[box type=”bio”] Learning Point of the Article: [/box]
The deep flexor tendon may become trapped in fracture of the phalanx diaphysis.
Case Report | Volume 9 | Issue 6 | JOCR November – December 2019 | Page 86-89 | Marco Bernardes, Moisés Ventura, Rita Grazina, Luís Miragaia, Guido Duarte, Pedro Canela. DOI: 10.13107/jocr.2019.v09.i06.1602
Authors: Marco Bernardes[1], Moisés Ventura[1], Rita Grazina[1], Luís Miragaia[1], Guido Duarte[1], Pedro Canela[1]
[1]Department of Orthopaedic, Ortophaedics and Traumatology Service of Centro Hospitalar de Vila Nova de Gaia/Espinho, Gaia, Portugal.
Address of Correspondence:
Dr. Marco Bernardes,
Department of Orthopaedic, Orthopaedics and Traumatology Service of Centro Hospitalar de Vila Nova de Gaia/Espinho, Gaia, Portugal.
E-mail: marco.silva.bernardes@gmail.com
Abstract
Introduction: The proximal phalanx fracture is a common fracture of the hand in pediatric ages. Most of these fractures can be treated conservatively with immobilization. There are only few cases reporting tendon entrapment in literature and most of them refer to epiphyseal fractures with only one case reporting tendon entrapment after diaphyseal fracture.
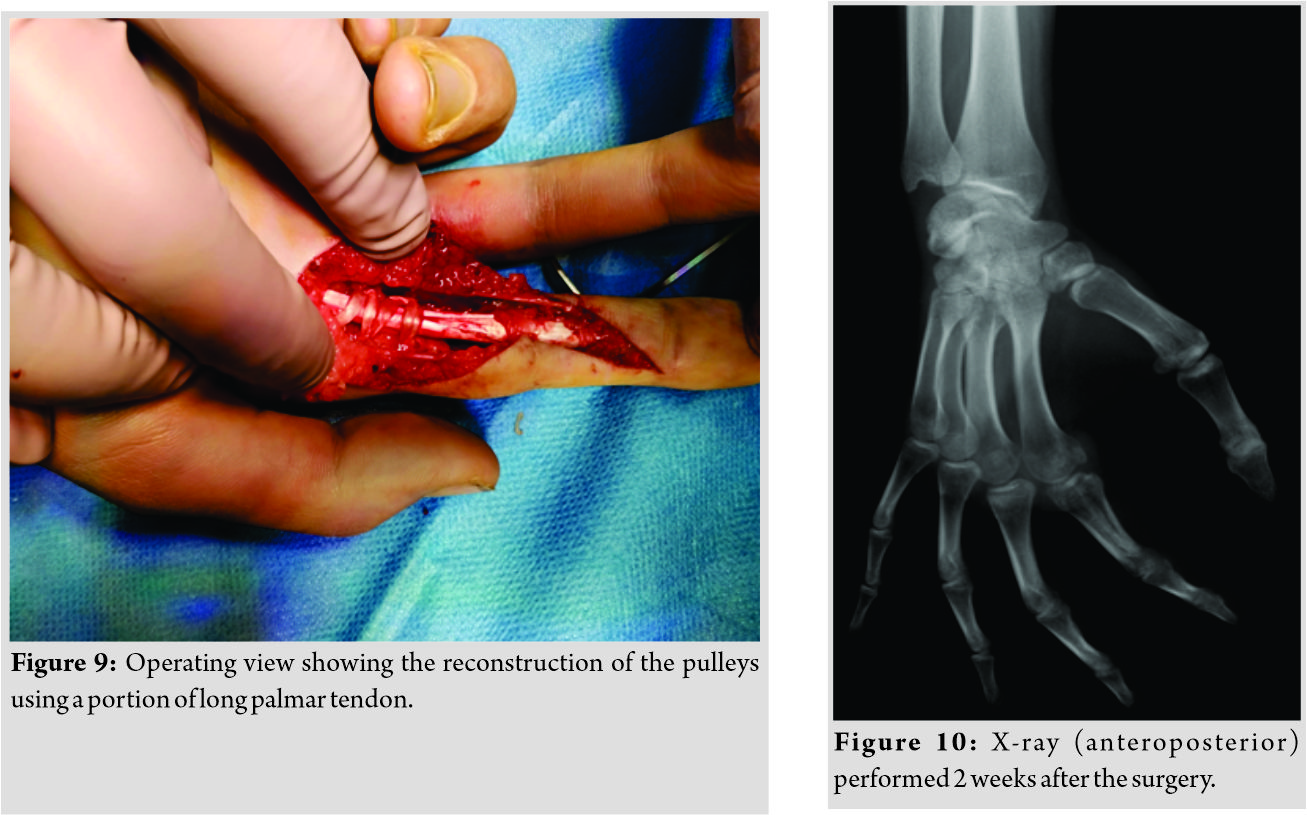
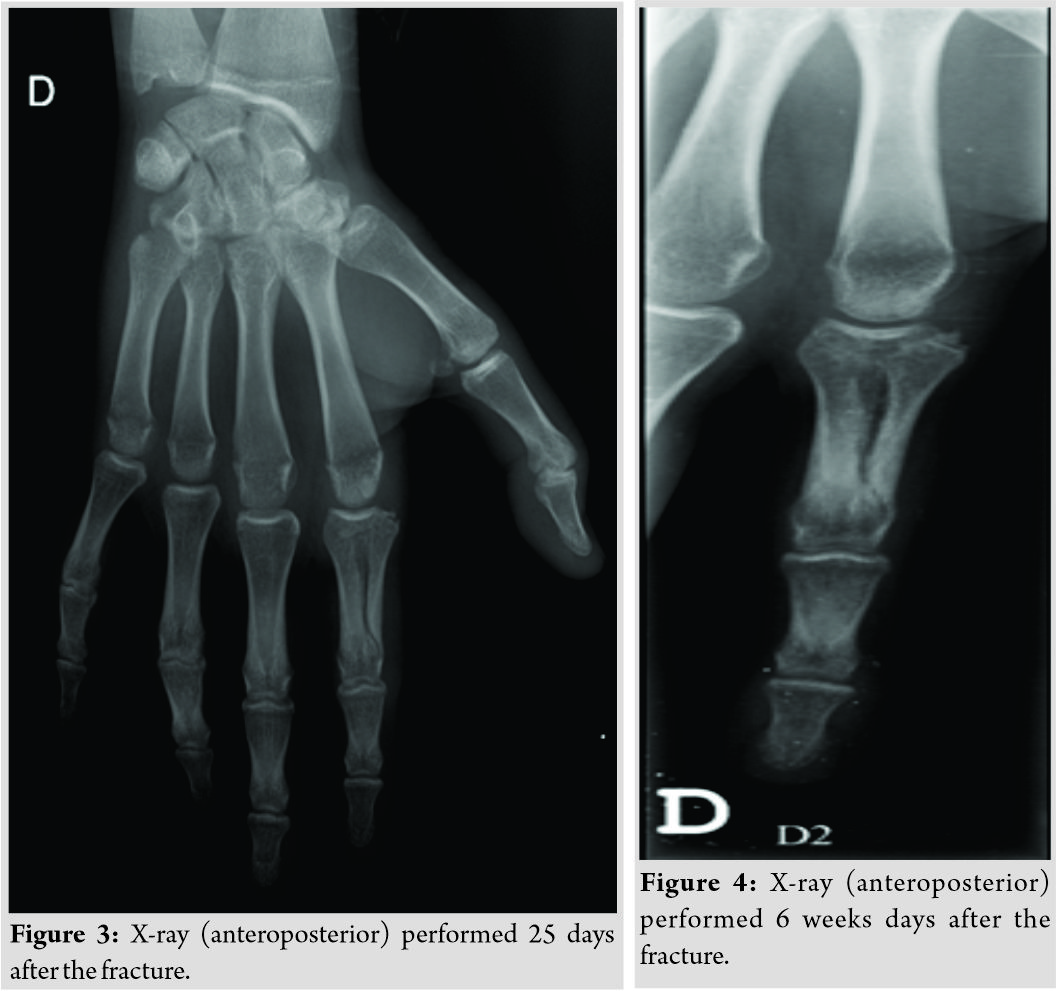
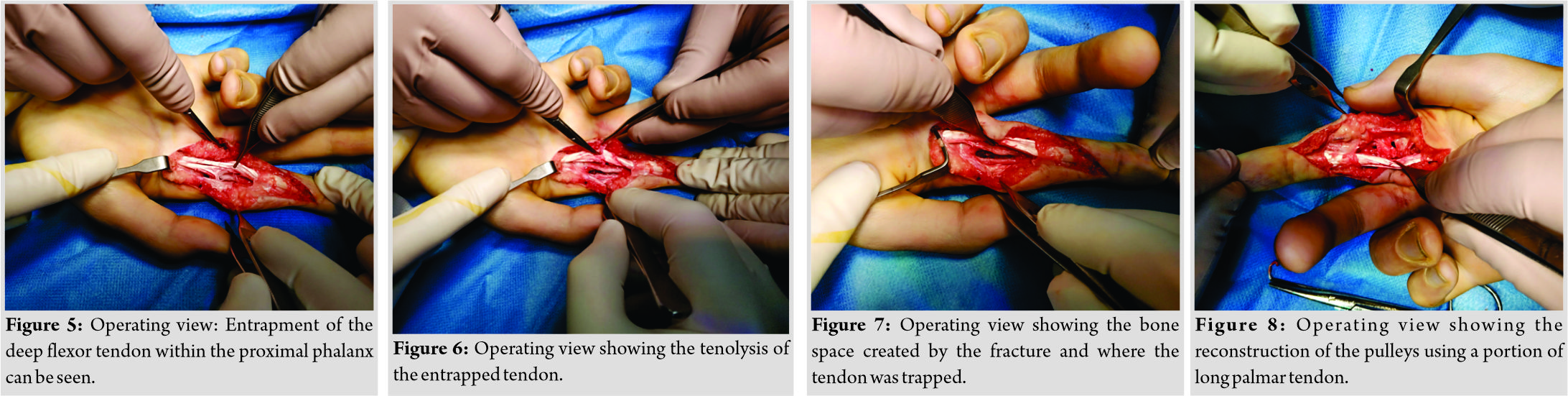
Case Report: A 15-year-old boy went to the emergency department after suffering trauma in his right hand caused by a fall. He complained of pain in his second finger of the right hand which was swollen. An imaging study was performed and a fracture of the proximal phalanx diaphysis of the second finger of the right hand was diagnosed. Due to deviation, reduction, syndactyly, and immobilization with Zimmer splint were performed. The control X-ray showed acceptable reduction and the patient was referred for follow-up at an outpatient consultation. During follow-up, the reduction was maintained and the conservative treatment was kept for 25 days, with apparent fracture healing. The patient presented active flexion limitation of the finger that was interpreted as a sequel of the immobilization and he was referred for physical therapy rehabilitation. Six weeks after the initial trauma, the patient was observed at the emergency department for new right-hand trauma. On examination, no active flexion of the third phalanx of the second finger of the right hand was noticed. The patient underwent an ultrasound that revealed deep flexor tendon entrapment at the fracture focus. A surgery was performed consisting in tenolysis and reconstruction of the pulleys using a portion of the long palmar tendon. The patient has good clinical evolution with almost complete recovery of mobility.
Conclusion: This case illustrates an entrapment of deep flexor tendon after a diaphyseal fracture of the proximal phalanx, with only few cases reported in literature. The authors highlight the importance of having a high index of suspicion to detect this situation once it restrains the success of the conservative treatmentand makes the surgery mandatory to avoid definite sequels and disabilities.
Keywords: Tendon entrapment, Diaphyseal fracture of the proximal phalanx, Tenolysis.
Introduction
The proximal phalanx is the most commonly fractured hand bone in children [1, 2, 3], being the base of phalanx the most common location. This is due to the high incidence of juxta-epiphyseal as well as Salter–Harris type II fractures [1, 2]. Most of these fractures are simple to reduce and are stable. However, when there is a soft tissue entrapment within the fracture, close reduction may become difficult or impossible and, when undiagnosed, may result in definite dysfunction of the affected finger. This entrapment is very rare with only few cases reported in literature and different anatomic structures were described such as extensor hood-periosteal fibrous tissue, lumbrical and interosseous tendons [4, 5, 6], as well as tendons [7, 8, 9, 10, 11, 12, 13, 14]. There are only few cases in literature reporting tendon entrapment after the fracture of the proximal phalanx [7, 8, 9, 10, 11, 12, 13, 14] with only one case occurring after diaphyseal fracture [12].
Case Report
A 15-year-old Caucasian boy with no relevant medical history went to the emergency department after suffering trauma in his right hand caused by a fall forward while playing football. He presented a deformity at the base of the second finger, swelling, and painfully restricted motion. Rotational deformity of the second finger associated with radial deviation and hyperextension was found during physical examination, but neurovascular structures were intact. The X-ray (Fig. 1) showed fracture of the proximal phalanx diaphysis of the second finger of the right hand with deviation. Closed reduction under sedation was performed applying traction and ulnar deviation followed by syndactyly and immobilization with Zimmer splint. 
Discussion
This case illustrates an entrapment of the deep flexor tendon after the fracture of the proximal phalanx of the second finger of the right hand which was not noticed at the time of primary closed reduction, leading to flexion limitation of the involved finger. This is a very rare entity with only seven cases reported in literature [7, 8, 9, 10, 11, 12, 13, 14].
(Video 1)
| https://www.youtube.com/watch?v=YHZKCMw5xBU&feature=youtu.be |
Most of the reported cases of tendon entrapment after the fracture of the proximal phalanx occurred in children between 4 and 12yearsold and in the majority of cases, a girl was affected [11]. The predominance of these fractures in pediatric age may explain why the epiphysis is the most frequent location of the fractures involved in the entrapment [7, 8, 9, 10, 11, 12, 13, 14]. Consequently, the most commonly affected fingers by the entrapment are the same affected by the juxta-epiphyseal/ Salter–Harris fractures, with the small finger being the most frequently involved, followed by the ring and long finger [11]. In some cases, the entrapment occurred in more than one finger [11]. Moreover, the deep flexor tendon is the most commonly involved in such entrapments due to its proximity to the bone [11], as happened in our case. The case presented has some special features that are different from the ones previously reported. At first, in our case, the tendon entrapment occurred in a 15-year-old boy. Furthermore, the fracture occurred in the diaphysis instead of the most common location in the epiphysis/peri-epiphyseal region (juxta-epiphyseal/ Salter–Harris fractures). At the best of our knowledge, this is the second case, in which the tendon entrapment occurred in a diaphysis fracture of the phalanx. The other case of entrapment reported after a diaphyseal fracture occurred in 45-year-old men and the second finger was the involved one [12]. In both cases, the patients were older when compared with the cases of entrapment after juxta-epiphyseal/ Salter–Harris fractures. On the one hand, this fact can explain the location of the fractures in the diaphysis and, on the other hand, it can justify the involvement of a finger different from the ones usually involved by juxta-epiphyseal/Salter–Harris fractures. As the fractures of the phalanx are much more frequent in children, it is easy to understand the reason why these fractures are juxta-epiphyseal. As skeleton matures, the phalanx loses its “fragile point” and the fractures are more able to occur in the diaphysis. The other point that must be discussed in our case is the fact that the entrapment went unnoticed at the time of primary closed reduction. Usually, phalanges fractures do not present difficulties related with reduction or post-reduction stability [5]. However, in some cases, it may be difficult or impossible to reduce the fracture due to soft tissue entrapment [4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14]. Some clues must raise suspicion of the presence of flexor tendon entrapment in these kinds of fractures, namely, severe swelling, dorsal angulation of the digit after a severe hyper extension injury, a rubbery resistance to manipulation, and failure in successive attempts to reduce [1, 2, 3]. It is important to take this into account as repeated attempts at closed reduction may result in an increase in swelling and damage of the growth plate (when juxta-epiphyseal/ Salter–Harris fractures are present) or the entrapped tissues [5, 9]. In our case, although the undiagnosed tendon entrapment, it was possible to perform a closed reduction in a single attempt with both apparent good immediate clinical and image results which delayed the diagnosis and the definite treatment. Pandey et al. have reported a case, in which the tendon entrapment remained unnoticed and present late as tendon dysfunction and the definite diagnosis of the entrapment was made by sonography as in our case [14]. Taking into account, the few cases reported, the best surgical approach to treat flexor tendon entrapment is not defined. Some authors have used dorsal approach, others mid-lateral approach, and others volar approach [12]. In our case, given that, the fracture was already consolidated, we opted for a volar approach that proved to be the best since it allowed not only the tenolysis but also the reconstruction of the pulleys using a portion of the long palmar tendon, which was very important to obtain a good functional result.
Conclusion
This case is an original case report that illustrates a deep flexor tendon entrapment after a diaphyseal fracture of the proximal phalanx of the second finger in a 15-year-old boy. This entity is very rare, especially taking into account its occurrence in the diaphysis, being the second case reported in literature. The authors highlight the importance of having a high index of suspicion to detect this situation once it restrains the success of the conservative treatment and makes the surgery mandatory to avoid definite sequels and disabilities.
Clinical Message
With this paper, the authors pretend to illustrate a deep flexor tendon entrapment after a diaphyseal fracture of the proximal phalanx in a 15-year-old boy which is a very rare entity, especially taking into account its occurrence in the diaphysis. The authors highlight the importance of having a high index of suspicion to detect this situation once it restrains the success of the conservative treatment and makes the surgery mandatory to avoid definite sequels and disabilities.
References
1. Kralj R, Barcot Z, Vlahovic T, Kurtanjek M, Petracic I. The patterns of phalangeal fractures in children and adolescents: A review of 512 cases. HandchirMikrochirPlastChir2019;51:49-53.
2. Al-Qattan MM, Al-Zahrani K, Al-Boukai AA. The relative incidence of fractures at the base of the proximal phalanx of the fingers in children. J Hand Surg Eur Vol 2008;33:465-8.
3. Cornwall R, Ricchetti ET. Pediatric phalanx fractures: Unique challenges and pitfalls. Clin OrthopRelat Res 2006;445:146-56.
4. Yamane T. Irreducible juxta-epiphyseal fracture due to entrapment of extensor hood: A case report. Hiroshima J Med Sci 1999;48:99-100.
5. Cowen NJ, Kranik AD. An irreducible juxta-epiphyseal fracture of the proximal phalanx. Report of a case. Clin OrthopRelat Res 1975;110:42-4.
6. Sopher M, Gopalgi B, Spencer JD. Interposition of the dorsal interosseous tendon in a fracture of the base of the proximal phalanx of the right ring finger. Injury 1989;20:53-4.
7. Freedman EL, Vander Griend RA, Dell PC. Tendon interposition in a juxta-epiphyseal fracture of the proximal phalanx. J Hand Surg Br 1998;23:558-9.
8. Nogueira A, Alvarez R, Iglesias F. Irreducible phalangeal fracture in a child due to flexor tendon entrapment. J Hand Surg Am 1999;24:924-7.
9. Harryman DT 2nd, Jordan TF 3rd. Physeal phalangeal fracture with flexor tendon entrapment. A case report and review of the literature. Clin OrthopRelat Res 1990;250:194-6.
10. Von Raffler W. Irreducible juxta-epiphyseal fracture of a finger. J Bone Joint Surg Br 1964;46B:229.
11. Rodríguez-Vega V, Pretell-Mazzini J, Marti-Ciruelos R, Jorge-Mora A, de la Mano AC. Simultaneous juxta epiphyseal proximal phalanx fracture with flexor tendon entrapment in a child: A case report and review of literature. J PediatrOrthop B 2013;22:148-52.
12. Woo SH, Kim JS, Gong HS. A flexor digitorum longus tendon entrapment in a diaphyseal fracture of the proximal phalanx caused by crushing injury. Injury Extra 2005;36:32-5.
13. Lee YK, Park S, Lee M. Flexor tendon entrapment at the malunited base fracture of the proximal phalanx of the finger in child: A case report. Medicine (Baltimore) 2015;94:e1408.
14. Pandey T, Al Kandari SR, Al Shammari SA. Sonographic diagnosis of the entrapment of the flexor digitorum profundus tendon complicating a fracture of the index finger. J Clin Ultrasound 2008;36:371-3.
 |
 |
 |
 |
 |
| Dr. Marco Bernardes | Dr. Moisés Ventura | Dr. Rita Grazina | Dr. Guido Duarte | Dr. Pedro Canela |
| How to Cite This Article: Bernardes M, Ventura M, Grazina R, Miragaia L, Duarte G, Canela P. Deep Flexor Tendon Entrapment in a Diaphyseal Fracture of the Proximal Phalanx – A Case Report. Journal of Orthopaedic Case Reports 2019 Nov-Dec;9(6):86-89. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com