[box type=”bio”] Learning Point of the Article: [/box]
Proximal femoral fractures after hip resurfacing are difficult to treat: conservative treatment might prove disappointing for the patient and the surgeon and we believe that anatomic reduction and stable fixation is the appropriate management of such injuries, and that an anatomic variable angle locking plate is an implant of choice for this fracture pattern.
Case Report | Volume 9 | Issue 6 | JOCR November – December 2019 | Page 65-69 | Simon Koulischer, Stéphane Devos, Pierre-Bernard Verstraeten, Olivier Delahaut, Atdhe Muhadri. DOI: 10.13107/jocr.2019.v09.i06.1592
Authors: Simon Koulischer[1], Stéphane Devos[2], Pierre-Bernard Verstraeten[2], Olivier Delahaut[2], Atdhe Muhadri[2]
[1]CHU Saint-Pierre, Rue aux Laines 105, 1000 Bruxelles, Belgium,
[2]Orthopedics and Traumatology Service ISPPC Charleroi, Boulevard ZoéDrion 1, 6000 Charleroi, Belgium.
Address of Correspondence:
Dr. Simon Koulischer,
CHU Saint-Pierre, Rue aux Laines 105, 1000 Bruxelles, Belgium.
E-mail: simon.koulischer@gmail.com
Abstract
Introduction: Periprosthetic fracture is the most common cause of reoperation after resurfacing arthroplasty. The majority of fractures associated with this kind of arthroplasty are mostly subcapital fractures. Inter- and sub-trochanteric fractures after resurfacing arthroplasty are rarely reported, and there is no consensus regarding the treatment of such fractures.
Case Report: We present the case of a patient in whom an intertrochanteric femoral fracture distal to a hip resurfacing implant was successfully managed by internal fixation with the use of a locking compression plate (LCP), after failed conservative management. We also discuss an in-depth literature review on the topic.
Conclusion: We believe that osteosynthesis is a better option than arthroplasty in the management of such injuries. Due to technical issues discussed in our paper, we believe LCP to be an optimal fixation device.
Keywords: Resurfacing arthroplasty, periprosthetic fracture, intertrochanteric fracture.
Introduction
Resurfacing arthroplasty is still regarded by many surgeons as a useful option for arthroplasty in young patients who are likely to require a future revision hip procedure. This type of arthroplasty has its unique set of complications. Periprosthetic fracture is the most common cause of reoperation. A multisurgeon national audit of the first 3429 metal-on-metal hip resurfacing arthroplasties performed in Australia over a 4-year period demonstrated a fracture rate of 1.46% at a mean of 15.4 weeks postoperatively [1]. Risk factors include notching of the superior part of the femoral neck and varus femoral placement relative to the anatomical neck[2].Patient-associated factors include female gender and poor proximal femoral bone quality [3]. The majority of fractures associated with this kind of arthroplasty are mostly subcapital fractures. Inter- and sub-trochanteric fractures after resurfacing arthroplasty are rarely reported. Although multiple management options have been proposed, there is no consensus regarding the treatment of such fractures. The frequent association of these injuries with a poor proximal femoral bone stock makes those fractures difficult to fix. Complex revision arthroplasty procedure is, however, associated with a high rate of complication. We present the case of a patient in whom an intertrochanteric femoral fracture distal to a hip resurfacing implant was successfully managed by internal fixation with the use of a locking compression plate (LCP).
Case Report
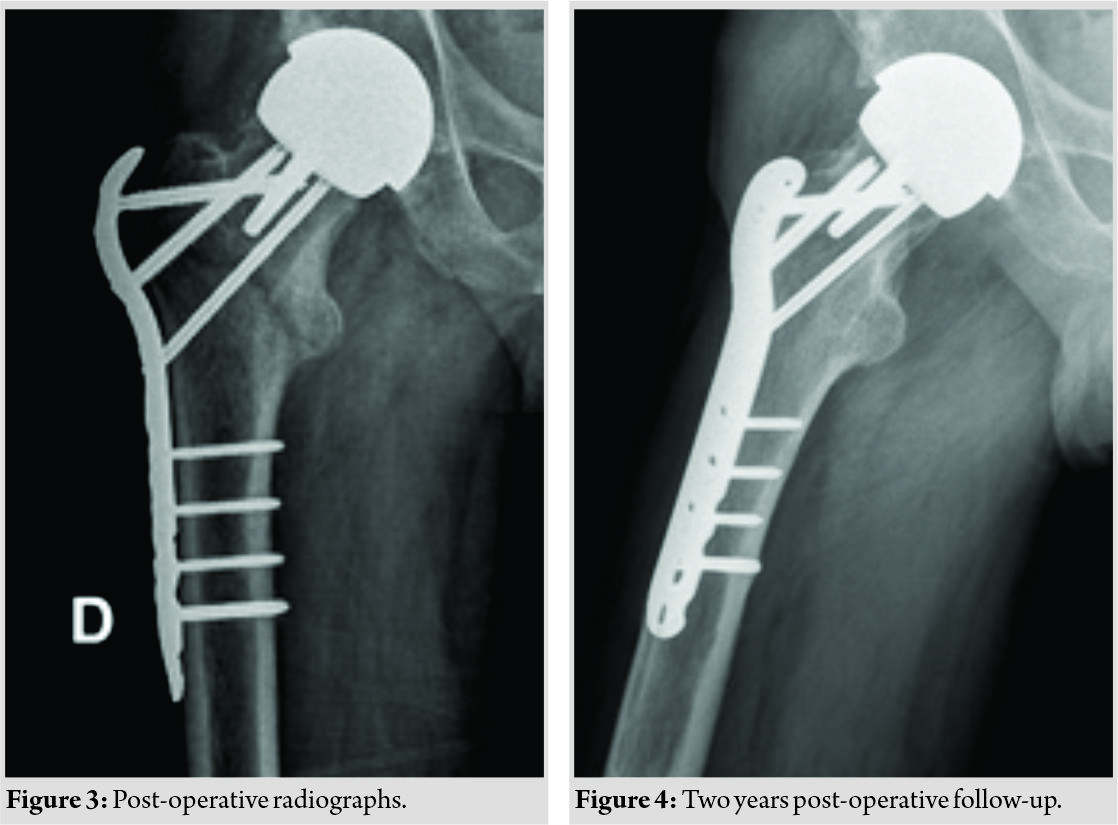
A 46-year-old-man was admitted to our emergency department after a fall from his own height. Two years earlier, he had undergone a resurfacing arthroplasty (Cormet, Corin Group, Cirencester, UK) of the right hip following avascular necrosis of the femoral head. The recovery from the arthroplasty had previously been uneventful, and post-operative radiographs revealed satisfactory positioning of the implants. Three months before the admission in our institution, the patient suffered a motorcycle injury and was diagnosed with a talus fracture, which was treated conservatively. On admission in the emergency department, the patient complained of severe pain in the right hip and was unable to stand. Radiographs showed a closed intertrochanteric fracture, AO 31-A2 (Fig. 1). In our opinion, disuse osteopenia following the conservative treatment of the talus fracture might have contributed to an increased fracture risk. After consideration of the management options and discussion with the patient, and with regard to the minimal displacement of the fragments, a conservative treatment was undertaken. A skin traction of 3kg was applied. Ten days after the admission, control radiographs revealed a significant displacement of the fragments (Fig. 2).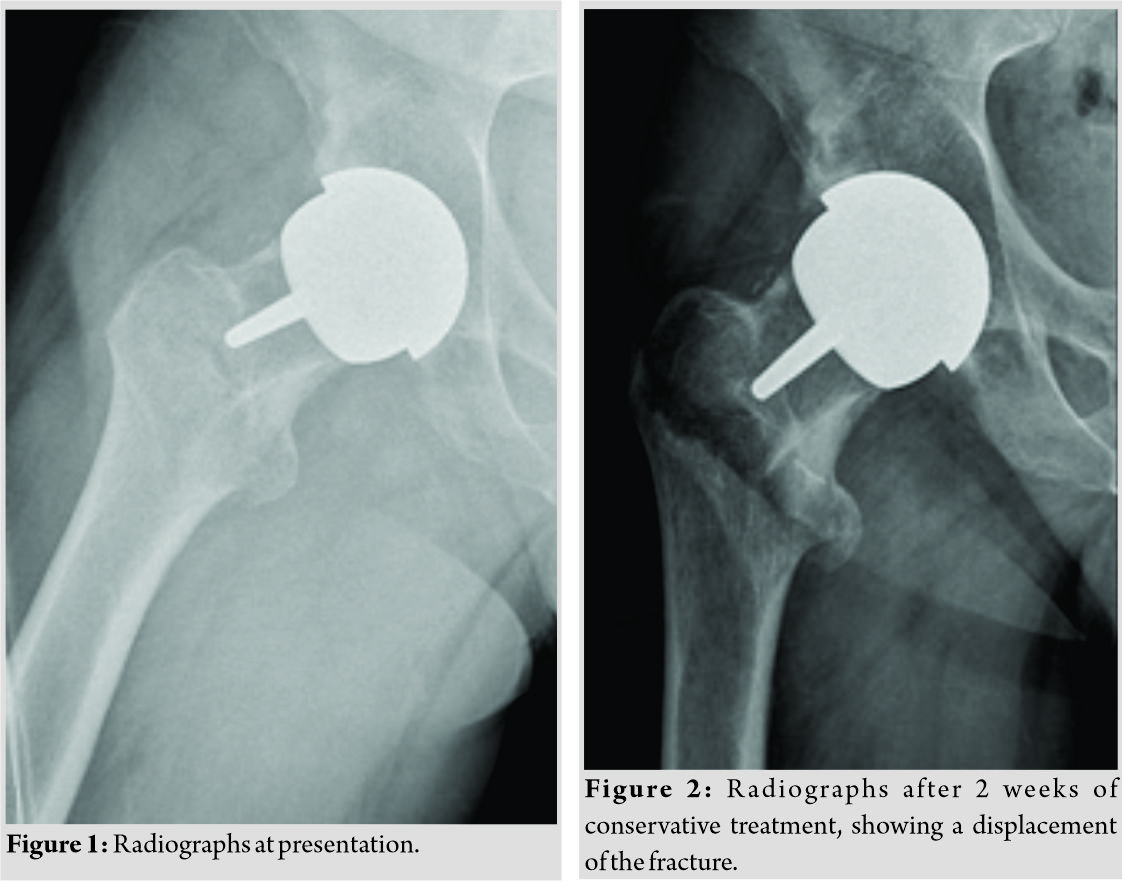
Discussion
Subcapital hip fracture
Periprosthetic fracture is a well-known complication of hip resurfacing. Most of these fractures are subcapital hip fractures because hip resurfacing increases the stress in femoral neck even in the absence of notching [4]. Subcapital fracture after hip resurfacing requires conversion to total hip arthroplasty (THA) [5]. The study of Matharu et al. showed a poor implant survivorship after conversion to THA: In the subgroup of the patient revised for fracture, 7 of 21 (33%) were rerevised at 10 years after conversion to THA [6]. Conservative treatment has been advocated by some authors. Cossey et al. reported seven cases of intracapsular fracture neck of femur after Birmingham hip resurfacing. They were treated conservatively non-weight-bearing for 4–6 weeks with good results[7].
Trochanteric fracture
Fractures in the trochanteric region are less common, and their treatment is more challenging. Rubin and Rubin reported a successful conservative treatment of an intertrochanteric fracture. Toe-touch weight-bearing with crutches was started from the beginning, with weight gradually increasing to full weight-bearing at 3 months post-trauma [8]. Morgan et al. similarly reported two cases of intertrochanteric fracture that was managed conservatively [9]. Although this option might be considered in compliant patient and in patient with high perioperative risk, our case presented a secondary displacement of the fracture, highlighting the instability of such fracture. The side effects of bed rest (pressure sores, etc…) should also not be overlooked. Difficulty associated with the proximal fixation of these fractures is often due to the presence of the centrally located prosthetic stem in the femoral neck which limits the space available for fixation and the poor bone mineral density in the proximal femur which compromises the proximal purchase of any fixation device. Furthermore, cement pressurized into the femoral neck around the stem of the implant might obstruct the passage of the blade or the screws.
Various fixation techniques have been reported.
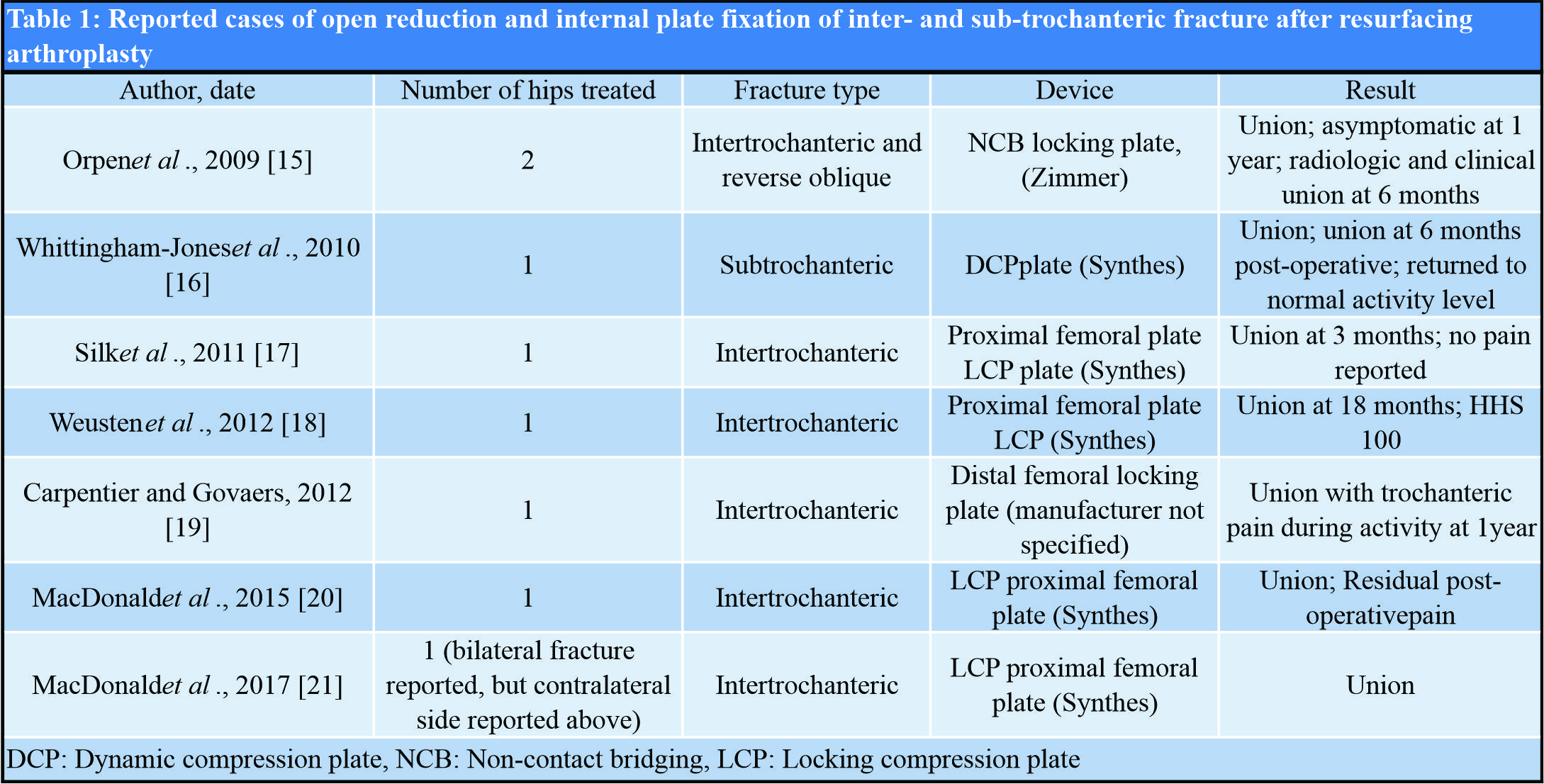
Two authors described the successful treatment of two different intertrochanteric fractures following hip resurfacing with screw fixation [10, 11]. Although minimal invasive, we believe that this fixation method might lack sufficient stability, particularly in the presence of a poor bone density. Most screw and blade plates (e.g., dynamic hip screw plates,…) and intramedullary devices for internal fixation of intertrochanteric hip fractures utilize a centrally placed lag screw. With a resurfacing femoral component stem located within the femoral neck, the placement of such an implant might be impossible or would require the lag screw to be placed in a substantially eccentric position. Weinrauch, however, reported that the use of a blade plate has an alternative method of fixation [12]. Banerjee et al. and Aning et al. described an alternative method using a cephalomedullary reconstruction nail and two proximal interlocking screws. Using a nail, it could, still, however, be possible that one of the two proximal screws interfered with the stem of the femoral component due to the fixed angulation of these screws [13, 14]. The most frequently reported device of fixation is the locking plate[15, 16, 17, 18, 19, 20,21].Such plates have the advantage that if one of the locking screws interferes with the stem, a non-locking screw can be placed in a different direction. Reported cases of open reduction and internal plate fixation of inter- and sub-trochanteric fracture after resurfacing arthroplasty are summarized in [Table 1]. Although locking plate fixation is the most documented fixation method, definite conclusions favoring one device over another in the fixation of these per- and inter-trochanteric fractures are difficult to construe. We do, however, believe that locking plates provide adequate stability compared to other fixations methods, with an acceptable rate of complications.
Conclusion
We present the case of an intertrochanteric fracture after hip resurfacing treated with open reduction and internal fixation after a failed attempt of conservative treatment. With regard to the issues of stability and medical problems associated with conservative treatment, and considering the risks of complex revision arthroplasty procedures, we believe osteosynthesis to be the option of choice in the management of such injuries. Due to the technical issues discussed in our paper, we believe that LCP fixation is an optimal fixation device.
Clinical Message
Proximal femoral fractures after hip resurfacing are difficult to treat. In this case, an attempted conservative treatment failed, highlighting the instability of such fracture. We believe that surgical reduction and fixation is the appropriate management of such injuries and that variable angle locking plate is, to this date, the implant of choice.
References
1. Shimmin A, Beaulé PE, Campbell P. Metal-on-metal hip resurfacing arthroplasty. J Bone Joint Surg Am 2008;90:637-54.
2. Zustin J, Krause M, Breer S, Hahn M, von Domarus C, Rüther W, et al. Morphologic analysis of periprosthetic fractures after hip resurfacing arthroplasty. J Bone Joint Surg Am 2010;92:404-10.
3. Marker DR, Seyler TM, Jinnah RH, Delanois RE, Ulrich SD, Mont MA, et al. Femoral neck fractures after metal-on-metal total hip resurfacing: A prospective cohort study. J Arthroplasty 2007;22:66-71.
4. Wik TS, Østbyhaug PO, Klaksvik J, Aamodt A. Increased strain in the femoral neck following insertion of a resurfacing femoral prosthesis. J Bone Joint Surg Br 2010;92:461-7.
5. Wera GD, Gillespie RJ, Petty C, Petersilge WJ, Kraay MJ, Goldberg VM, et al. Revision of hip resurfacing arthroplasty. Am J Orthop (Belle Mead NJ) 2010;39:E78-83.
6. Matharu GS, Pandit HG, Murray DW. Poor survivorship and frequent complications at a median of 10 years after metal-on-metal hip resurfacing revision. Clin OrthopRelat Res 2017;475:304-14.
7. Cossey AJ, Back DL, Shimmin A, Young D, Spriggins AJ. The nonoperative management of periprosthetic fractures associated with the Birmingham hip resurfacing procedure. J Arthroplasty 2005;20:358-61.
8. Rubin PG, Rubin CG. Intertrochanteric fracture after hip resurfacing arthroplasty: Successful non operative treatment. Webmedcentral 2015;5:WMC004636.
9. Morgan D, Myers G, O’Dwyer K, Thomas AM. Intertrochanteric fracture below Birmingham Hip Resurfacing: Successful non-operative management in two cases. Injury Extra 2008;39:313-5.
10. Lein T, Schlee J, Kothe M, Moritz F, Wubtaye DT. Periprosthetic intertrochanteric fracture of the femur following articular resurfacing of the hip joint: Treatment with lag screw osteosynthesis. Unfallchirurg2010;113:944-50.
11. Haddad BZ, Konan S, McAuliffe TB. Successful fixation of an intertrochanteric fracture after hip resurfacing arthroplasty using cannulated screws. J Arthroplasty 2013;28:197.e13-6.
12. Weinrauch P, Krikler S. Proximal femoral fracture after hip resurfacing managed with blade-plate fixation. A case report. J Bone Joint Surg Am 2008;90:1345-7.
13. Banerjee S, Little T, Little N. Intramedullary fixation of pertrochanteric fractures after hip resurfacing arthroplasty do we have the answer? Case report and literature review. J Orthop2015;12:66-9.
14. Aning J, Aung H, Mackinnon J. Fixation of a complex comminuted proximal femoral fracture in the presence of a Birmingham hip resurfacing prosthesis. Injury 2005;36:1127-9.
15. Orpen NM, Pearce O, Deakin M, Keys R. Internal fixation of trochanteric fractures of the hip after surface replacements. Injury Extra 2009;40:32-5.
16. Whittingham-Jones P, Charnley G, Francis J, Annapureddy S. Internal fixation after subtrochanteric femoral fracture after hip resurfacing arthroplasty. J Arthroplasty 2010;25:334.e1-4.
17. Silk G, Sangster M, Sandhu H. Internal fixation of trochanteric fracture following hip resurfacing. Injury Extra 2011;42:183-5.
18. Weusten AJ, Khan SK, Bonczek SJ, Elsharief D, Wallace IW. Internal fixation of a traumatic fracture around a hip resurfacing arthroplasty using the proximal femoral locking compression plate. Acta OrthopBelg2012;78:688-93.
19. Carpentier K, Govaers K. Internal fixation of an intertrochanteric femoral fracture after Birmingham hip resurfacing arthroplasty. Acta OrthopBelg2012;78:275-8.
20. Macdonald J, Robinson A, Brown I. Fixation of a periprosthetic intertrochanteric hip fracture below a Birmingham hip resurfacing. Case Rep Orthop2014;2014:393984.
21. Macdonald J, Pagoti R, Cusick L. Bilateral fixation of a periprosthetic intertrochanteric hip fracture below Birmingham hip resurfacing. BMJ Case Rep 2017;2017:bcr2016218840.
| How to Cite This Article: Koulischer S, Devos S, Verstraeten P, Delahaut O, Muhadri A. Internal Fixation of an Intertrochanteric Fracture after Resurfacing Arthroplasty: A Case Report. Journal of Orthopaedic Case Reports 2019 Nov-Dec; 9(6): 65-69. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com