[box type=”bio”] Learning Point of the Article: [/box]
Cemented hip arthroplasty is an efficient option to reconstruct the hip anatomyin a patient suffering from combined achondroplasia and hereditary multiple exostosis syndromes.
Case Report | Volume 9 | Issue 6 | JOCR November – December 2019 | Page 32-35 | E Kenanidis, G Paparoidamis, N Garantziotis, P Kakoulidis, M Potoupnis, E Tsiridis. DOI: 10.13107/jocr.2019.v09.i06.1576
Authors: E Kenanidis[1], G Paparoidamis[1], N Garantziotis[1], P Kakoulidis[1], M Potoupnis[1], E Tsiridis[1]
[1]Department of Orthopaedic, Academic Orthopaedic Unit, Papageorgiou General Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece.
Address of Correspondence:
Dr. Eustathios Kenanidis,
Department of Orthopaedic, Academic Orthopaedic Unit, Papageorgiou General Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece.
E-mail: stathiskenanidis@gmail.com
Abstract
Introduction: Combined achondroplasia and hereditary multiple exostosis (HME) syndrome is a rare autosomal dominant inherited skeletal dysplasia. We report, for the 1sttime, a complex primary hip arthroplasty in a patient with combined achondroplasia and HME syndrome. We emphasize to the femoral and acetabular surgical concerns and difficulties of the surgical exposure and soft tissue balancing for this complex procedure.
Case Report: An ambulatory 66-year-old female Caucasian with achondroplasia and HME presented with the left hip pain, progressive walk disability and limited range of hip motion due to severe hip osteoarthritis. Full cemented primary total hip arthroplasty (THA) with an impaction grafting technique was performed; posterior lip augmentation device was implanted to improve stability. At 5 years follow-up, the patient remains ambulatory and pain-free with improved range of hip motion. No signs of aseptic loosening are present.
Conclusions: Cemented THA could be an efficient option to reconstruct the complex hip anatomy in patients with skeletal dysplasia.
Keywords: Total hip arthroplasty, hereditary multiple exostosis, achondroplasia.
Introduction
Achondroplasia is the most common form of disproportionate dwarfism [1]. This autosomal dominant inherited disease is attributed to spontaneous mutations of fibroblast growth factor receptor 3 [1]. The syndrome is typically characterized by short stature with disproportionate shortening of the limbs, large head with frontal bossing and hypoplastic midface and marked joint deformities. The metaphyseal irregularities of hip and knee, abnormalities of the vertebrae and pelvis with small and square iliac wings are the most common radiological findings [2]. Hereditary multiple exostosis (HME) is another common autosomal dominant inherited skeletal dysplasia. Mutations in the exostosin 1–3 genes [3] and other EXT-like genes have been implicated as causing genes [4]. The variable skeletal deformities are mainly attributed to the development of multiple exostoses at the metaphyses of long bones [5, 6]. These are the short stature, leg length discrepancy, valgus knee and ankle deformity, asymmetry of the pectoral, and pelvic girdles [7, 8]. Periacetabular and femoral exostoses can cause hip osteoarthritis, coxa valga, increased neck-shaft angle, etc. [9]. The combined achondroplasia and HME dysplasia syndrome are rarely reported in the literature [10]. Total hip arthroplasty (THA) in patients suffering either from achondroplasia or HME is a complex primary hip arthroplasty with a high rate of complications and difficulties [11]. This article aims to present for the 1sttime the technical considerations of performing a complex primary THA in a rare case of Caucasian women who suffered from combined achondroplasia and HME syndromes.
Case Report
An ambulatory 66-year-old female Caucasian (149 cm/76 kg) with achondroplasia and HME presented with left hip pain and progressive walk disability. On physical examination, she had a painful and limited range of left hip motion. She achieved 45° of hip flexion, 0° of internal and 5°of external rotation, and 0°–5° of abduction and adduction. The flexion contracture of the hip was 5°. The Harris hip score (HHS) was 42. The left lower limb was 2 cm lower than the right. The patient also suffered from osteoporosis and depression.
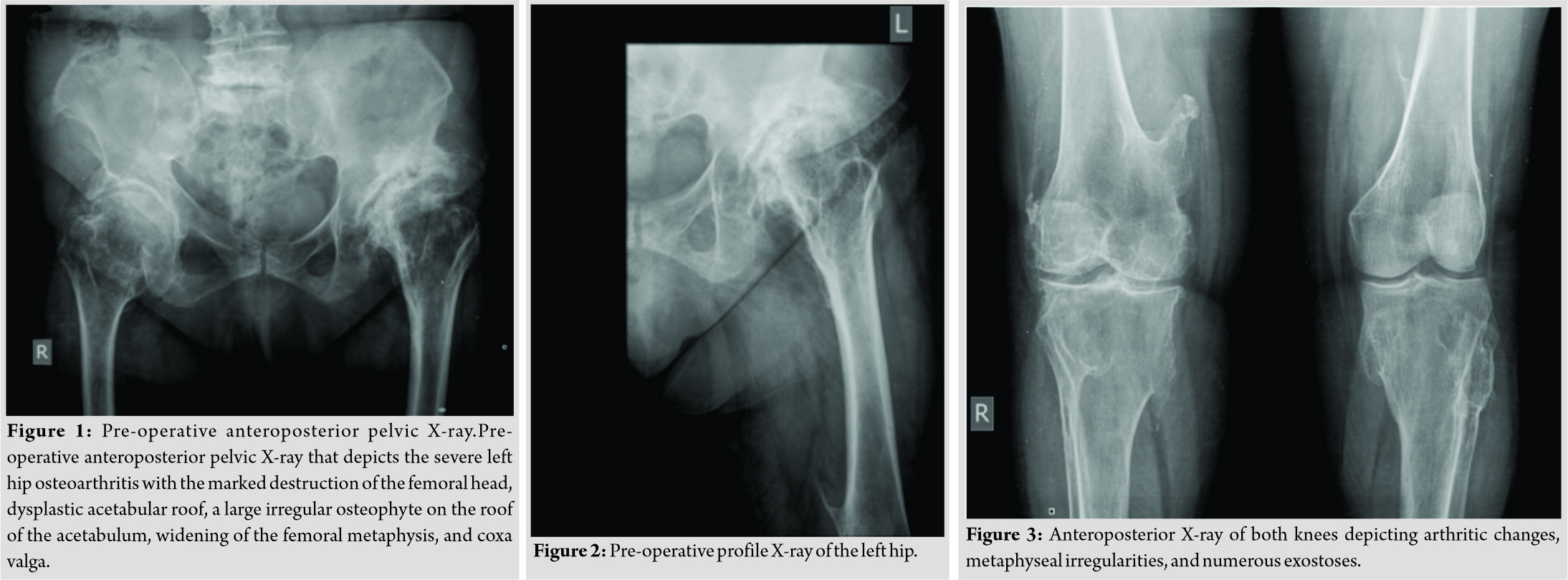
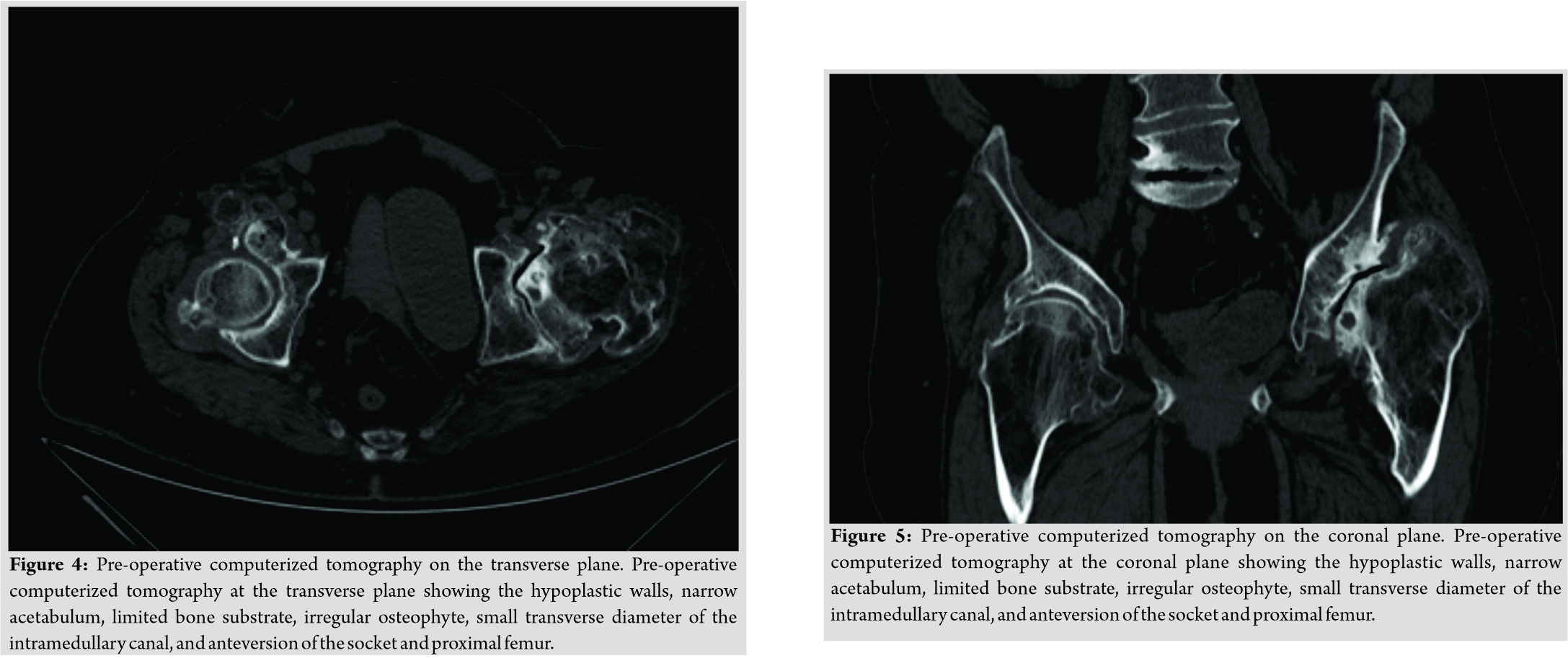
Her radiograph revealed severe hip osteoarthritis with the marked destruction of the femoral head, dysplastic acetabular roof, limited acetabular inclination, a large irregular osteophyte on the roof of the acetabulum, widening of the femoral metaphysis, and coxa valga (Fig. 1, 2, 3). A pre-operative computerized tomography showed the hypoplastic anterior wall, narrow acetabulum, limited bone substrate, the large irregular osteophyte from the femoral head, and the small transverse diameter of the intramedullary canal. The socket, femoral neck, and proximal femur were anteverted (Fig. 4 and 5). Pre-operative planning demonstrated that cemented implants had sufficient structural stability compared to non-modular uncemented under these geometric conditions.
She subsequently underwent a left THA through a posterior approach. The approach was hampered by the capsule that was densely adherent to the underlying bone and the large exostosis that was hard to remove. On the acetabular side, the anterior wall insufficiency and the limited bone substrate made the use of a cementless cup implant impossible. The dysplastic acetabular roof was reconstructed with an impaction grafting technique. The anterior and posterior columns of the acetabulum were adequately exposed, and the teardrop and the margins of the defect were identified. Careful acetabular reaming promoted the bleeding of the host bone surface to assist the incorporation of the bone graft. We reconstructed the uncontained to contained defect with the use of a ceiling mesh. We trimmed a rim mesh appropriately to fit using an impactor as a guide to its final location and secured the mesh with several screws placed around the margin. The autologous femoral head was sectioned into chips and vigorously impacted to provide a “cobblestone looking” bed following impaction. We washed gingerly the grafted bed as preparing for proper cementing technique. Third generation cementing technique was then performed including drying of the bed, creation of peg holes, retrograde cement insertion, pressurization for 3–5 min against the bed, insertion of the standard polyethylene cup (Stryker, Exeter, X3, RimFit, 46mm), and continuous pressurization into the adjusted position until cement setting.
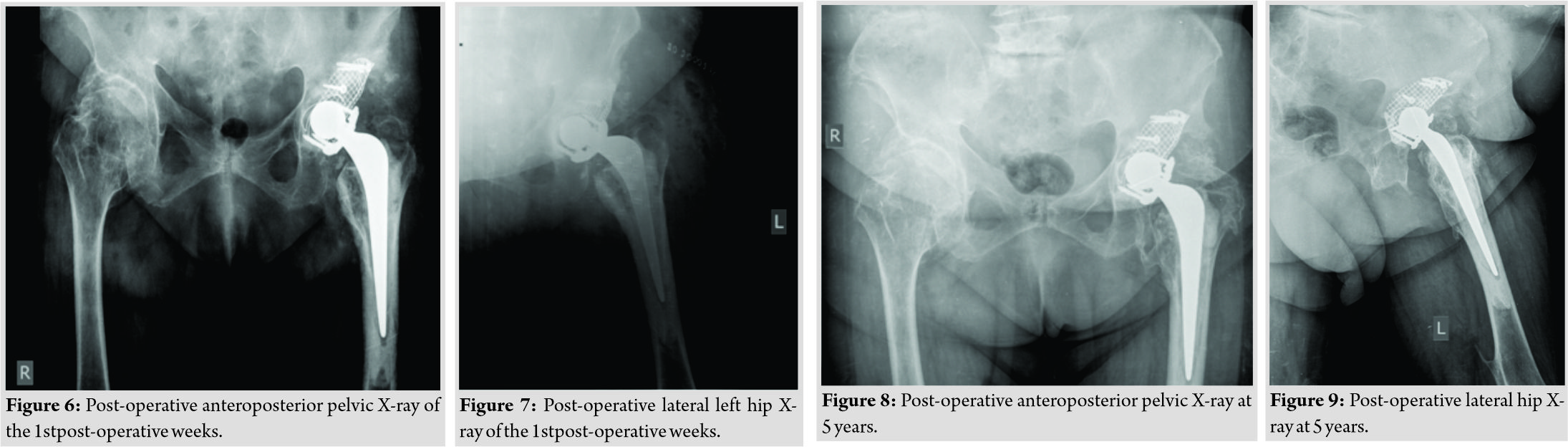
On the femoral side, an extensive metaphyseal flare followed immediately by a narrow medullary canal existed. This was managed with a cemented stem (Stryker, Exeter V40, No 2, Offset 44) with a metallic head (Stryker, Exeter V40, 28mm) that engaged the diaphysis. The stem was fixed with Palacos cement (Palacos, Heraeus) and a third-generation cementation technique. Lack of abductors, ossification of the gluteus medius, and part of the minimus caused instability. An additional posterior lip augmentation device (PLAD) (DePuy International Limited, Leeds, United Kingdom) was then implanted into the posterior rim of the polyethylene to improve stability. Post-operative radiographs showed that the THA components were well aligned (Fig. 6 and 7). Both legs were identical in length. Postoperatively, the patient was mobilized with partial weight-bearing for 8 weeks and then as tolerated. Her pain and post-operative range of motion had significantly improved. Her recovery was uneventful following the surgery. Follow-up is now at 5 years (Fig. 8 and 9). Her HHS is 82. She has painless and unlimited walking ability. She achieves 70° of hip flexion, 5° of internal and external rotation, and 10° of abduction and adduction. There are no signs or symptoms of loosening with an adequate osseous integration of the autogenous grafts at the acetabulum; heterotopic ossification of gluteus medius was developed.
Discussion
To the best of our knowledge, this is the first reported THA in a patient suffering from combined achondroplasia and HME syndrome. We report the femoral and acetabular surgical concerns as well as difficulties of surgical exposure and soft tissue balancing for this complex primary THA. The distorted anatomy of the hip was the reason for the increased reported rate of complications following THA in patients with achondroplasia or HME. Wade et al. [11] reported perforation of the proximal femur in two patients with achondroplasia and secondary osteoarthritis undergoing cemented THA. This was mainly attributed to the abnormal proximal femoral anatomy and the difficult exposure. Femoral perforation was revealed postoperatively and managed with revision THA [11]. The bony deformities of this skeletal syndrome and patients’ age necessitate an individualized, case-by-case component selection for this complex primary THA [3]. Uncemented non-modular or modular and custom made or cemented are the stem choices [3, 12, 13]. Moran et al. used uncemented modular proximal femoral replacing THA in two patients with hip dysplasia secondary to HME due to the poor bone quality of metaphysis and the disease severity. Mefsin et al. used fully coated diaphyseal engaging stem in a patient with HME and hip arthritis due to the wide metaphysis and the metaphyseal-diaphyseal mismatch. In our case, the anatomic variations of the proximal femur, namely the increased anteversion, metaphyseal flaring, and short diameter of the medullary canal were the main surgical concerns. The proximal femoral anatomy and the age of the patient with poor bone quality led us to use a cemented stem with no complications. The versatility of this stem to sit as it fits an irregular canal, the ability to correct the femoral anteversion and several stem choices to fix the offset are other undoubtful advantages of the cemented stem. On the acetabular side, the limited bone substrate, the reduced size of the bony structures, and acetabular dysplasia were the main surgical concerns. Wirtz et al. [13] presented a case of a patient with achondroplasia who was treated successfully with cemented THA. The abnormal acetabular columns made the use of uncemented cup impossible. In our case, the cemented acetabular impaction grafting (AIG) was chosen to reconstruct the dysplastic acetabular roof. AIG is an established, technically demanding but reproducible technique with good published results [14]. AIG can correct cavitary and segmental defects, restore acetabular anatomy, recreate the correct hip rotation center,and replace the acetabular bone stock, a particular advantage in the younger patient. Soft tissue balancing and the risk of dislocation are further surgical difficulties. Vaishya et al. [15] reported dislocation of the right hip uncemented arthroplasty of a patient suffering from hip osteoarthritis due to HME. Open reduction combined with a revision of THA with a longer stem was followed. In our case, an additional PLAD was implanted into the posterior rim of the polyethylene to improve stability.
Conclusion
The unique features of this advanced surgery in a patient suffering from combined achondroplasia and HME were reported for the 1sttime. Cemented hip arthroplasty was an efficient option to reconstruct the hip anatomy offering a good clinical result at midterm.
Clinical Message
Cemented hip arthroplasty was effective for reconstructing hip osteoarthritis in a patient suffering from combined achondroplasia and HME syndromes with an excellent clinical result at midterm. A comprehensive preoperative plan and knowledge of the anatomic alterations of the patient were essential to overcome the technical difficulties.
References
1. Wang Y, Liu Z, Liu Z, Zhao H, Zhou X, Cui Y, et al. Advances in research on and diagnosis and treatment of achondroplasia in China. Intractable Rare Dis Res 2013;2:45-50.
2. Laederich MB, Horton WA. FGFR3 targeting strategies for achondroplasia. Expert Rev Mol Med 2012;14:e11.
3. Mesfin A, Goddard MS, Tuakli-Wosornu YA, Khanuja HS. Total hip and knee arthroplasty in patients with hereditary multiple exostoses. Orthopedics 2012;35:e1807-10.
4. Guo XL, Deng Y, Liu HG. Clinical characteristics of hereditary multiple exostoses: A retrospective study of mainland Chinese cases in recent 23 years. J Huazhong Univ Sci Technolog Med Sci 2014;34:42-50.
5. Hennekam RC. Hereditary multiple exostoses. J Med Genet 1991;28:262-6.
6. Schmale GA, Conrad EU 3rd, Raskind WH. The natural history of hereditary multiple exostoses. J Bone Joint Surg Am 1994;76:986-92.
7. Staal HM, Witlox AM, Mooij DT, Emans PJ, Ham JS, van Rhijn LW, et al. Current knowledge on exostoses formation in hereditary multiple exostoses: Where do exostoses originate and in what way is their growth regulated? Hereditary Genet 2014;3:134.
8. Goud AL, de Lange J, Scholtes VA, Bulstra SK, Ham SJ. Pain, physical and social functioning, and quality of life in individuals with multiple hereditary exostoses in the Netherlands: A national cohort study. J Bone Joint Surg Am 2012;94:1013-20.
9. Porter DE, Benson MK, Hosney GA. The hip in hereditary multiple exostoses. J Bone Joint Surg Br 2001;83:988-95.
10. Dominguez R, Young LW, Steele MW, Girdany BR. Multiple exostotic hypochondroplasia: Syndrome of combined hypochondroplasia and multiple exostoses. PediatrRadiol1984;14:356-9.
11. Wade FA, Parvizi J, Sharkey PF, Purtill JJ, Hozack WJ. Femoral perforation complicating contemporary uncemented hip arthroplasty. J Arthroplasty 2006;21:452-5.
12. Moran M, Krieg AH, Boyle RA, Stalley PD. Bilateral total hip arthroplasty in severe hereditary multiple exostosis: A report of two cases. Hip Int 2009;19:279-82.
13. Wirtz DC, Birnbaum K, Siebert CH, Heller KD. Bilateral total hip replacement in pseudoachondroplasia. Acta OrthopBelg2000;66:405-8.
14. Petheram TG, Howell JR. The exeter method-acetabular impaction grafting with cemented reimplantation. OperOrthopTraumatol2014;26:114-25.
15. Vaishya R, Swami S, Vijay V, Vaish A. Bilateral total hip arthroplasty in a young man with hereditary multiple exostoses. BMJ Case Rep 2015;2015:bcr2014207853.
 |
 |
 |
 |
 |
 |
| Dr. E Kenanidis | Dr. G Paparoidamis | Dr. N Garantziotis | Dr. P Kakoulidis | Dr. M Potoupnis | Dr. E Tsiridis |
| How to Cite This Article: Kenanidis E, Paparoidamis G, Garantziotis N, Kakoulidis P, Potoupnis M, Tsiridis E. Technical Considerations of Complex Primary Total Hip Arthroplasty in a Rare Case of Combined Achondroplasia and Hereditary Multiple Exostosis Syndromes. Journal of Orthopaedic Case Reports 2019 Nov-Dec;9(6): 32-35. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com