post-stroke hemiplegic patients [15]. It was very useful in this patient during walking with weight-bearing because it allowed him to exercise his foot and regulate his ankle, enabling smooth plantarflexion. The patient reported a high level of satisfaction, and he is currently healthy.
Conclusion
Limb salvage can be successfully performed even in a patient with a severely mangled foot. For successful salvage surgery with good outcomes, such patients should be managed by a team of experienced orthopedic and plastic surgeons from an early stage to achieve appropriate bone alignment and soft tissue coverage.
Clinical Message
No scoring system has been established regarding the methods of treating a mangled foot. The MESS and LSI can be used as alternative scoring systems for determining the best course of treatment. In cases that are determined to be amenable to limb salvage, there are many disadvantages, such as high cost. However, if the patient is open to it, limb salvage should be the first-line treatment. If limb salvage is performed, it is essential to cooperate with experienced plastic surgeons from an early phase.
References
1. Bakota B. Kopljar M, Jurjević Z, Staresinić M, Cvjetko I, Dobrić I, et al. Mangled extremity–case report, literature review and borderline cases guidelines proposal. Coll Antropol2012;36:1419-26.
2. Patel MB, Richter KM, Shafi S. Mangled extremity: Amputation versus salvage. Curr Trauma Rep 2015;1:45-9.
3. Ellington K, Bosse MJ, Castillo RC, MacKenzie EJ; LEAP Study Group. The mangled foot and ankle: Results from a 2-year prospective study. J Orthop Trauma 2013;27:43-8.
4. Shawen SB, Keeling JJ, Branstetter J, Kirk KL, Ficke JR. The mangled foot and leg: Salvage versus amputation. Foot Ankle Clin 2010;15:63-75.
5. McNamara MG, Heckman JD, Corley FG. Severe open fractures of the lower extremity: A retrospective evaluation of the Mangled Extremity Severity Score (MESS). J Orthop Trauma 1994;8:81-7.
6. Scalea TM, DuBose J, Moore EE, West M, Moore FA, McIntyre R, et al. Western trauma association critical decisions in trauma: Management of the mangled extremity. J Trauma Acute Care Surg 2012;72:86-93.
7. Godina M. Early microsurgical reconstruction of complex trauma of the extremities. PlastReconstr Surg 1986;78:285-92.
8. Rezzadeh KS, Nojan M, Buck A, Li A, Vardanian A, Crisera C, et al. The use of negative pressure wound therapy in severe open lower extremity fractures: Identifying the association between length of therapy and surgical outcomes. J Surg Res 2015;199:726-31.
9. Steiert AE, Gohritz A, Schreiber TC, Krettek C, Vogt PM. Delayed flap coverage of open extremity fractures after previous vacuum-assisted closure (VAC) therapy-worse or worth? J PlastReconstrAesthet Surg 2009;62:675-83.
10. Nemoto M, Aoyagi K, Kashiwai S, Akimoto M, Ishikawa S, Kumazawa K, et al. Early reconstruction for open fracture to upper and lower extremities using free flap. Japan J Surg Wound Care 2010;1:74-80.
11. Karger C, Kishi T, Schneider L, Fitoussi F, Masquelet AC; French Society of Orthopaedic Surgery and Traumatology (SoFCOT). Treatment of posttraumatic bone defects by the induced membrane technique. OrthopTraumatol Surg Res 2012;98:97-102.
12. Giannoudis PV, Faour O, Goff T, Kanakaris N, Dimitriou R. Masquelet technique for the treatment of bone defects: Tips-tricks and future directions. Injury 2011;42:591-8.
13. Masquelet AC, Begue T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am 2010;41:27-37.
14. Largey A, Faline A, Hebrard W, Hamoui M, Canovas F. Management of massive traumatic compound defects of the foot. OrthopTraumatol Surg Res 2009;95:301-4.
15. Farmani F, Bandpei MA, Bahramizadeh M, Aminian G, Nikoo MR, Sadeghi-Goghari M. The effect of different shoes on functional mobility and energy expenditure in post-stroke hemiplegic patients using ankle-foot orthosis. ProsthetOrthot Int 2016;40:591-7.
 |
 |
 |
 |
 |
| Dr. Takahiro Oda | Dr. Keisuke Oe | Dr. Atsushi Sakurai | Dr. Takahiro Niikura | Dr. Ryosuke Kuroda |
| How to Cite This Article: Oda T, Oe K, Sakurai A, Fukui T, Niikura T, Kuroda R. Limb Salvage for a Mangled Foot: A Case Report. Journal of Orthopaedic Case Reports 2019 Nov-Dec;9(6): 58-61. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com