[box type=”bio”] Learning Point of the Article: [/box]
Peri-implant subtrochanteric fractures following neck of femur fractures treated with cancellous screws are surgically challenging and a robust system of evaluating such fractures and decision-making aids perioperative planning.
Case Report | Volume 9 | Issue 6 | JOCR November – December 2019 | Page 44-49 | Youheng Ou Yang, Sheng Xu, Merng Koon Wong. DOI: 10.13107/jocr.2019.v09.i06.1582
Authors: Youheng Ou Yang[1], Sheng Xu[1], Merng Koon Wong[1]
[1]Department of Orthopaedic Surgery, Singapore General Hospital, 20 College Road, Academia, Level 4 169865, Singapore.
Address of Correspondence:
Dr. Sheng Xu,
Department of Orthopaedic Surgery, Singapore General Hospital, 20 College Road, Academia, Level 4 169865, Singapore.
E-mail: sheng.xu@mohh.com.sg
Abstract
Introduction: Cannulated screw fixation is a common technique employed for the closed reduction and fixation of minimally or non-displaced neck of femur (NOF) fractures. A rare but potentially devastating complication is a peri-implant subtrochanteric fracture. Given the possibility of dealing with two potentially unstable fractures in close proximity from an incomplete union of the femoral neck, surgical fixation must be carefully planned with the option of retaining the existing cancellous screws to maintain femoral neck stability. The authors describe a case of subtrochanteric fracture in a patient with an existing NOF fracture which was previously fixed with cancellous screw fixation and have provided our approach to such patients.
Case Report: The patient is a 73-year-old Chinese male with a previous cancellous screw fixation for an undisplaced NOF fracture 10 months before sustaining another fall resulting in a subtrochanteric fracture. Radiographs and computed tomography imaging revealed a peri-implant subtrochanteric fracture with fracture line originating distal to the inferior screw at the level of the lesser trochanter.
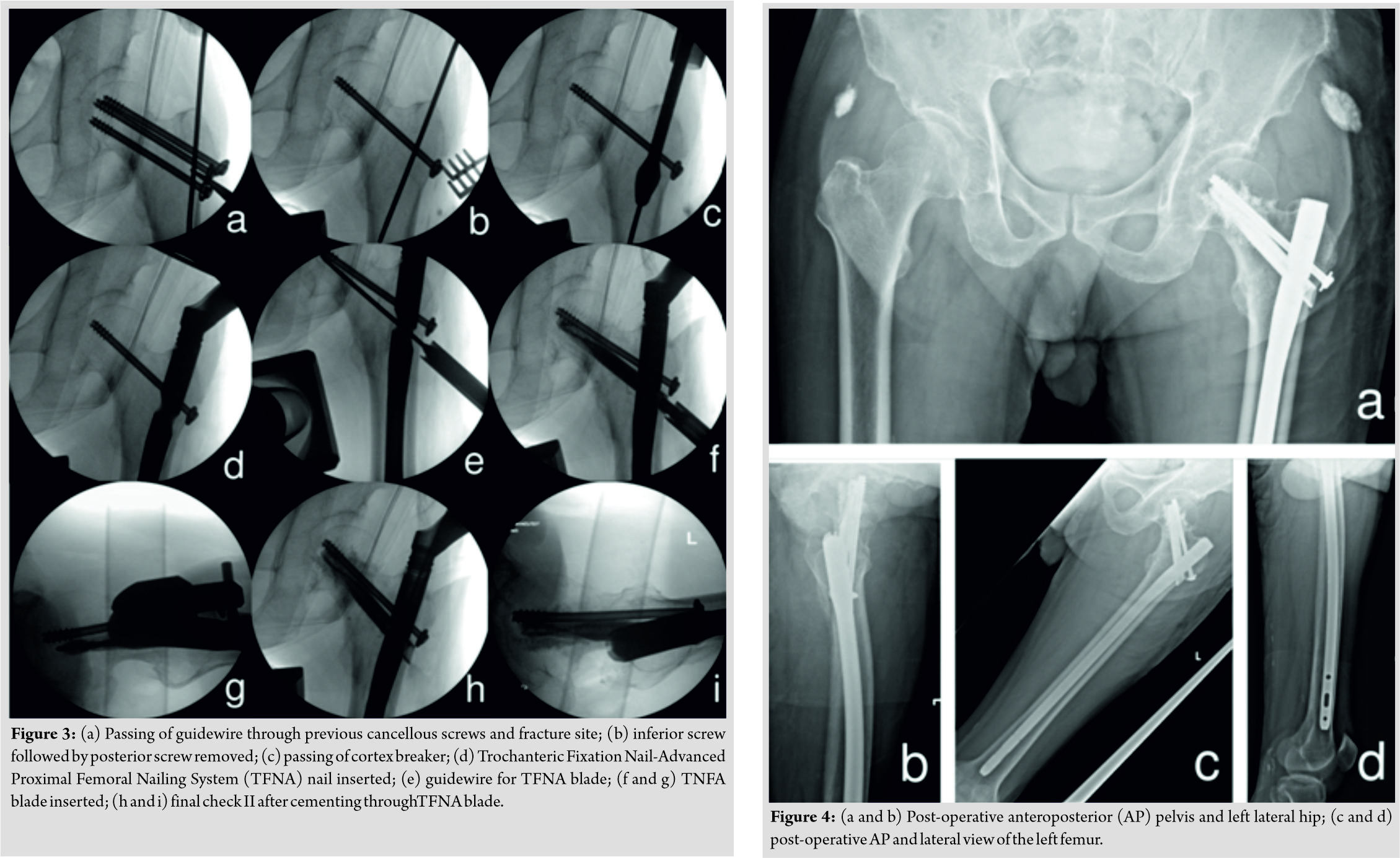
The patient subsequently underwent a Trochanteric Fixation Nail-Advanced Proximal Femoral Nailing System (TFNA, Depuy Synthes) fixation of peri-implant subtrochanteric fracture. Two previous cancellous screws (superior-posterior and inferior-central) were first removed to allow the passage of the TFNA nail which just skirted the remaining superior-anterior screw.
Postoperatively, the patient was allowed full weight-bearing with the patient managing to ambulate with a roller frame support on the immediate 1stpost-operative day. The subsequent progress was uneventful and at the final follow-up 6-month postoperatively, X-ray showed complete bony union and the patient is pain free and walking independently.
Conclusion: Peri-implant subtrochanteric fractures following NOF fractures treated with cancellous screws are surgically challenging. A robust system of evaluating such fractures and decision-making aids perioperative planning. An intimate understanding of implant geometries and basic science principles can significantly help in difficult cases and may reduce the likelihood of intraoperative difficulties and complications. Further large-scale studies are required to evaluate the validity of the approach we have proposed.
Keywords: Cancellous screw fixation, subtrochanteric fracture, periprosthetic fracture.
Introduction
Cannulated screw fixation is a common technique employed for the closed reduction and fixation of minimally or non-displaced neck of femur (NOF) fractures. A rare but potentially devastating complication is peri-implant subtrochanteric fracture. The incidence of subtrochanteric fracture post-cancellous screw fixation in literature is about 3% [1, 2], with majority occurring in the first 12 weeks but can occur as late as 24 weeks. The subtrochanteric fracture may occur due to the formation of a stress riser due to the difference in Young’s modulus between the rigid cancellous screws and the surrounding bone. There have been several studies investigating predisposing factors for such a fracture in the effort to decrease its incidence by optimizing the screw configuration and orientation [3], position of distal screw [4], and surgical technique [2]. Given the possibility of dealing with two potentially unstable fractures in close proximity from an incomplete union of the femoral neck, surgical fixation must be carefully planned with option of retaining the existing cancellous screws to maintain femoral neck stability. Due to its relatively rare incidence, most traditional solutions are based mainly on surgeons’ personal preferences and experience. Case series and reports in literature have shown conflicting results [5]. A rational approach to such patients is needed and should take into account clinical, radiological, and basic science considerations. The authors describe a case of subtrochanteric fracture in a patient with an existing NOF fracture which was previously fixed with cancellous screw fixation and have provided our approach to such patients.
Case Report
A 73-year-old Chinese male patient, who was a community ambulant without aid, slipped and fell while walking. Radiographs revealed a valgus-impacted NOF fracture (Fig. 1a and b). The patient underwent an uneventful cancellous screw fixation with three7.3mmscrews inserted in an inverted triangular configuration (inferior screw placed midway between the anterior and posterior cortices, superior screws placed as anterior and as posterior as possible in the sagittal plane, in the middle of the femoral neck on anteroposterior [AP]imaging). Threads of all three cancellous screws passed the fracture line into the femoral head (Fig. 1c and d).Post-operative Garden’s alignment index was satisfactory at 160° in the AP plane and 170° in the lateral plane. The patient recovered well postoperatively and regained independent ambulatory status. At 10-month post-operative, the patient sustained another fall while walking and complained of pain over the left hip and inability to weight bear. Radiographs and computed tomography (CT) imaging revealed a peri-implant subtrochanteric fracture with a fracture line originating distal to the inferior screw at the level of the lesser trochanter (Fig. 2a and e).
The patient subsequently underwent a Trochanteric Fixation Nail-Advanced Proximal Femoral Nailing System (TFNA, Depuy Synthes) fixation of peri-implant subtrochanteric fracture. This was achieved with the patient under general anesthesia and on a traction table aiding reduction of the subtrochanteric fracture. Two previous cancellous screws (superior-posterior and inferior-central) were first removed to allow the passage of the TFNA nail which just skirted the remaining superior-anterior screw. The TFNA blade was measured and inserted without incident. As per the authors’ preferences, the distal locking screws were left unlocked.
Postoperatively, the patient was allowed full weight-bearing with the patient managing to ambulate with a roller frame support on the immediate 1st post-operative day and was discharged well soon after. This subsequent progress was uneventful and the patient was able to ambulate fluidly at 3-month post-operative. At the final follow-up 6-month postoperatively, X-ray showed complete bony union and the patient is pain free and walking independently.
Discussion
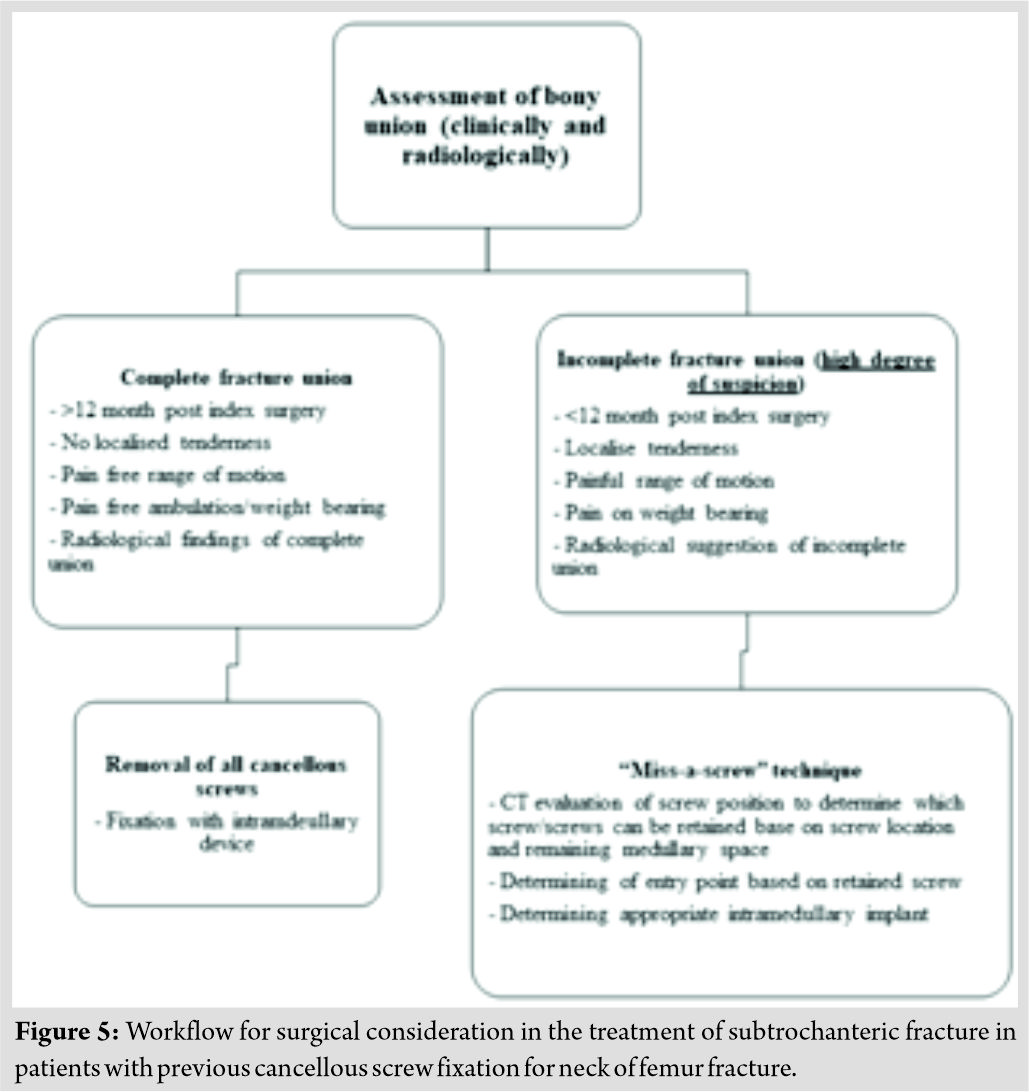
Subtrochanteric fracture after previous cancellous screw fixation for NOF fracture is rare but difficult to manage complication that poses technical difficulties to the surgeon. Both intramedullary and extramedullary fixation techniques have been described with varying degrees of success. In a series by Howard et al., in 1982, 10 out of 408 patients developed subtrochanteric fracture after the two screws Garden technique [6] for the treatment of subcapital fracture. Six of those patients were treated with a McLaughlin pin and plate, the pin being substituted for one of the screws. However, the complication rate was high with 50% of patients developing a complication. In 1984, Mac Eachern et al. [7] described a method of fixation by substituting a Richards sliding screw of a corresponding angle for the lower cancellous screw which resulted in good union in all four patients treated. Similarly, Mackie and Leyshon [8] described a technique of replacing the lower cancellous screw with an AO dynamic hip screw and a five-hole plate in onepatient, resulting in satisfactory healing of both fractures. More recently, Jansen et al. [1] described a case series of two patients who underwent intramedullary nailing of the peri-implant subtrochanteric fracture which also led to a good outcome. At present, there are no standardized means of fixation and most literature is based on authors’ personal experiences. While we acknowledge that there are a multitude of possible fixation methods and considerations to take note, from fracture pattern, degree of NOF fracture union, to the specific previous placement of cancellous screws, we believe that a framework of management can be developed. We, therefore, propose a rational system of evaluating and managing such fractures as well as provide some technical insights to achieve good fixation (Fig. 5). In our protocol, we divide cases by previous NOF union after cancellous screw fixation. Previous union is of utmost importance as it dictates whether screw removal is possible while avoiding a disastrous scenario, in which there area concurrent iatrogenic NOF and subtrochanteric fracture. Union can be assessed clinically as well as radiologically [9]. Clinically relevant factors would include the duration since index surgery, the presence of hip pain on weight-bearing, ambulatory status, and concurrent medical comorbidities which might delay healing such as the presence of renal failure or osteoporosis. Radiological union is best evaluated through plain film and CT imaging [10]. Radiological imagining should be interpreted with caution in light of the metallic artifacts generated by the clustered cancellous screws insitu. A low index of suspicion should be adopted in the anticipation that femoral neck could be subjected to great stresses during the subsequent subtrochanteric surgery on a traction table or during reduction to overcome the strong muscular deforming forces acting at the subtrochanteric area. In the case of a completely united NOF fracture, simple implant removal should suffice with the subtrochanteric fracture treated as an isolated injury. In such circumstances, the authors recommend the placement of an intramedullary device as extramedullary devices (such as fixed angle blade plates or a sliding hip screw and plate) rely on fixation at the level of the femoral neck to resist the large amounts of laterally directed coronal and anterior/posterior sagittal plane stresses. The placement of the critical neck component resides within cancellous bone and therefore relies on cancellous impaction in normal bone to achieve stability [11]. However, as there are voids from the removal of large cancellous screws, this impaction of cancellous bone may be compromised. Intramedullary devices such as nails rely on the long lever arm passing inferiorly to resist the above stresses and are thus less affected. In the case of an incompletely united NOF fracture, strategies must be applied to retain the cancellous screws to maintain the reduction of the femoral neck. In this case, both extramedullary devices and intramedullary devices may be used. A careful analysis of the existing screws should be undertaken preoperatively. As previously described, the removal of the inferior-most screw and substitution with a dynamic hip screw has led to good results. However, it is the authors’ preference to treat subtrochanteric fractures with intramedullary devices in light of their biomechanical advantages mentioned above. A meta-analysis by Liu et al. [12] also found a significant lower rate of fracture fixation complication such as revision rate, fixation failure rate, and non-union rate with intramedullary fixation compared to extramedullary fixation for subtrochanteric fracture, especially in the elderly. In such cases, a “miss-a-screw” technique must be employed. The technical challenges can be analyzed with the proximal real estate and nail entry point in mind. First, a decision must be made on which screw(s) is/are retained. This is best evaluated on the sagittal cuts in a CT scan. Screws which are the most eccentric and whom allow the largest medullary fit should be retained and a measurement of the potential medullary canal diameter taken. Next the entry point should be evaluated, in the case of retaining anterior screws, a more posterior entry point should be selected and vice versa with retained posterior screws. By considering the natural bow of a femur, an intramedullary nail with an appropriate radius of curvature and proximal femoral fit can be selected.
To illustrate these concepts, we will now discuss the case report in detail:
The patient had a NOF fracture fixed with three cancellous screws in an inverted triangle configuration, approximately 10 months before sustaining another subtrochanteric fracture. As the duration between index surgeries was relatively short and the patient reporting occasional hip pain prior to the fall, we discounted radiographical evidence of union by adopting a low index of suspicionfor possible incompletely united NOF fracture. Subsequently, we analyzed the pattern of cancellous screw fixation and elected to retain the anterior superior screw. A measurement of the screw-posterior wall distance revealed adequate clearance for an intramedullary nail allowing us to proceed to the next step. The patient’s anterior femoral bow was evaluated to be normal and a more posterior nail entry point was anticipated. Implant selection was subsequently conducted. To illustrate this next concept, two nail designs have been presented as examples: The TFNA and proximal femoral nail antirotation (PFNA II), both implants are manufactured by Synthes. These implants have no specific advantages over each other and are presented with the aim of demonstrating that a deep understanding of implant geometry can greatly aid perioperative planning. The TFNA has a smaller radius of curvature of 1m compared to the PFNA II of 1.5m, this helps in preventing an anterior wall fracture from a posterior starting point in a patient with a normal femoral bow. Second, the proximal femoral diameter of the TFNA is smaller at 15.66mm compared to 16.5mm in the PFNA II which affords more proximal clearance. By utilizing the specific geometries of the implants, we were able to “miss-a-screw” and obtain stable fixation of the peri-implant subtrochanteric fracture. It should be noted that the TFNA retains one technical advantage over the PFNA II in the option of cement augmentation of the femoral head. This design advance was exploited and interestingly, the cement clearly delineated the voids left behind by the removal of screws (Fig. 4a and b) which would support the concern for suboptimal cancellous fixation after implant removal. A final consideration arises from the material of the cancellous screw (stainless steel) and TFNA nail (titanium). Conventional AO recommendations include an avoidance of mixing cobalt chrome with stainless steel implants to avoid galvanic corrosion from two electrochemically dissimilar metals [13]. Galvanic corrosion may occur as a consequence of existing electrochemical potential difference between dissimilar biomaterials. The least noble metal in a galvanic coupling is more likely to corrode. Nickel and chrome ions from artificial prosthesis may pass to peri-implant tissues due to the leakage of saliva between implant and superstructure. This may result in bone reabsorption and also affect the stability of the implant and eventually cause failure. However, multiple studies invivo [14] and invitro [15] have shown that the specific combination of stainless steel and titanium is safe in part due to the rapidly forming self-passivating oxide layer exhibited by both metals.
Conclusion
Peri-implant subtrochanteric fractures following NOF fractures treated with cancellous screws are surgically challenging. A robust system of evaluating such fractures and decision-making aids perioperative planning. An intimate understanding of implant geometries and basic science principles can significantly help in difficult cases and may reduce the likelihood of intraoperative difficulties and complications. Further large-scale studies are required to evaluate the validity of the approach we have proposed.
Clinical Message
Peri-implant subtrochanteric fractures following NOF fracture treated with cancellous screws are surgical challenging. The “miss-a-screw” technique will assist surgeons met with similar patient in future to help with the decision-making progress.
References
1. JansenH, FreySP, MeffertRH. Subtrochanteric fracture: A rare but severe complication after screw fixation of femoral neck fractures in the elderly.Acta OrthopBelg2010;76:778-84.
2. AndrewTA, ThorogoodM. Subtrochanteric fracture after garden screw fixation: A review of predisposing factors and management in nine cases.Injury1984;16:169-77.
3. OakeyJW, StoverMD, SummersHD, SartoriM, HaveyRM, PatwardhanAG. Does screw configuration affect subtrochanteric fracture after femoral neck fixation?Clin OrthopRelat Res2006;443:302-6.
4. KloenP, RubelIF, LydenJP, HelfetDL. Subtrochanteric fracture after cannulated screw fixation of femoral neck fractures: A report of four cases.J Orthop Trauma2003;17:225-9.
5. TsaiAG, AshworthTJ, MarcusR, AkkusO. Femoral iatrogenic subtrochanteric fatigue fracture risk is not increased by placing drill holes below the level of the lesser trochanter.Iowa Orthop J2017;37:23-8.
6. Garden RS. Low angle fixation in fractures of the femoral neck. J Bone Joint Surg 1964;43-B:647-63.
7. MacEachernAG, Heyse-MooreGH, JonesRN. Subtrochanteric fractures of the femur through the track of the lower garden screw–treatment with a Richards sliding screw.Injury1984;15:337-40.
8. MackieIG, LeyshonRL. Sub-trochanteric fracture (after garden-screw fixation of sub-capital fracture) treated with AO dynamic hip screw and plate.Injury1983;15:136-7.
9. MorshedS. Current options for determining fracture union.Adv Med2014;2014:708574.
10. MorganEF, MasonZD, ChienKB, PfeifferAJ, BarnesGL, EinhornTA,et al. Micro-computed tomography assessment of fracture healing: Relationships among callus structure, composition, and mechanical function.Bone2009;44:335-44.
11. David GL. Campbell’s Operative Orthopaedics. 10th ed. St. Louis: Mosby; 2003. p. 2897.
12. LiuP, WuX, ShiH, LiuR, ShuH, GongJ, et al. Intramedullary versus extramedullary fixation in the management of subtrochanteric femur fractures: A meta-analysis.Clin Interv Aging2015;10:803-11.
13. Disegi J. Wrought 18% Chromium-14% Nickel-2. 5% Molybdenum Stainless Steel Implant Material. Paoli, PA: AO ASIF Materials Technical Commission; 1998.
14. Rüedi T, Perren SM, Pohler O, Riede U. Titanium, steel and their combination in bone surgery. Langenbecks Arch Chir1975;???:395-8.
15. HølPJ, MølsterA, GjerdetNR. Should the galvanic combination of titanium and stainless steel surgical implants be avoided?Injury2008;39:161-9.
 |
 |
 |
| Dr. YouhengOu Yang | Dr. Sheng Xu | Dr. Merng Koon Wong |
| How to Cite This Article: Y H Ou Yang, S Xu, M K Wong. Surgical Fixation of Subtrochanteric Fracture in Patient with Cancellous Screw Fixation for Neck of Femur Fracture: Surgical Decision-Making and Outcome. Journal of Orthopaedic Case Reports 2019 Nov-Dec;9(6): 44-49. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com