[box type=”bio”] Learning Point of the Article: [/box]
One should consider the possibility of Giant cell tumor of tendon sheath in case of finger swelling.
Case Report | Volume 9 | Issue 6 | JOCR November – December 2019 | Page 78-81 | Mukund Naresh Dhaniwala, Nareshkumar Satyanarayan Dhaniwala, Aquib Ahmed. DOI: 10.13107/jocr.2019.v09.i06.1598
Authors: Mukund Naresh Dhaniwala[1], Nareshkumar Satyanarayan Dhaniwala[2], Aquib Ahmed[2]
[1]Department of Orthopedics, Rajawadi Hospital, Ghatkopar, Mumbai, Maharashtra, India,
[2]Department of Orthopedics, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi, Wardha, Maharashtra, India.
Address of Correspondence:
Dr. Nareshkumar Satyanarayan Dhaniwala,
Jawaharlal Nehru Medical Collegeand AVBRH, Datta Meghe Institute of Medical Sciences (Deemed to be University),Sawangi (Meghe), Wardha – 442107, Maharashtra, India.
Email: nsdhaniwala@gmail.com
Abstract
Introduction: Giant cell tumor of the tendon sheath (GCTTS) is an uncommon benign soft tissue tumor of unknown etiology. It is seen more commonly in hand than ankle and foot. It presents as a painless and palpable swelling. Its diagnosis is mostly established by histopathology after surgical resection, although pre-operative imaging and fine-needle aspiration cytology (FNAC) support its suspicion. Herein, a case of GCT of flexor tendon sheath of the right index finger is reported due to its rarity.
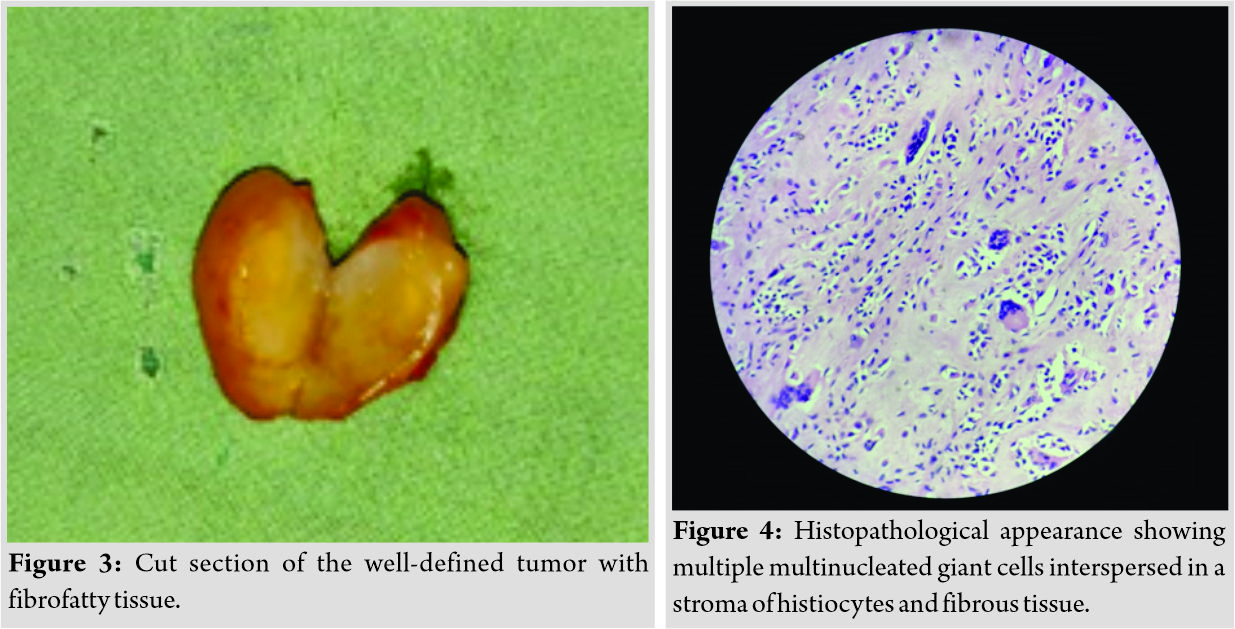
Case Report: A 46-year-old female presented with complaints of swelling over the front of the right index finger for 1½years. The swelling was spontaneous, painless, and very slowly progressive. Examination revealed a 2 cm × 1.5 cm firm swelling situated on the palmar aspect of the right index finger over distal part of middle phalanx and proximal part of the distal phalanx. Swelling was well defined, having smooth surface, uniformly firm consistency and could be moved sideways easily. X-ray of the hand showed localized soft tissue shadow in the involved area without any bony involvement. Ultrasonography of the finger showed soft tissue mass. FNAC examination reported the swelling as GCTTS. Excisional biopsy was done. Histopathology showed typical features of GCTTS.
Conclusion: GCTTS should be kept as a differential diagnosis in soft tissue tumors of hand in adults. FNAC followed by excisional biopsy is diagnostic and curative, but the patient should be followed up for detecting and managing recurrences.
Keywords: Giant-cell tumor, tendon sheath, excisional biopsy.
Introduction
Giant cell tumor of the tendon sheath (GCTTS) is a solitary, firm, and extra-articular localized benign soft tissue tumor presenting with painless swelling for many years. Overall incidence is 1 in 50,000 individuals and it commonly affects adults between the age of 30 and 50 years. It is more common in females with female-to-male ratio being 3:2 [1, 2]. It commonly affects small joints of the hand and feet but can be seen around ankle, knee, elbow, and hip. Complete local excision with or without radiotherapy is the preferred mode of treatment. Local recurrence is reported in 10–20% of cases. The entity was first described by Chassaignac, in 1852, as fibrous xanthoma [3]. The tumor has been named in literature as fibrous histiocytoma of synovium, pigmented nodular synovitis, tenosynovialGCT, localized nodular tenosynovitis, benign synovioma, sclerosing hemangioma, myeloid epithelioma, fibrohemosideric sarcoma, giant-cell fibrohemangioma, and fibrous xanthoma [3,4]. It is still controversial whether GCTTS is a neoplasm or bulk reactive proliferation [5]. About 15% of patients report some trauma preceding swelling, but its causative correlation is not established [6]. It was earlier considered as an inflammatory swelling, but the finding of aneuploidy in some cases and demonstration of clonal chromosomal abnormalities supports a neoplastic origin [7]. The most frequent location is fingers in the hand. The index finger is the most commonly involved digit followed by the middle, ring, little finger, and thumb [5, 8]. The reported case presents the classical features of GCTTS of the index finger.
Case Report
A 46-year-old female presented in the orthopedic outpatient department of our tertiary health-care center in Central India with the chief complaints of swelling over the front of the right index finger for 1½ years. The swelling developed spontaneously without any previous trauma or thorn prick. It increased gradually in size and caused little discomfort in day-to-day and household activities. The patient visited another tertiary care center in the area, where fine-needle aspiration cytology (FNAC) examination of the swelling was done, but further treatment could not be done, after which the patient visited our center. Examination revealed a 2 cm × 1.5 cm firm swelling situated on the palmar aspect of the right index finger over distal part of middle phalanx and proximal part of the distal phalanx (Fig. 1). There was no local rise of temperature or involvement of the skin. Swelling was well defined, its surface was smooth and consistency uniformly firm. The swelling could be moved sideways easily, but its mobility from proximal to distal was limited. There was no involvement of bone clinically. The swelling moved on movement of the finger.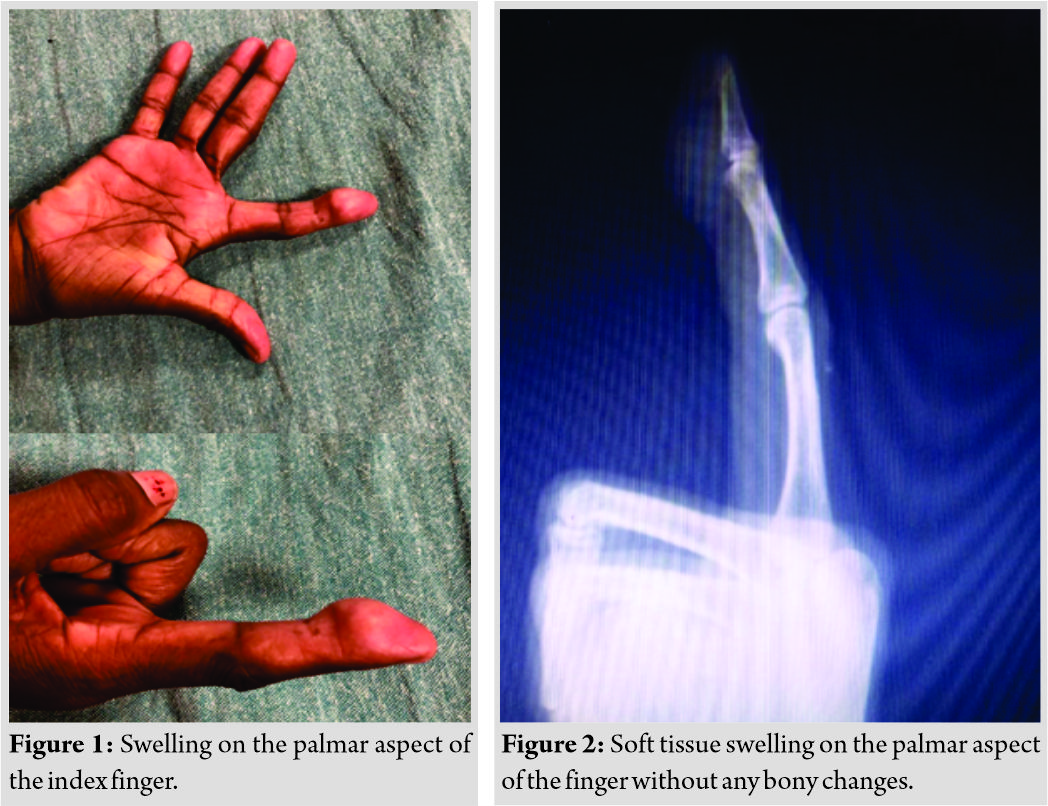
Discussion
GCTTS starts spontaneously, although some patient may feel its onset after minor trauma [6]. It is free from overlying structures but may cause indentation on bone if it is large in size and long standing in duration. It usually does not cause functional disability; hence, the patient presents late. It is common in the hand, though described in ankle and foot also [1, 2, 3, 4, 5]. The foot and ankle GCTTS accounts for 3–5% of all GCTTS in the body, with most located in the hand. GCTTS is seen on the lateral aspect of ankle and dorsum of foot, commonly involving extensor tendons, in which case misdiagnosis is likely. In the hand, it is seen on flexor aspect commonly. Kant et al. [1] reviewed 26 cases of GCTTS with the minimum follow-up for 2 years. He found it most commonly in the age group between 21 and 40 years. He noted bony indentation in 7 of these 26 cases. GCTTS can have two clinical presentations. The most common type is localized or nodular type. Localized nodular type is common in the hands, while diffuse type is common in joints. Few cases of malignant GCTTS have also been reported [5]. The other less common type is diffuse type, which recurs at a high rate and its treatment may require multiple increasingly morbidity causing procedures [9]. Pexidartinib drug has been used effectively for decreasing the size of this tumor [9]. Lautenbach et al. [8] analyzed 84 cases of GCTTS. His study did not find any soft tissue imaging method superior for the diagnosis or for the pre-operative planning. Tumors have been reported as both hypoechoic and hyperechoic on sonography [10]. Levi and Crafton [11] described role of magnetic resonance imaging (MRI) in early diagnosis of GCTTS. On MRI, it is seen as low signal intensity on both T1- and T2-weighted images and its accurate size and extent can be measured, helping in the surgical approach. MRI cannot differentiate between GCTTS, villonodular synovitis, synovial chondromatosis, and synovial sarcoma; hence, histopathological confirmation is must. Local recurrence of GCTTS has been reported variously from 4.7%, 14.8%, to 45% [12,13,14,15]. Di Grazia et al. [12] reviewed 64 cases and reported recurrence in 4.7%, tendon involvement in 10.9%, and bone erosion in 4.7% of cases. Factors predicting recurrence include pressure erosion on X-rays, location of tumor at IP joints, presence of osteoarthritic changes, and incomplete surgical excision. Thumb IP and DIP joint tumors recur more frequently. Lower rate of recurrence is expected when surgeon uses operating microscope or magnifying loop for resecting tumor. Kotwal et al. [13] suggested post-operative use of radiotherapy of 20 Gy in daily doses of 2 Gy in cases having predictive factors and found 0% recurrence rate in a series of 14 cases. The role of histology of tumor and radiotherapy remains inconclusive and controversial. Incomplete excision and leaving behind satellite nodules, more likely at IP joints, are considered as the most important factor for recurrence. GCT of bone on the contrary shows recurrence commonly if treated only by intralesional curettage. The use of bone cement and/or bone graft after curettage reduces recurrence rate. Wide excision of tumor with reconstruction shows lower recurrence rate [16]. However, in GCT of bone metastatic tumors may occur despite using multimodal treatment also. Receptor activator nuclear kappa-B ligand expression has been found to be a reliable prognostic marker in predicting the risk of local recurrences by Ghani et al. [17]. The reported case presented in the usual way as a benign tumor. The diagnosis was suspected on FNAC and confirmed on histopathology of the surgically excised specimen. The patient does not show any clinical or ultrasound evidence of recurrence at 6 months. Further, follow-up for at least 2 years is planned to note any recurrence.
Conclusion
GCTTS should be kept as a differential diagnosis in soft tissue tumors of hand in adults. FNAC followed by excisional biopsy is diagnostic and curative, but the patient should be followed up for detecting and managing recurrences.
Clinical Message
Although uncommon, GCT of the tendon sheath should be considered as a differential diagnosis of benign tumors in the hand and feet in adults.
References
1. Kant KS, Manav AK, Kumar R, Abhinav, Sinha VK, Sharma A. Giant cell tumour of tendon sheath and synovial membrane: A review of 26 cases. J Clin Orthop Trauma 2017;8 Suppl 2:96-9.
2. Rukavina I, Caleta D. Giant-cell tumor of the tendon sheath. A review. OA Orthop2014;2:11.
3. Darwish FM, Haddad WH. Giant cell tumor of tendon sheath: Experience with 52 cases. Singapore Med J 2008;49:879-82.
4. Adams EL, Yoder EM, Kasdan ML. Giant cell tumor of tendon sheath: Experience with 65 cases. Eplasty 2012;12:e50.
5. Monaghan H, Salter DM, Al-Nafussi A. Giant cell tumour of tendon sheath (localized nodular tenosynovitis) clinicopathological features of 71 cases. J Clin Pathol2001;54:404-7.
6. Fawi HM, Dojcinov S, Lyons K, Matthews TJ. Trauma or tumor: Giant cell tumour of distal biceps tendon sheath, an unusual cause of elbow pain. Shoulder Elbow 2019;11:137-9.
7. Sun C, Seng W, Yu H, Han J. Giant cell tumour of the tendon sheath: A rare case in the left knee of a 15-year-old boy. Oncol Lett 2012;3:718-20.
8. Lautenbach M, Kim S, Millrose M, Eisenschenk A. Nodular giant cell tumour of the tendon sheathof the hand: Analysis of eighty-four cases: Diagnostic decisions and outcome. Int Orthop2013;37:2211-5.
9. Giustini N, Bernthal NM, Bukata SV, Singh AS. Tenosynovial giant cell tumor: Case report of a patient effectively treated with pexidartinib (PLX3397) and review of the literature. Clin Sarcoma Res 2018;8:14.
10. Wang Y, Tang J, Luo Y. The value of sonography in diagnosing giant cell tumors of tendon sheath. J Ultrasound Med 2007;26:1333-40.
11. Levi M, Crafton J. Rare Giant Cell Tumor of the distal flexor digitorum longus tendon sheath and early diagnosis with use of magnetic resonance imaging. J Am Podiatr Med Assoc 2017;107:333-6.
12. Di Grazia S, Succi G, Fraggetta F, Perrotta RE. Giant call tumor of tendon sheath: Study of 64 cases and review of literature. G Chir2013;34:149-52.
13. Kotwal PP, Gupta V, Malhotra R. Giant-cell tumor of the tendon sheath. Is radiotherapy indicated to prevent recurrence after surgery? J Bone Joint Surg Br 2000;82:571-3.
14. Messoudi A, Fnini S, Labsaili N, Ghrib S, Rafai M, Largab A. Giant cell tumor of the tendon sheath of the hand: 32 cases. Chir Main 2007;26:165-9.
15. Grover R, Grobbelaar AO, Richman PI, Smith PJ. Measurement of invasive potential provides an accurate prognostic marker for giant cell tumor of tendon sheath. J Hand Surg Br 1998;23:728-31.
16. Frank MK, Doris EW, Carrie YI, Peter SR, Franklin HS. Giant cell tumor of bone: Risk factors for recurrence. Clin Orth Relat Res 2011;469:591-9.
17. Ghani SA, Wan Ismail WF, Md. Salleh MS, Yahaya S, SyahrulFitri ZM. The values of receptor activator nuclear kappa-B ligand expression in stage III giant cell tumor of the bone. Indian J Orthop2018;52:31-4.
 |
 |
 |
| Dr. Mukund Naresh Dhaniwala | Dr. Nareshkumar Satyanarayan Dhaniwala | Dr. Aquib Ahmed |
| How to Cite This Article: Dhaniwala M N, Dhaniwala N S, Ahmed A. A Case Report of Giant Cell Tumor of Flexor Tendon Sheath in Index Finger. Journal of Orthopaedic Case Reports 2019 Nov-Dec;9(6): 78-81. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com