[box type=”bio”] Learning Point of the Article: [/box]
The ganglion cysts arising from the Hoffa’s fat pad of the knee are an uncommon cause of knee pain and a surgical wide excision of the lesion is curative.
Case Report | Volume 9 | Issue 6 | JOCR November – December 2019 | Page 36-39 | Raju Vaishya, Ankur Kansagra, Amit Kumar Agarwal, Vipul Vijay. DOI: 10.13107/jocr.2019.v09.i06.1578
Authors: Raju Vaishya[1], Ankur Kansagra[1], Amit Kumar Agarwal[1], Vipul Vijay[1]
[1]Department of Orthopaedics, Indraprastha Apollo Hospitals, Sarita Vihar, New Delhi – 110076, India.
Address of Correspondence:
Dr. Amit Kumar Agarwal,
Department of Orthopaedics, Indraprastha Apollo Hospitals, New Delhi – 110076, India.
E-mail: amitorthopgi@yahoo.co.in
Abstract
Introduction: The ganglion cysts are benign fluid-filled sacs, which often arise from a tendon sheath or a joint capsule. Their origin from the fat pad of the knee is rare. Several studies have described intra-articular ganglion cysts in detail; however, extra-articular soft-tissue ganglion cysts have been reported sparingly. We report a rare case of giant ganglion cyst arising from lateral Hoffa’s fat pad (HFP).
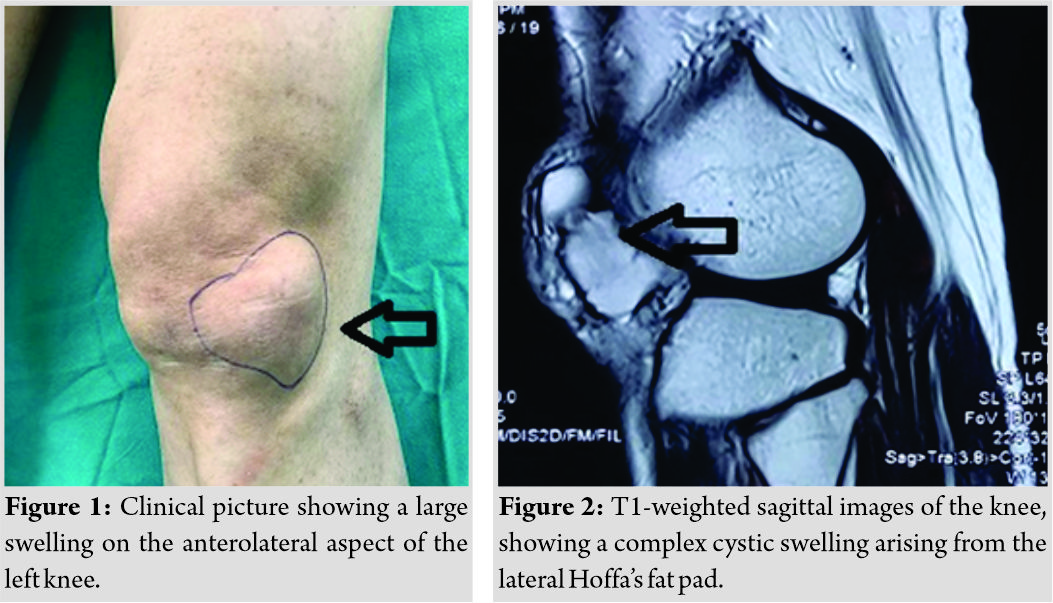
Case Report: A 59-year-old male patient presented with a 3-year history of swelling of the left knee, with occasional pain. There was no history of trauma or any constitutional symptoms. There was an apparent swelling (10 cm ×5 cm in size) around the anterolateral aspect of the knee joint. A magnetic resonance imaging (MRI) scan revealed a multilobular, complex cystic lesion of the lateral HFP. Surgical excision of the cyst was done, and histopathological examination confirmed the diagnosis of the ganglion cyst.
Conclusion: Cysts and cystic-appearing lesions around the knee are not uncommon, but a ganglion cyst arising from HFP is rare. The presence of multipotent cells in the HFP may be responsible for producing a variety of cyst and cyst-like tumors around the anterior aspect of the knee joint. An MRI is the best imaging modality for the diagnosis of these cysts and cysts-like lesions around the knee. We recommend that the smaller intra-articular lesions can be resected arthroscopically, but larger lesions, with extraarticular extension, are best treated by open resection to avoid incomplete excision and recurrence.
Keywords: Knee, ganglion, cyst, arthroscopy, fat pad.
Introduction
The ganglion cysts are benign fluid-filled sacs, which are usually small in size and are most commonly seen around the wrist, hand, and foot but are rarely seen around the elbow [1] and knee as well. They often arise from a tendon sheath or a joint capsule. Their origin from the fat pad of the knee is rare. The ganglion cysts around the knee joint may be classified as (a) intra-articular or extra-articular and (b) soft tissue, periosteal, and intra-osseous ganglion cysts depending on the site of origin. Several studies have described intra-articular ganglion cysts in detail; however, extra-articular soft-tissue ganglion cysts have been reported sparingly. Extra-articular ganglion cysts usually appear as uni- or multi-septate cysts on magnetic resonance imaging (MRI). The infrapatellar Hoffa’s fat pad (HFP) is intracapsular, but anextrasynovial structure can be affected by a variety of pathological conditions such as lipoma, hemangioma, synovial chondromatosis, localized pigmented villonodularsynovitis (PVNS) [2], ganglion cyst, osteochondroma, and chondrosarcoma [3, 4]. Even though the exact function of HFP is not known yet, the involvement of HFP in a variety of tumors and tumor-like conditions has significant clinical implications. We report a rare case of giant ganglion cyst arising from lateral HFP.
Case Report
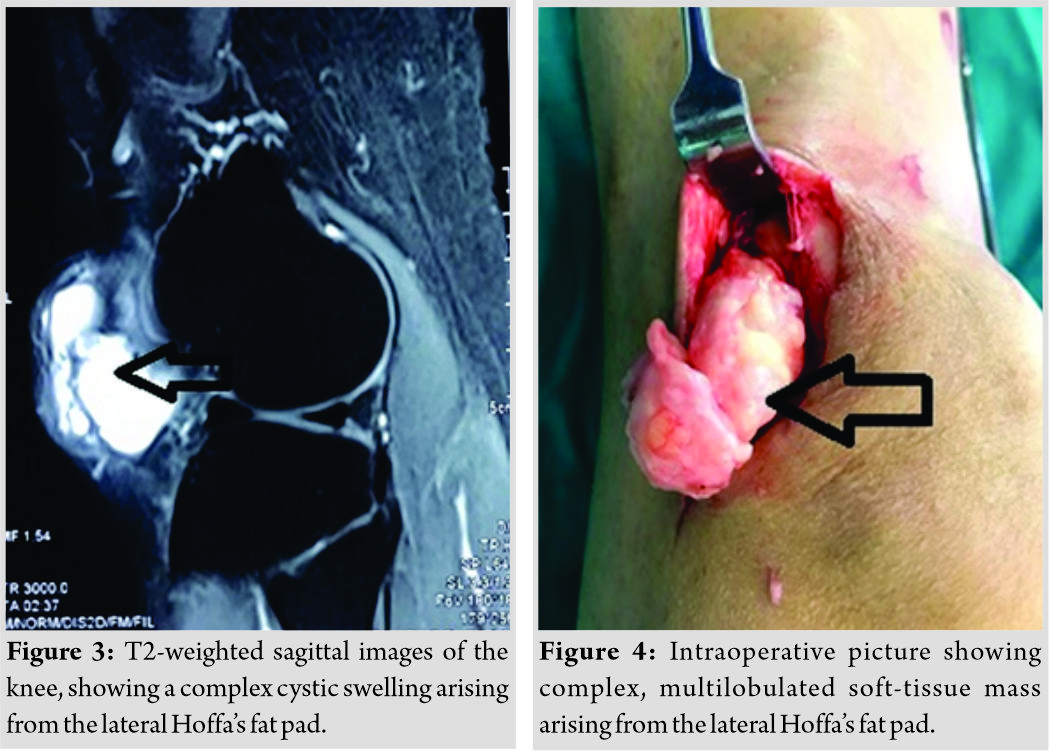
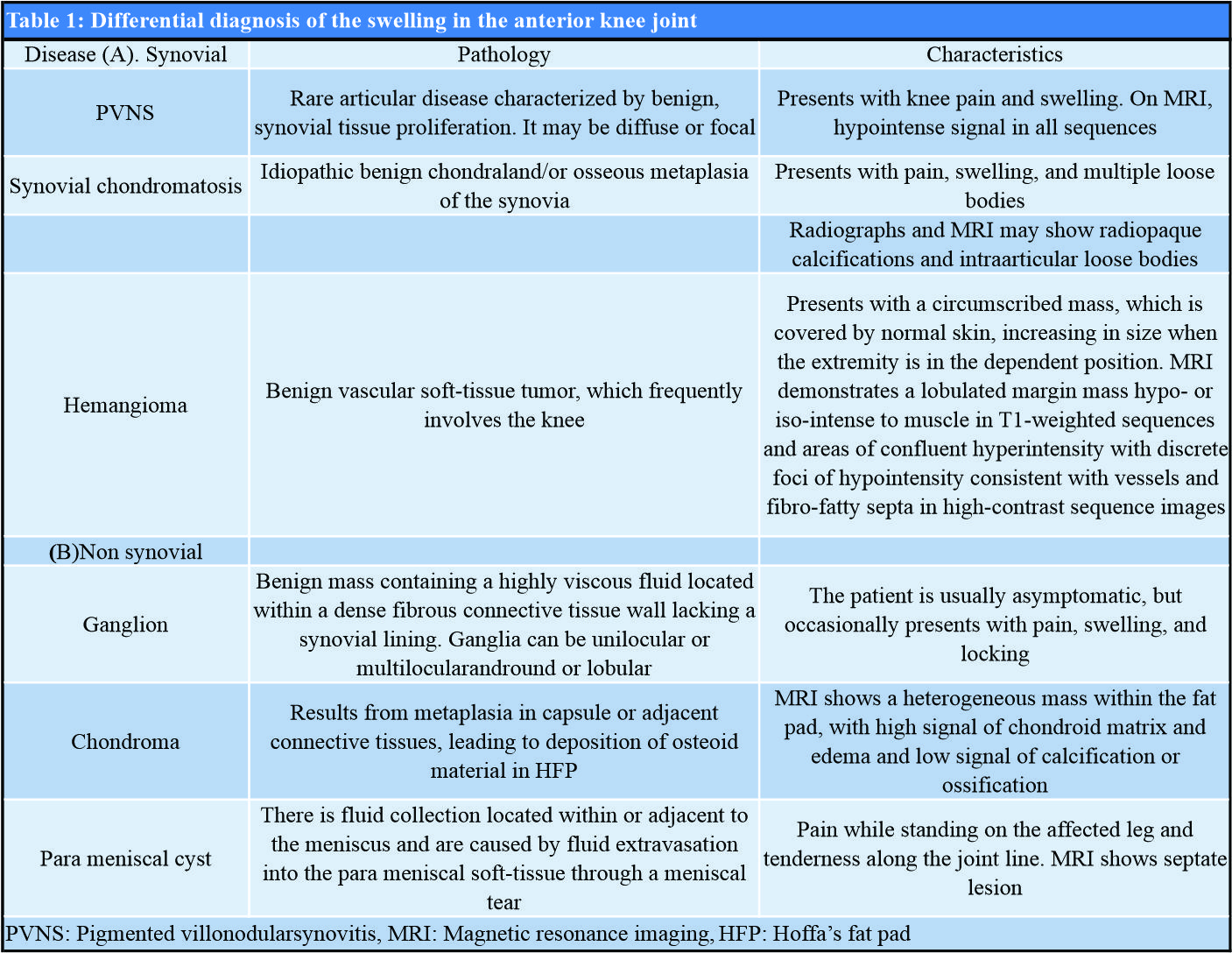
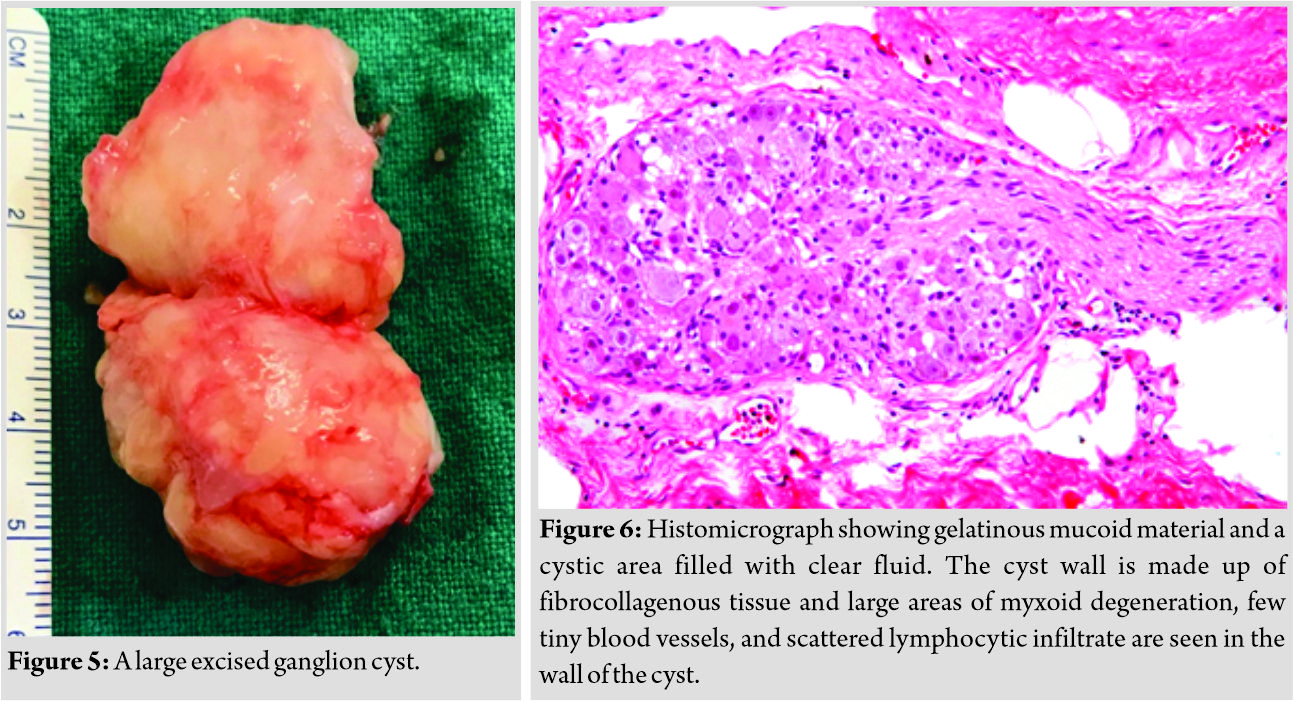
A 59-year-old male patient presented with a 3-year history of swelling of the left knee, with occasional pain. It was gradual in onset and was progressively increasing in size. There was no history of trauma or any constitutional symptoms. There was an apparent swelling (10 cm ×5 cm in size) around the anterolateral aspect of the knee joint (Fig. 1). It was cystic, firm in consistency, non-tender, and not fixed to the overlying skin. The knee had pain-free full range of motion. The plain radiographs were normal. A MRI scan revealed a multilobular, complex cystic lesion of the size of 22 mm × 27 mm × 41mm in the lateral HFP, which was hypointense on T1-weighted and hyperintense on T2-weighted images (Fig. 2 and 3), without any connection with the lateral meniscus. There was no other intraarticular pathology noticed on the MRI scan. This lesion was excised in toto, through an anterolateral incision. A large multilobulated cystic lesion was found coming from lateral HFP through the patellar retinaculum to the subcutaneous tissue (Fig. 4). It was 6 cm × 3 cm in size (Fig. 5). After complete resection of the cyst, the retinaculum was repaired, and the wound was closed in layers. Histopathological examination of the excised mass showed gelatinous mucoid material and a cystic area filled with clear fluid. The cyst wall was made up of fibrocollagenous tissue and lacking any epithelial lining. Large areas of myxoid degeneration, few tiny blood vessels, and scattered lymphocytic infiltrate were observed in the wall of the cyst. These features were consistent with a diagnosis of a ganglion cyst. At 6-month follow-up, there was no sign of recurrence of this swelling, and the patient was asymptomatic with a full range of knee motion.
Discussion
The infrapatellar fat pad (IFP) is also known as HFP. These are intracapsular, but extra synovial structures fill the anterior compartment of the knee. These are richly vascularized and innervated structures. The exact function of these HFP is not known. However, some studies have indicated that these may play a role in the biomechanics of the knee or act as a store for reparative cells after the injury. The HPF of the knee may be affected by a variety of tumors and tumor-like conditions [5]. These include ganglion, localized PVNS, parameniscal cyst, synovial cyst, and chondroma. The differential diagnosis of these similar-looking lesions may be difficult (Table 1), and hence awareness about these entities is crucial in making a right and prompt diagnosis.
It seems that HFP has some peculiar characteristics by which a variety of pathology such as a ganglionic cyst, hemangioma, villonodular synovitis, and chondroma can develop from it. This characteristic feature of the HPF can be attributed to the presence of multipotent stem cells, which can differentiate into other cells such as osteoblasts, chondrocytes, and adipocytes under appropriate conditions in the knee joint. Recently, such cells have been identified in various tissues in the adults (e.g., skin, subcutaneous fat, muscle, and bone marrow). Wickham et al. noted that the cells isolated from the fat pad stroma are different from bone marrow-derived mesenchymal stem cells [6]. Using defined culture conditions, they could induce fat pad-derived stromal cells to differentiate cells with the following phenotypic characteristics: (1) chondrocytes to synthesize cartilage matrix molecules; (2) adipocytes to produce lipid vacuoles and leptin; or (3) osteoblasts to form mineralized tissue. These authors thus supported the hypothesis that multipotent stromal cells are present in many connective tissues and the fat pad may prove to be a potential source of progenitor cells for musculoskeletal tissue engineering.
A variety of benign tumors have been reported to originate from the HFP. These could of synovial or nonsynovial in origin (Table 1). The synovial pathology may be PVNS, synovial osteochondromatosis (Fig. 6), and synovial hemangioma [7]. The nonsynovial pathology includes ganglion cyst, paramensical cysts, andchondroma. The ganglion cysts are benign and contain a highly viscous fluid within a cavity, which is composed of a dense fibrous connective tissue but lacks a synovial lining. These ganglionic cysts may be unilocular or multilocular, round, or lobular. However, communication between ganglia and adjacent joints is uncommon. Ganglia can produce pain and swelling, but they are usually asymptomatic; when symptomatic they may require drainage or excision. A ganglion cyst in the knee joint often arises from the cruciate ligaments, but rarely from the HFP. Only a few case reports of the ganglionic cysts arising from HFP have been reported [8, 9].These cysts are often reported in younger- or middle-aged people, with the presentation of anterior knee pain and swelling around the anteromedial or anterolateral aspect of the knee joint. There may be some restriction of movement and locking of the knee. An MRI is the most useful modality for the diagnosis of ganglion cysts. MRI shows hypointense signals on T1-weighted and hyperintense signals on T2-weighted images [10].
Conclusion
Cysts and cystic-appearing lesions around the knee are not uncommon, but a ganglion cyst arising from HFP is rare. The presence of multipotent cells in the HFP may be responsible for producing a variety of cyst and cyst-like tumors around the anterior aspect of the knee joint. These lesions are usually asymptomatic and are often either not diagnosed or misdiagnosed as meniscal or ligamentous lesions of the knee joint. Awareness about the different swellings arising from the anterior knee joint must be present among the clinician to reach to prompt and accurate diagnosis. A diagnosis of a ganglion cyst can be easily made clinically if it is large. An MRI is the best imaging modality for the diagnosis of these cysts and cysts-like lesions around the knee. We recommend that the smaller intra-articular lesions can be resected arthroscopically, but larger lesions, with extraarticular extension, are best treated by open resection to avoid incomplete excision and recurrence.
Clinical Message
Ganglion cyst arising from HFP is a rare entity that can be diagnosed easily on MRI, and larger lesions, with extraarticular extension, are best treated by open resection to avoid incomplete excision and recurrence.
References
1. Vaishya R, Kapoor C, Agarwal AK, Vijay V.A rare presentation of ganglion cyst of the elbow.Cureus2016;8:e665.
2. Vaishya R, Irfan S. Arthroscopic resection of localized pigmented villonodularsynovitis of the knee. Apollo Med 2012;9:339-42.
3. Vaishya R. Tumor like swellings arising from Hoffa’s fat pad: A report of three patients. Ind J Orthop2012;46:728-9.
4. Sakai H, Tamai K, Iwamoto A, Saotome K. Para-articular chondromaandosteochondroma of the infrapatellar fat pad: A report of three cases. IntOrthop1999;23:114-7.
5. Dean BJ, Reed DW, Matthews JJ, Pandit H, McNally E, Athanasou NA, et al.The management of solitary tumors of Hoffa’s fat pad. Knee 2011;18:67-70.
6. Wickham MQ, Erickson GR, Gimbley JM, Vail P, Guilak F. Multipotent stromal cells derived from the infrapatellar fat pad of the Knee. ClinOrthopRelat Res 2003;412:196-212.
7. Nouri H, Ben Hmida F, OuertataniM,Bouaziz M, Abid L, Jaafoura H, et al. Tumour-like lesions of the infrapatellar fat pad. Knee Surg Sports TraumatolArthrosc2010;18:1391-4.
8. Sloane J, Gulati V, Penna S, Pastides P, Baghla DP. Large intra-articular anterior cruciate ligament ganglion cyst, presenting with inability to flex the knee. Case Rep Med 2010;2010:705919.
9. Schmitz MC, Schaefer B, Bruns J. A ganglion of the anterior horn of the medial meniscus invading the infrapatellar fat pad. Case report. Knee Surg Sports TraumatolArthrosc1996;4:97-9.
10. Amin M, Torreggiani W, Sparkes J. Infrapatellar ganglion that developed from infrapatellar fat and had minimalintraarticular extension. Knee Surg Sports TraumatolArthrosc2008;16:179-81.
11. Bisicchia S, Savarese E. Infra-patellar fat pad cysts: A case report and review of the literature. Muscles Ligaments Tendons J 2013;2:305-8.
12. Yang JH, Kim TS, Lim HC, Kim HJ, Kim YJ, Oh CH, et al. Endoscopic excision of a ganglion cyst in an infrapatellar fat pad extending into the subcutaneous layer. J OrthopSci2012;17:654-8.
13. Saha P, Bandyopadhyay U, Mukhopadhyay AS, Kundu S, Mandal S. Ganglion cyst of knee from Hoffa’s fat pad protruding anterolaterally through retinacular rent: A case report. J Orthop Case Rep 2015;5:69-71.
14. Nikolopoulos I, Krinas G, Kipriadis D, Ilias A, Giannakopoulos A, Kalos S. Large infrapatellar ganglionic cyst of the knee fat pad: A case report and review of the literature. J Med Case Reports 2011;5:351.
15. Ghate SD, Deokar BN, Samant AV, Kale SP. Tumor like swellings arising from Hoffa’s fat pad: A report of three patients. Indian J Orthop2012;46:364-8.
 |
 |
 |
 |
| Dr. Raju Vaishya | Dr. Ankur Kansagra | Dr. Amit Kumar Agarwal | Dr. Vipul Vijay |
| How to Cite This Article: Vaishya R, Kansagra A, Agarwal AK, Vijay V. A Giant Ganglion Cyst Arising from Lateral Hoffa’s Fat Pad of the Knee. Journal of Orthopaedic Case Reports 2019 Nov-Dec;9(6): 36-39. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com