[box type=”bio”] Learning Point of the Article: [/box]
Ankle arthroscopy is a safe and effective technique for the reduction and fixation of selected talar body fractures.
Case Report | Volume 9 | Issue 6 | JOCR November – December 2019 | Page 90-93 | Márcio A Oliveira, Henrique Sousa, Moisés Ventura, José R Oliveira, David Sá, Campos Lemos. DOI: 10.13107/jocr.2019.v09.i06.1604
Authors: Márcio A Oliveira[1], Henrique Sousa[1], Moisés Ventura[1], José R Oliveira[1], David Sá[1], Campos Lemos[1]
[1]Department of Orthopedics, Vila Nova de Gaia/Espinho Hospital Center, Vila Nova de Gaia, Portugal.
Address of Correspondence:
Dr. Márcio A Oliveira,
Department of Orthopedics, Vila Nova de Gaia/Espinho Hospital Center, 4400-129 Dr. Francisco Sá Carneiro Street, Vila Nova de Gaia, Portugal.
E-mail: marcio_oliveira86@hotmail.com
Abstract
Introduction: Arthroscopic-assisted reduction and internal fixation (ARIF) is a recent concept and is increasingly used for articular fractures, due to the minimally invasive nature and high accuracy. However, there are few reports in literature about this procedure in talar fractures.
Case Report: The authors describe a clinical case of a 22-year-old woman with a closed right articular talar neck fracture, Hawkins type II, treated with arthroscopically ARIF.
Conclusion: This is a minimally invasive technique that can allow close accurate reduction and stable fixation of selected articular talar fractures. It avoids some complications of multiple and large incisions of the conventional open surgery, with good functional outcomes and patient satisfaction.
Keywords: Arthroscopy, talar fracture, reduction, fixation.
Introduction
Talar fractures represent 3%–6% of fractures about the foot and ankle [1, 2]. They are a challenging group of fractures with a high rate of complications, namely, avascular necrosis, malunion, non-union, and post-traumatic arthritis [3, 4]. Conservative treatment can lead to a high rate of malunions, with shortening of the medial column, adduction and supination of the forefoot, and poorly tolerated in active patients [5]. Anatomic reduction and fixation of talar fractures may restore the foot shape and function and also diminish the circulatory disorders, preventing non-union, and reducing the incidence of avascular necrosis [6]. It has been achieved through an open medial, lateral, and/or dorsal approaches that can lead to extensive damage to the surrounding soft tissue, contributing to post-operative complications. Arthroscopic-assisted reduction and internal fixation is a recent concept and is increasingly used for certain intra-articular fracture types, due to the minimally invasive nature and high accuracy [7, 8, 9]. The proposal benefits of arthroscopic approach are small incisions, direct visualization of the articular cartilage, the ability to remove incarcerated fragments and debris from joint space, and maintenance of the osseous blood supply by minimizing trauma to the soft tissue envelope. Arthroscopic procedure in the treatment of ankle fractures is well established in literature; however, little information is available concerning to the talar fractures treatment[7,8,10]. On the other hand, some fractures cannot be anatomically reduced by this approach due to their complexity. With this case report, the authors aim to describe the rule of the arthroscopic procedure in selected talar neck fractures and evaluate if the reduction can be maintained and healing achieved with this minimally invasive surgical technique. Similarly, we pretend to evaluate the functional results and the patient satisfaction concerning the return to daily life activities.
Case Report
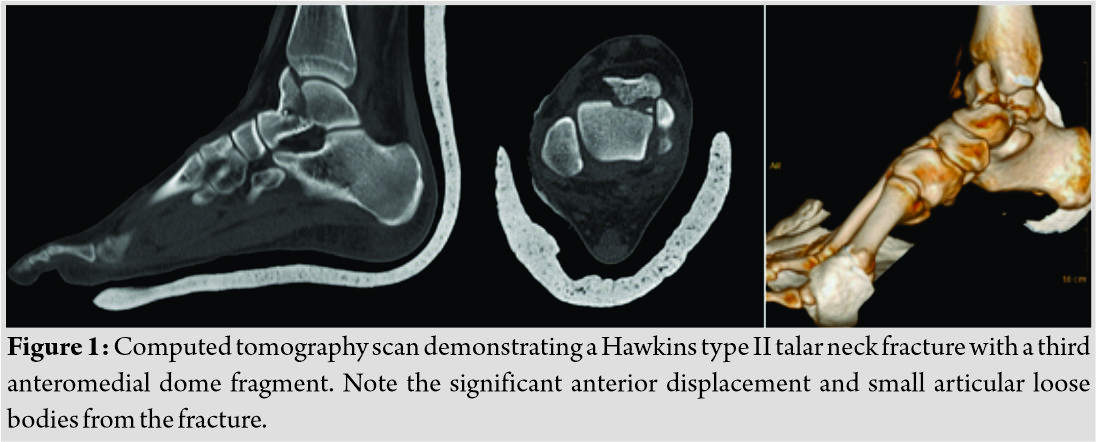
A 22-year-old woman sustained a closed right talar neck fracture, Hawkins type II, after falling from height. A pre-operative study was performed with anteroposterior and lateral ankle X-rays, as well as a computed tomography. There were three major talar fragments including an intermediate anteromedial displaced articular, head, and body (Fig. 1). We performed a temporary posterior leg plaster and symptomatic care with limb elevation until surgery.
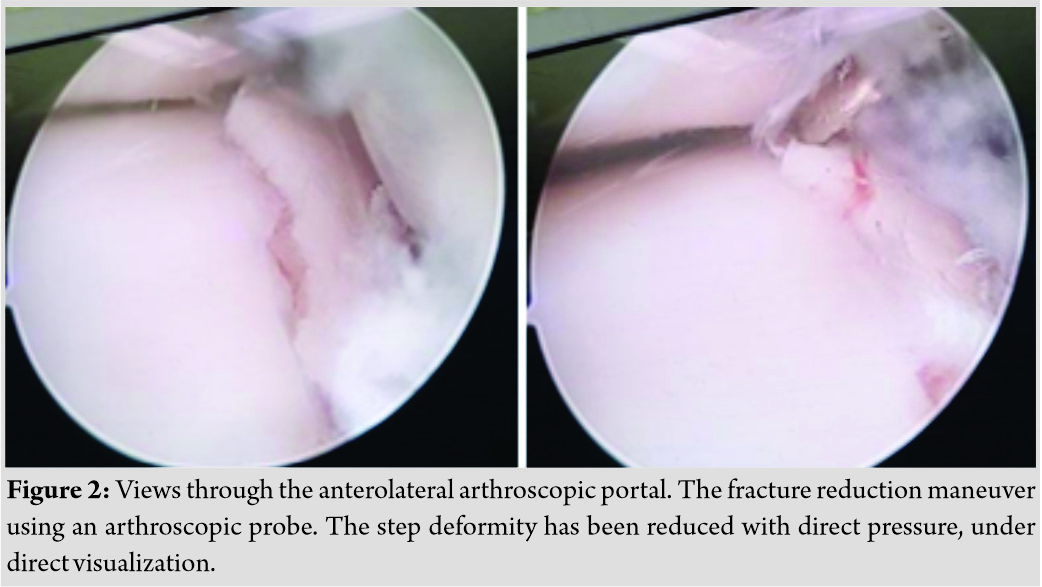
Surgery was performed with the patient supine, with an ipsilateral thigh tourniquet. To preserve the soft tissues and obtain an anatomic reduction, an arthroscopically assisted technique was employed, with a gravity irrigation system, without foot distraction devices. The conventional anterolateral and anteromedial portals were used. As the articular fragment was in anteromedial position, we first performed an anterolateral portal with irrigation and drainage of the fracture hematoma, to visualize directly the fragment with 4.0mm arthroscope. As the fragment was greatly displaced, we did a percutaneous reduction with fluoroscopy control, to achieve a better articular space work. Then, conversion to a minimally invasive approach from anteromedial portal (about 4cm) was performed, allowing to directly maintain the reduction of the intermediate articular fragment, confirm a stepof inferior to 1mm, debride synovium, and remove small articular fragments (Fig. 2).
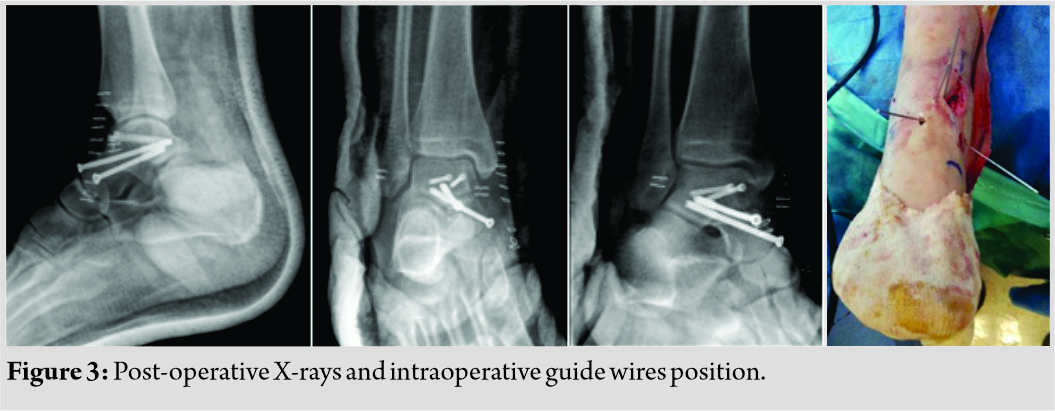
After fluoroscopic evaluation of global talar shape and reduction of the three fragments, provisional fixation with guidewires was performed. First, two 1.6mm guidewires were inserted medial and laterally in the dome articular fragment. Articular insertion site was arthroscopically controlled and directed to the posterior talar process with fluoroscopic control. We checked again the reduction, shape, and length of the talus. Next, another two 2.5mm guidewires were inserted percutaneously under fluoroscopic control, from the talar head into the posterior aspect of talar body to maintain reduction. After drill, two 3.0mm self-drilling self-tapping cannulated headless compression screws (DePuy Synthes) were inserted over the first two guidewires to fix the articular fragment to talar body, with direct visualization of articular screw position. Finally, other two 4.0mm cannulated partial threatened screws (Stryker) were used to complete the fixation (Fig. 3).
We did not identify any other associated injuries, namely, osteochondral or ligament lesions.
The patient was kept non-weight-bearing; the ankle was protected with a posterior splint until stitches were removed in 2 weeks. Then, the patient was allowed to partial weight-bearing with a walker boot and crutches until computed tomography confirms fracture healing at 8 weeks. During this time, the patient was encouraged to do active motion of foot and ankle. Then, walker boot was removed and the patient-initiated partial weight-bearing with crutches, with progression as tolerated. Sports-related rehabilitation started at 6 months.
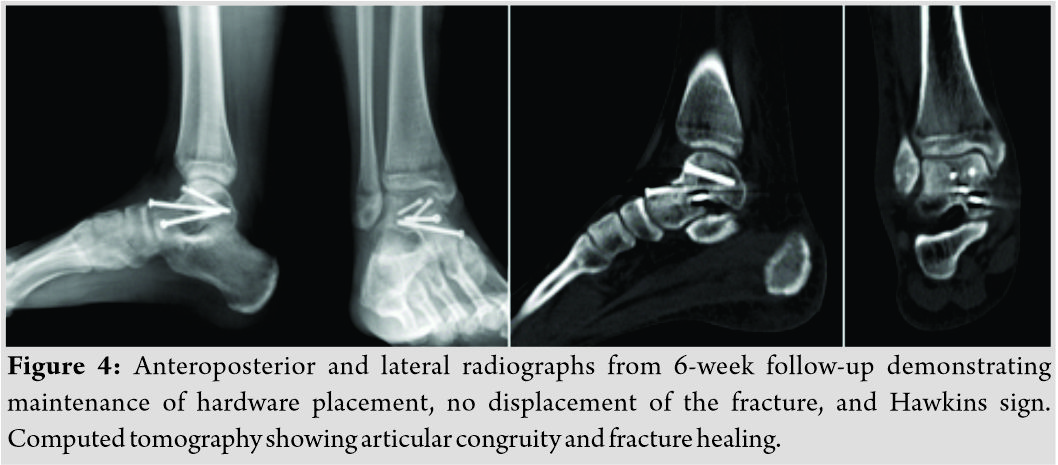
The radiological evaluation at 8 weeks revealed fracture healing with reduction maintained. A positive Hawkins sign was observed, indicative of intact blood supply. No degenerative changes of subtalar or talonavicular joints were observed on radiographs at 6-month follow-up (Fig. 4). At 6-month follow-up, one of the positive findings in clinical evaluation was a slight deficit of strength in supination, 4/5 according to the Medical Research Council scale. The inversion subtalar joint movement was also slightly restricted, compared to contralateral. However, the patient showed an important clinical improvement with rehabilitation program.
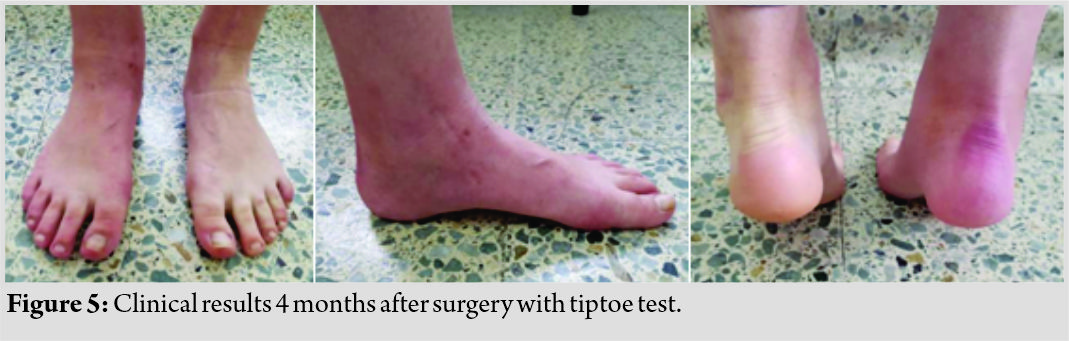
There were no swelling, no tenderness or pain, and no scar-related complaints. No differences in the hindfoot alignment were seen (Fig. 5).
The patient had a visual analog scale of 1 and a foot and ankle outcome score of85% (symptoms and stiffness 86%, pain 89%, function and daily living93%, function, sports, and recreational activities65%, and quality of life subtotal69%).
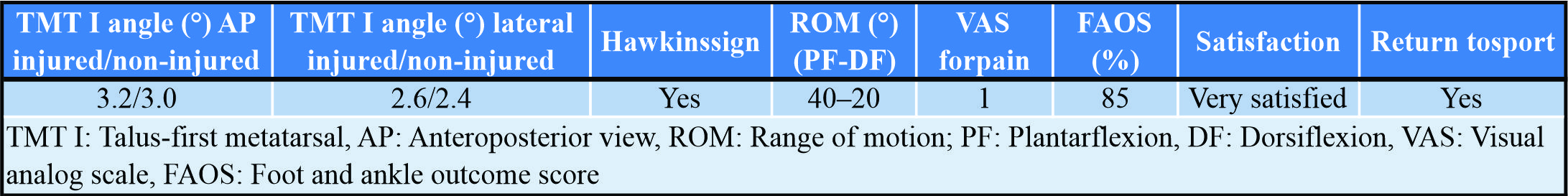
At final follow-up, she started running without complaints and will progress to contact sports activities. At this point, she was very satisfied with the results and motivated to return to pre-injury activity level. No post-operative complications occurred. [Table 1] summarizes the radiological and clinical outcomes at final follow-up.
Discussion
Ankle arthroscopy is increasing regard numerous advantages as diagnostic and treatment. Cadaveric studies have demonstrated the great importance of anatomic reduction of intra-articular talar fractures. They showed an association between an articular displacement >2 mm and a statistically significant alteration of the ankle biomechanics [2]. Thus, we believe that arthroscopy can be very helpful to achieve that objective. It is a powerful tool to assist talus fractures, even with displacement, without great comminution. In our case report, it enabled the direct visualization of articular fracture reduction and fixation, loose bodies removal, exclusion of associated injuries as osteochondral or ligamentar, and preservation of the soft tissue envelope. On the other hand, soft tissue and bone dissection can be considered one possible factor to post-traumatic ankle arthritis[11,12,13]. Thus, we believe that soft tissue trauma associated to open procedure, sometimes with osteotomy for exposure, could have a negative impact in complications and prognosis. Once again, arthroscopy can be a fundamental role to prevent it. Nowadays, there is no consensus about which talar fractures can benefit with arthroscopic-assisted procedure. It has been proposed for two fragment fractures without severe soft tissue damage. Compared to more traditional techniques, where the articular surface is reduced using an image intensifier, arthroscopy has several advantages, namely, the identification and treatment of intra-articular loose bodies, and chondral or osteochondral defects that are radiologically insignificant. Similarly, arthroscopy allows the direct visual control of the reduction and position of the osteosynthesis devices, avoiding implant protruding and malposition. A limitation of this case report is the short-term follow-up. The authors think that it is important to have a second look, with ankle and subtalar arthroscopy at the time of screws removal, after 12-month post-surgery.
Conclusion
With this case report, we show that it is possible to obtain good results in some selected cases beyond the previously mentioned indications, namely, for three fragment articular fractures. Anatomical reduction, soft tissue protection, and good clinical outcomes can be obtained with arthroscopically assisted reduction and fixation of talar neck fractures. It should be considered on a case-by-casebasis. However, arthroscopy does not exclude the fluoroscopic control and even a conversion to a minimally invasive procedure as needed. More research must be performed to evaluate expanded indications for less invasive surgical treatment of talar fractures, with comparison studies of arthroscopic, percutaneous, and open approaches.
Clinical Message
We advocate that ankle arthroscopy is a safe and effective technique for the reduction and fixation of selected talar body fractures. It should be complemented with limited open approach as needed. Its utility can be priceless in talar fractures, regard particular features of bone vascular supply and prevention of associated complications.
References
1. Boack DH, Manegold S. Peripheral talar fractures. Injury 2004;35Suppl 2:SB23-35.
2. Ahn JH, Lee SK, Kim KJ, Kim YI, Choy WS. Subtalar arthroscopic procedures for the treatment of subtalar pathologic conditions: 115 consecutive cases. Orthopaedics2009;32:891.
3. Halvorson JJ, Winter SB, Teasdall RD, Scott AT. Talar neck fractures: A systematic review of the literature. J Foot Ankle Surg 2013;52:56-61.
4. Rammelt S, Zwipp H. Talar neck and body fractures. Injury 2009;40:120-35.
5. Suter T, Barg A, Knupp M, Henninger H, Hintermann B. Surgical technique: Talar neck osteotomy to lengthen the medial column after a malunited talar neck fracture. Clin OrthopRelat Res 2013;471:1356-64.
6. Vallier HA, Reichard SG, Boyd AJ, Moore TA. A new look at the hawkins classification for talar neck fractures: Which features of injury and treatment are predictive of osteonecrosis? J Bone Joint Surg Am 2014;96:192-7.
7. Subairy A, Subramanian K, Geary NP. Arthroscopically assisted internal fixation of a talus body fracture. Injury 2004;35:86-9.
8. Wagener J, Schweizer C, Zwicky L, Horn Lang T, Hintermann B. Arthroscopically assisted fixation of hawkins Type 2 talar neck fracture: A case series. Bone Joint J 2018;100-B:461-7.
9. Pyle C, Harris TG. Arthroscopically assisted percutaneous fixation of a talar neck fracture via posterior approach. Tech Foot Ankle Surg 2018;17:204-8.
10. Bonasia DE, Rossi R, Saltzman CL, Amendola A. The role of arthroscopy in the management of fractures about the ankle. J Am AcadOrthop Surg 2011;19:226-35.
11. Meyer-Wölbert B, Schmidt R, Benesch S, Fels T, Becker HP.Die prognostischebedeutungverletzteranteilebeisprunggelenkfrakturen. Chirurg1999;70:1323-9.
12. Watson JT, Moed BR, Karges DE, Cramer KE.Pilon fractures. Treatment protocol based on severity of soft tissue injury. Clin OrthopRelat Res 2000;375:78-90.
13. Pettrone FA, Gail M, Pee D, Fitzpatrick T, Van Herpe LB. Quantitative criteria for prediction of the results after displaced fracture of the ankle. J Bone Joint Surg Am 1983;65:667-77.
 |
 |
 |
 |
 |
 |
| Dr. Márcio A Oliveira | Dr. Henrique Sousa | Dr. Moisés Ventura | Dr. José R Oliveira | Dr. David Sá | Dr. Campos Lemos |
| How to Cite This Article: Oliveira M A, Sousa H, Ventura M, Oliveira J R, Sá D, Lemos C. Arthroscopically Assisted Reduction and Internal Fixation of Talar Neck Fracture: A Case Report. Journal of Orthopaedic Case Reports 2019 Nov-Dec;9(6): 90-93. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com