[box type=”bio”] Learning Point of the Article: [/box]
This article demonstrates the importance of early recognition and close follow up of Morel-Lavallée lesions.
Case Report | Volume 9 | Issue 6 | JOCR November – December 2019 | Page 15-18 | Megan Mooney, Marshall Gillette, Drew Kostiuk, Maged Hanna, Nabil Ebraheim. DOI: 10.13107/jocr.2019.v09.i06.1568
Authors: Megan Mooney[1], Marshall Gillette[1], Drew Kostiuk[1], Maged Hanna[1], Nabil Ebraheim[1]
[1]Department of Orthopedics, The University of Toledo Medical Center, MS 1094, 3000 Arlington Avenue, Toledo, Ohio 43614, US.
Address of Correspondence:
Dr. Megan Mooney,
Department of Orthopedics, The University of Toledo Medical Center, MS 1094, 3000 Arlington Avenue, Toledo, Ohio 43614, US.
E-mail: megan.mooney2@utoledo.edu
Abstract
Introduction: Morel-Lavallée lesions (MLLs) are a post-traumatic degloving injury which the superficial fascia and skin are separated from the deep fascia through shearing forces. This process leads to the development of a potential space in which blood products and necrotic material can collect, potentially resulting in abscesses, cellulitis, or osteomyelitis. Most of these cases occur at the greater trochanter, gluteal musculature, proximal femur, and around the knee. However, there have been few reports of MLLs occurring in the lumbar region. In this report, we seek to present our experience with a case of a lumbar MLL and outline the diagnostic and operative management utilized.
Case Report: A 48-year-old female presented to our clinic with complaints of persistent low back and swelling 1 month after sustaining a fall from stand resulting in an L5 transverse process fracture. The patient was treated non-operatively but continued to have swelling noted to the lower back. A computed tomography scan demonstrated a large subcutaneous fluid collection measuring 15 cm×16 cm×7 cm centralized over the lower lumbar region. We elected to proceed with operative evacuation of the fluid collection. A 2 cm midline incision over the proximal aspect of the fluid collection was made and approximately 900 ml of serosanguinous fluid was evacuated. The cavity was then irrigated with a normal saline 0.9%/betadine solution and a wound vacuum-assisted closure (VAC) sponge was placed. The post-operative course was unremarkable and the wound VAC was discontinued at the first post-operative visit. The surgical incision went on to heal uneventfully with no signs of infection or fluid reaccumulation.
Conclusion: Although MLLs are rare, clinicians should maintain a high clinical suspicion in patients presenting after blunt trauma injuries with persistent pain, and fluid collections noted on advanced imaging. Conservative management can be initiated if discovered acutely, but if left untreated may require surgical intervention and evacuation of fluid as described in this case.
Keywords: Morel-Lavallée lesion, chronic, lumbar
Introduction
Initially described by French surgeon Maurice Morel-Lavallée in 1853, Morel-Lavallée lesions (MLLs) are a post-traumatic, closed, and degloving injury where skin and superficial fascia become separated from deep fascia as a direct result of shearing forces resulting in the creation of potential space [1, 2, 3]. Blood products and necrotic material can accumulate in this space leading to a chronic inflammatory reaction. If not addressed, the developed space becomes encapsulated and lined by a fibrous capsule containing necrotic material and blood products [4]. Efrimescu et al. have estimated that one to two-thirds of MLL patients is initially misdiagnosed, leading to a delay in treatment [2]. This delay can allow necrotic tissue to act as a nidus for infection resulting in abscesses, cellulitis, or even osteomyelitis [5]. The majority of these lesions are reported to occur at the greater trochanter, gluteal musculature, proximal femur, and around the knee. However, there have been reports of MLLs occurring in the lumbar region [2, 3, 5, 6]. In this report, we seek to present our experience with a case of a lumbar MLL and outline the diagnostic and operative management utilized.
Case Report
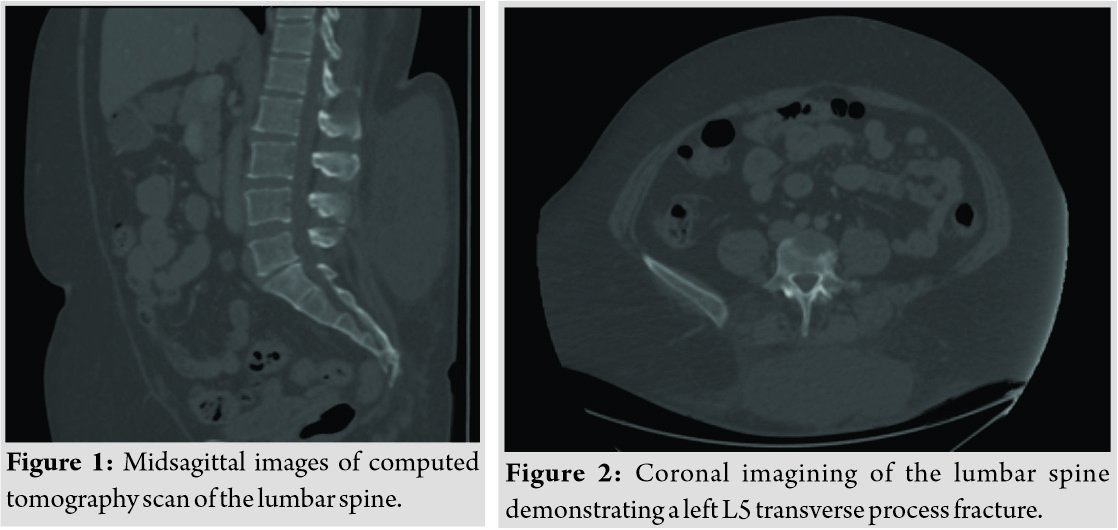
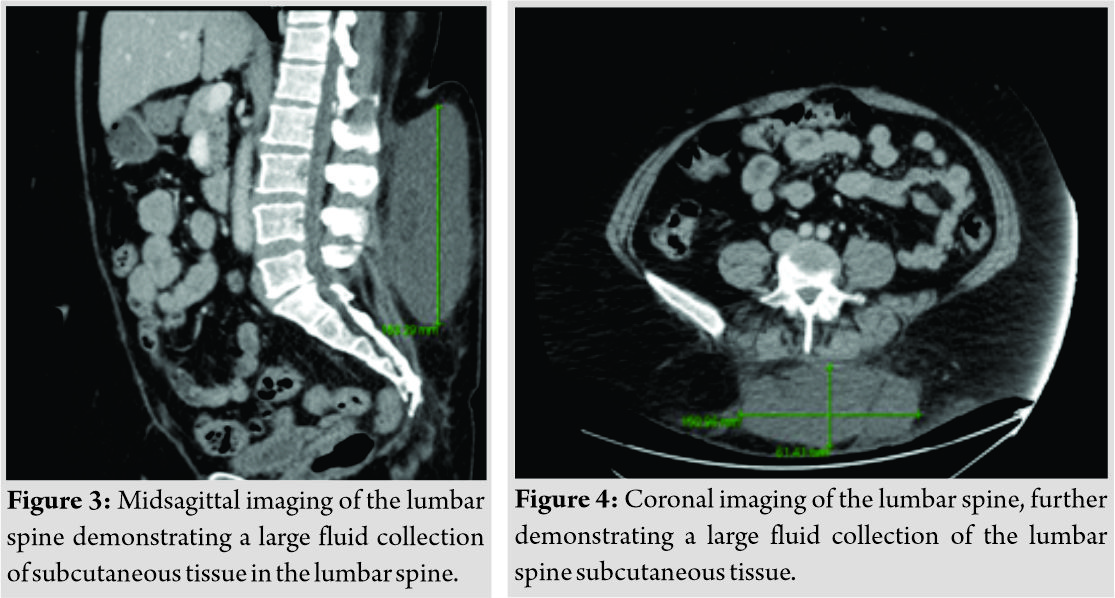
The patient is a 48-year-old female who presented to our institution following a slip and fall on the ice landing directly onto her low back 1 month before presentation. The patient was evaluated at an outside hospital at the time of initial injury where a computed tomography (CT) scan of the lumbar spine was performed. The CT scan of the lumbar spine demonstrated a non-displaced fracture of the left L5 transverse process and a large subcutaneous fluid collection measuring 15 cm×16 cm×7 cm (Fig. 1-4). No additional imaging or laboratory studies were performed and the patient was discharged home.
Upon presentation to our institution, she was complaining of persistent low back swelling that prevented her from sitting or lying on her back comfortably. Physical examination of the patient revealed a large fluctuant mass in the lumbar region, measuring approximately 20 cm×20 cm. No overlying erythema, warmth, or ecchymosis noted. Diffuse tenderness to palpation of the mass was noted. The patient exam was otherwise unremarkable.
The patient was informed of the presence of a persistent fluid collection and given that the patient would likely benefit from operative evacuation, she was offered an open incisional drainage. Treatment options were discussed with the patient and family, and after explaining the risks, benefits, and alternatives to surgery, the patient elected to procedure with surgical irrigation and debridement of the persistent fluid collection. Pre-operative testing was performed with basic laboratory studies; however, no additional imaging studies were obtained. The patient was taken to the operating room 1 week after the initial clinic visit. She received general anesthesia and was placed on the operating table in the right lateral decubitus position. Pre-operative antibiotics, cefazolin 2 g, were given before incision. The patient was prepped and draped in the typical sterile fashion, and a 2 cm midline incision over the proximal aspect of the fluid collection was made that extended through the subcutaneous tissue, opening the superficial fascia. At this time, a large amount of serosanguinous fluid began exuding from the incision. No purulence noted or obvious necrotic tissue. The fluid obtained was sent for culture and cell count. In total 900 ml of serosanguinous fluid was evacuated. On intraoperative examination of the lesion, it was felt that the fluid collection demonstrated a defined walled-off lesion. The cavity was the irrigated with copious amounts of a normal saline 0.9%/betadine solution. A small wound vacuum-assisted closure (VAC) sponge was placed inside the cavity to aid in absorption of any remaining free fluid and to eliminate the present dead space. Negative pressure therapy was then initiated with machine settings at 175 mmHg continuous. The patient recovered well from anesthesia, no complications were encountered and she was transferred to post-anesthesia care unit (PACU) in stable condition. She was discharged home from the PACU and was instructed to continue the wound VAC therapy until her first follow-up appointment in 4 days, at which a wound VAC change will be completed.
At the first post-operative clinic visit, the wound VAC was removed with good wound healing and dead space closing noted. The incision with then closed with 2-0 Novafil under aseptic conditions. The patient reported improvements in her symptoms and no complications at that time. Intraoperative culture results were finalized on post-operative day 5, demonstrating no anaerobic, aerobic, or fungal growth. The 2-week post-operative visit demonstrated a well healing surgical incision with no evidence of infection or drainage. The patient stated that she was now able to comfortably lay and sit down.
Discussion
MLLs, though rarely seen, are a product of blunt trauma in which high energy shearing forces induce separation of the skin and subcutaneous tissues from solid underlying fascia generating a potential space. The vascular and lymphatic vessels that travel through the hypodermis then drain into the newly formed potential space eventually leading to a collection of blood, lymph, and necrotic fat. Inflammatory and metabolic products within the fluid then potentiate cellular permeability and further exacerbate leakage into the created space [7, 8, 9, ]. This fluid then becomes surrounded by granular tissue, which may result in the formation of a fibrous pseudocapsule, prevention of fluid resorption, and predilection toward bacterial infection [10, 11, 12]. The formation of the capsule itself is related to lack of fluid evacuation in the acute phase of the condition, which may be achieved with prompt compression [14]. When this does not occur, there is a subsequent inflammatory reaction, which may result in capsular formation [13, 14]. Due to the risk of infectious complications, early diagnosis is paramount to ensuring that patients receive the necessary treatment. The condition itself is primarily a clinical diagnosis; however, symptoms such as skin hypermobility and loss of cutaneous sensation over the affected area may be noted, and help develop an index of suspicion [4, 5]. Once a MLL is suspected, further imaging studies are necessary to confirm the diagnosis. Although CT scans have been used in the past as the primary study for evaluation of these lesions, especially in acute trauma cases, they demonstrate several drawbacks. CT imagining does not readily allow soft tissue characterization in comparison to that of MRI and poses a significant radiation risk [15]. At present, the imaging modality of choice is MRI due to excellent soft tissue evaluation, high contrast resolution, multiplanar acquisition, and greater anatomic details [4, 16, 17]. However, in the case presented, the size and easily palpable location of the fluid collection and its appearance on CT imaging did not necessitate further imaging to aid in a diagnosis. At present, there is no established consensus on the treatment methods for MLLs as the condition is a relatively rare [4, 5]. In patients with acute, small lesions without underlying fractures, the first-line therapy is suggested to be as simple as a compression bandage, anti-inflammatory therapy, and bed rest [18]. Regarding the even less commonly reported cases of lumbar MLL, Zairi et al. performed a review of all cases documenting the condition and the outcomes reported [5]. They noted that for patients who do not respond to conservative management and needle aspiration can be performed. However, concerns for recurrence should be present if the lesion is particularly large [5]. As in the aforementioned case, operative incision and drainage was performed due to the chronicity and size of the lesion, which was felt to have a high likelihood of recurrence if not completed evacuated; however, there are few reports in literature to support the treatment of chronic MLL management. Another therapeutic option for those not responding to conservative treatment is sclerotherapy [4, 5, 18]. The object of sclerotherapy in this avenue is to eliminate the potential space in which fluid accumulates [19]. A variety of agents has been utilized for this procedure; including talc, bleomycin, tetracycline, and erythromycin though none of these are considered to be ideal agents [19, 20, 21]. Recently, doxycycline was also evaluated for its efficacy in sclerotherapy and was discovered to be safe, effective, and inexpensive in comparison to other agents and may even be a suitable substitute for open debridement in the case of chronic lesions [22]. When these methods prove unsuccessful, or the condition is diagnosed late, as in the case presented, operative management remains the mainstay of treatment as it allows for the relief of symptoms and mitigates the risk of infectious complications [5].
Conclusion
Although MLLs are rare, clinicians should maintain a high suspicion in patients presenting after blunt trauma injuries with persistent pain and fluid collections noted on advanced imaging. Conservative management can be initiated if discovered acutely, but if left untreated may require surgical intervention as described in this case.
Clinical Message
The aforementioned case report highlights the importance of maintaining a high clinical suspicion for a Morel-Lavallée lesion given the mechanism with careful and close follow up to detect rare, but potential complications.
References
1. Kumar Y, Hooda K, Lo L, Karol I. Morel-Lavallée lesion: A Case of an American football injury. Conn Med 2015;79:477-8.
2. Efrimescu CI, McAndrew J, Bitzidis A. Acute lumbar Morel-Lavallee haematoma in a 14-year-old boy. Emerg Med J 2012;29:433.
3. Moran DE, Napier NA, Kavanagh EC. Lumbar Morel-Lavallée effusion. Spine J 2012;12:1165-6.
4. Diviti S, Gupta N, Hooda K, Sharma K, Lo L. Morel-Lavallee lesions-review of pathophysiology, clinical findings, imaging findings and management. J Clin Diagn Res 2017;11:TE01-4.
5. Zairi F, Wang Z, Shedid D, Boubez G, Sunna T. Lumbar Morel-Lavallée lesion: Case report and review of the literature. Orthop Traumatol Surg Res 2016;102:525-7.
6. Sawkar AA, Swischuk LE, Jadhav SP. Morel-Lavallee seroma: A review of two cases in the lumbar region in the adolescent. Emerg Radiol 2011;18:495-8.
7. Palacio EP, Di Stasi GG, Lima EH, Mizobuchi RR, Júnior AD, Galbiatti JA, et al. Results from surgical treatment of Morel-Lavallée lesions: Prospective cohort study. Rev Bras Ortop 2015;50:148-52.
8. Gwinn DE, Morgan RA, Kumar AR. Gluteus maximus avulsion and closed degloving lesion associated with a thoracolumbar burst fracture. A case report. J Bone Joint Surg Am 2007;89:408-12.
9. Hak DJ, Olson SA, Matta JM. Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: The Morel-Lavallée lesion. J Trauma 1997;42:1046-51.
10. Collinge C, Tornetta P 3rd. Soft tissue injuries associated with pelvic fractures. Orthop Clin North Am 2004;35:451-6, 5. Wood GW. General principles of fracture treatment. In: Canale ST, Beaty JH, editors. Campbell’s Operative Orthopaedics. 11th ed. Philadelphia, PA: Mosby Elsevier; 2008. p. 3032-5.
11. Harma A, Inan M, Ertem K. The Morel-Lavallée lesion: A conservative approach to closed degloving injuries. Acta Orthop Traumatol Turc 2004;38:270-3.
12. McKenzie GA, Niederhauser BD, Collins MS, Howe BM. CT characteristics of Morel-Lavallée lesions: An under-recognized but significant finding in acute trauma imaging. Skeletal Radiol 2016;45:1053-60.
13. Bonilla-Yoon I, Masih S, Patel DB, White EA, Levine BD, Chow K, et al. The Morel-Lavallée lesion: Pathophysiology, clinical presentation, imaging features, and treatment options. Emerg Radiol 2014;21:35-43.
14. Moriarty JM, Borrero CG, Kavanagh EC. A rare cause of calf swelling: The Morel-Lavallee lesion. Ir J Med Sci 2011;180:265-8.
15. Mellado JM, Pérez del Palomar L, Díaz L, Ramos A, Saurí A. Long-standing Morel-Lavallée lesions of the trochanteric region and proximal thigh: MRI features in five patients. AJR Am J Roentgenol 2004;182:1289-94.
16. Mellado JM, Bencardino JT. Morel-Lavallée lesion: Review with emphasis on MR imaging. Magn Reson Imaging Clin N Am 2005;13:775-82.
17. Tejwani SG, Cohen SB, Bradley JP. Management of Morel-Lavallee lesion of the knee: Twenty-seven cases in the national football league. Am J Sports Med 2007;35:1162-7.
18. Isaacson AJ, Stavas JM. Image-guided drainage and sclerodesis of a Morel-Lavallee lesion. J Vasc Interv Radiol 2013;24:605-6.
19. Luria S, Applbaum Y, Weil Y, Liebergall M, Peyser A. Talc sclerodhesis of persistent Morel-Lavallée lesions (posttraumatic pseudocysts): Case report of 4 patients. J Orthop Trauma 2006;20:435-8.
20. Davis S, Rambotti P, Grignani F. Intrapericardial tetracycline sclerosis in the treatment of malignant pericardial effusion: An analysis of thirty-three cases. J Clin Oncol 1984;2:631-6.
21. Haddad FJ, Younes RN, Gross JL, Deheinzelin D. Pleurodesis in patients with malignant pleural effusions: Talc slurry or bleomycin? Results of a prospective randomized trial. World J Surg 2004;28:749-53.
22. Bansal A, Bhatia N, Singh A, Singh AK. Doxycycline sclerodesis as a treatment option for persistent Morel-Lavallée lesions. Injury 2013;44:66-9.
 |
 |
 |
 |
 |
| Dr. Megan Mooney | Dr. Marshall Gillette | Dr. Drew Kostiuk | Dr. Maged Hanna | Dr. Nabil Ebraheim |
| How to Cite This Article: Mooney M, Gillette M, Kostiuk D, Hanna M, Ebraheim N. Surgical Treatment of a Chronic Morel-Lavallée Lesion: A Case Report. Journal of Orthopaedic Case Reports 2019 Nov-Dec;9(6): 15-18. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com