[box type=”bio”] Learning Point of the Article: [/box]
Pigmented villonodular synovitis should be considered in diagnostic flow chart of anterior ankle impingement.
Case Report | Volume 10 | Issue 1 | JOCR January – February 2020 | Page 16-18 | Federico Morelli, Giorgio Princi, Alessio Rossato, Raffaele Iorio, Andrea Ferretti. DOI: 10.13107/jocr.2019.v10.i01.1618
Authors: Federico Morelli[1], Giorgio Princi[1], Alessio Rossato[1], Raffaele Iorio[1], Andrea Ferretti[1]
[1]Department of Trauma and Orthopaedics, S. Andrea Hospital, University of Rome “Sapienza,” Rome, Italy.
Address of Correspondence:
Dr. Giorgio Princi,
Department of Trauma and Orthopaedics, S. Andrea Hospital, University of Rome “Sapienza,” Rome, Italy.
E-mail: giorgioprinci@gmail.com
Abstract
Introduction: Anterior ankle impingement is characterized by a painful range of motion (ROM)limitation of tibiotarsal joint. More than 70% of cases are secondary to trauma or repetitive microtrauma of the anterior aspect of the ankle such as it occurs during ball kicking (“footballer’s ankle”) or forced plantar flexion (ballet dancers, volleyball players, and runners) in people practicing sport for many years. There are other causes of anterior ankle impingement. We report a case of villonodular synovitis that, also less common, has to be considered in diagnostic flowchart.
Case Report: In this paper, we report a rare case of pigmented villonodular synovitis (PVNS) in a 37-year-old Caucasian male soccer player, with a 4-year story of ankle swelling and ROM painful limitation.
Conclusion: PVNS, although it is an unusual cause of anterior ankle impingement, needs an early diagnosis and surgical excision to prevent extra-articular extension of the mass, cartilage damage, and soft tissue compression.
Keywords: Ankle, impingement, pigmented villonodular synovitis.
Introduction
Anterior ankle impingement, also known as “footballer’s ankle” or “athlete’s ankle” due to its high frequency of occurrence in sportactive population, is characterized by a chronic painful limitation of range of motion (ROM) of tibiotarsal joint. It can be classified according to the pathological tissue (bone or soft tissue) developed on the anterior aspect of the ankle. Repetitive anterior microtrauma such as during ball kicking (soccer players) or forced plantarflexion (ballet dancers, volleyball players, and runners) of the ankle has been advocated as the most frequent pathogenetic factor responsible of the onset of a symptomatic anterior ankle impingement. Major trauma (i.e., fracture, ankle sprain, or dislocation), surgery, rheumatic disease, or infection have been described as a possible cause of this pathology. Pigmented villonodular synovitis (PVNS) is an unusual cause of anterior ankle impingement; it is considered a benign proliferative disorder of the synovial tissue, with uncertain pathogenesis. The incidence is estimated to be 1.8 per million in the general population with a preponderance in the third and fourth decades of life [1]. Two types of PVNS have been described, with no differences in histological characteristics: Localized PVNS and diffuse PVNS [2].
Case Report
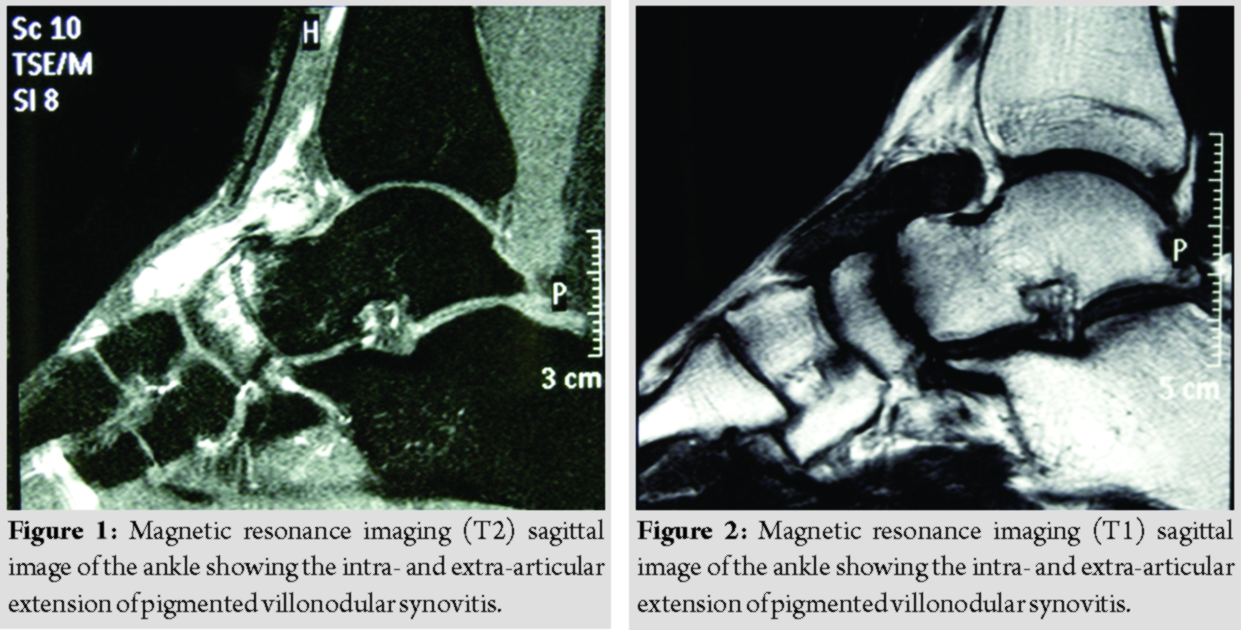
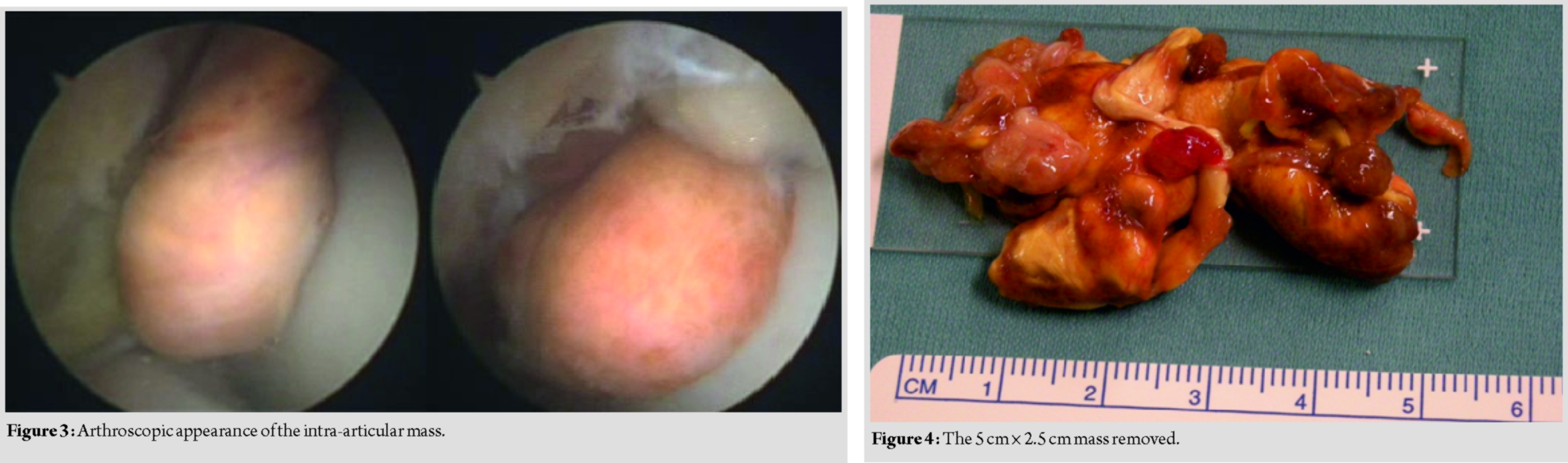
A 37-year-old Caucasian male, professional soccer player, presented in our department in December 2008 with a 4-year history of swelling of the anterior aspect of his left ankle, limitation of ROM and painful limitation of everyday, and sport activity (especially running and kicking the ball). He did not report any previous trauma, ankle sprain, or surgery and his medical history was not contributory. Physical examination revealed a hardelastic mass in the anterior aspect of the ankle, painful at palpation, with severe limitation of his ankle dorsiflexion (10°). The patient reported several conservative treatments in the past years (i.e.,physical therapy (PT), drugs, and orthoses) without any benefits. At X-ray examination, no osseous spurs could be found. Magnetic resonance imaging (MRI) scans revealed in the anterior aspect of the ankle joint a multinodular cystic-like capsulated mass with a major intra-articular localization, but an extra-articular extension was clearly identifiable with deep relations with the extensor tendons sheath. The mass had low signal intensity on T1 and signal dropout on T2-weighted images suggestive for PVNS (Fig. 1 and 2). Under general anesthesia and supine position, we performed an anterior ankle arthroscopy through standard anterior portals. A well-encapsulated rounded mass was found in the anterior aspect of the joint (Fig.3), while the talar and tibial cartilage surface were uninvolved. Distally, the mass was extruding the joint space through a lesion of the articular capsule. Complete mobilization of the mass could not be achieved with an arthroscopic-assisted technique without the risk of damaging the mass capsule and contaminating the joint. The surgery was converted to an open procedure. Just deep to the extensor fingers tendon and partially adherent to their sheath, a brown, encapsulated, lobulated, 5 cm × 2.5cm mass was identified. The neo formation was carefully dissected from soft tissues and tendons sheath and entirely excised (Fig.4). Optical microscope examination revealed mononucleated histiocytes, multinucleated giant cells, foaming histiocytes, and hemosiderin deposits, consistent with diagnosis of PVNS. No intraoperative or post-operative complications occurred. The patient was dismissed from hospital the day after surgery with compression bandaging and allowed to weight-bearing as tolerated. At 2-week post-operative, the patient was incentivated to return to full weight-bearing and a PT program was started. At 6-week post-operative, the patient was allowed to return to sport activity with no limitation. At the final follow-up,10-year post-operative, the patient did not refer any discomfort at his left ankle and no limitation in any sport or daily living activity. Physical examination revealed no pain or swelling on the anterior aspect of the ankle and a complete asymptomatic ROM of the joint. MRI did
not show any recurrence of the neoformation.
Discussion
In 1852,Chassaignac [3]described an abnormal sarcomatous such as synovial proliferation of the finger flexor tendons sheath, but the term PVNS was first used by Jaffe et al. [4], in 1941, as a benign, hypertrophic synovial process characterized by villous, nodular or villonodular proliferation, and abnormal pigmentation by hemosiderin. Etiology is uncertain [5], but cytogenetic studies provide increasing evidence that it has more likely neoplastic origin [6]. The disease can be localized or diffuse and either intra-articular or extra-articular: Diffuse PVNS involves the entire joint synovium, while the localized form is characterized by a single well-defined lesion surrounded by normal synovial membrane. PVNS is usually a monoarticular process of the big joints, affecting the knee in 80% of cases; rarely, the hip, ankle, shoulder, and elbow may be affected [7]. PVNS of the ankle occurs in <2.5% of cases [8]; the localized form being more common than the diffuse form. Rare malignant PVNS has also been reported in few cases with poor outcome. Clinical appearance and subjective symptoms may vary greatly depending on location and form: Extra-articular localized PVNS appears as a painful soft tissue mass, while intra-articular form is characterized by pain on weight-bearing and swelling, being joint disorders unusual in the initial stages. X-ray examination is generally nonspecific at the early stages [9], while MRI scan is suggestive for PVNS: Hemosiderin deposits determine a characteristic low signal intensity on T1, signal dropout on T2, and a paramagnetic effect with fast field echo images [10]. The treatment options include surgical resection, radiation therapy, pharmaceutical modulation of the disease, or a combination of these procedures. Localized PVNS is more likely treated with surgical excision; conversely, adjuvants therapies are recommended for diffuse intra-articular involvement [11]. The excision of the pathological tissue in intra-articular disease may be performed either arthroscopically or with an open technique, but it is mandatory to preserve intact the mass capsule due to the high risk of local recurrence. To the best of our knowledge, there is no report in literature of contemporary intra- and extra-articular localization of PVNS. Moreover, anterior ankle impingement is rarely caused by a villonodular synovitis. More likely, the case we report had an early intra-articular origin with subsequent lesion of the joint capsule by the enlarging mass. Extra-articular diffusion resulted in soft tissue adherences and compression on the overlying tendons sheath. Simultaneous presence of extra-articular adherences, large size, and intra-articular extension of the mass was most probably responsible of reduced ROM of the ankle.
Conclusion
PVNS is certainly an uncommon cause of anterior ankle impingement, but it can be clearly diagnosed at clinical and MRI investigation. Early diagnosis and surgical excision is recommended to prevent extension of the mass, cartilage damage, and a painful limitation of dorsal flexion of the ankle.
Clinical Message
Althought uncommon, pigmented villonodular synovitis should be kept in mind in case of anterior ankle impingement. It can be diagnosed with clinical and MRI investigation. Early surgical excision is recommended.
References
1. Myers BW, Masi AT. Pigmented villonodular synovitis and tenosynovitis: A clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore) 1980;59:223-38.
2. Granowitz SP, Mankin HJ. Localized pigmented villonodular synovitis of the knee. Report of five cases. J Bone Joint Surg Am 1967;49:122-8.
3. Chassaignac M. Cancer de la gaine des tendons. Gas Hosp Civ Milit1852;47:185-90.
4. Jaffe HL, Lichtenstein L, Sutro CJ. Pigmented villonodular synovitis, bursitis and tenosynovitis. A discussion of the synovial and bursal equivalents of the tenosynovial lesion commonly denoted as xanthanoma, xanthogranuloma, giant cell tumor or myeloplaxoma of the tendon sheath, with. Arch Pathol1941;31:731-65.
5. Saxena A, Perez H. Pigmented villonodular synovitis about the ankle: A review of the literature and presentation in 10 athletic patients. Foot Ankle Int 2004;25:819-26.
6. Ray RA, Morton CC, Lipinski KK, Corson JM, Fletcher JA. Cytogenetic evidence of clonality in a case of pigmented villonodular synovitis. Cancer 1991;67:121-5.
7. Loriaut P, Djian P, Boyer T, Bonvarlet JP, Delin C, Makridis KG, et al. Arthroscopic treatment of localized pigmented villonodular synovitis of the knee. Knee Surg Sports TraumatolArthrosc2012;20:1550-3.
8. Rochwerger A, Groulier P, Curvale G, Launay F. Pigmented villonodular synovitis of the foot and ankle: A report of eight cases. Foot Ankle Int 1999;20:587-90.
9. Al-Nakshabandi NA, Ryan AG, Choudur H, Torreggiani W, Nicoloau S, Munk PL, et al. Pigmented villonodular synovitis. Clin Radiol2004;59:414-20.
10. Horger M, Vogel M, Schmit M, Wehrmann M. Imaging in pigmented villonodular synovitis. Rofo2007;179:97-9.
11. Blanco CE, Leon HO, Guthrie TB. Combined partial arthroscopic synovectomy and radiation therapy for diffuse pigmented villonodular synovitis of the knee. Arthroscopy 2001;17:527-31.
 |
 |
 |
 |
 |
| Dr. Federico Morelli | Dr. Giorgio Princi | Dr. Alessio Rossato | Dr. Raffaele Iorio | Dr. Andrea Ferretti |
| How to Cite This Article: Morelli F, Princi G, Rossato A, Iorio R, Ferretti A. Pigmented villonodular synovitis: A rare case of anterior ankle impingement. Journal of Orthopaedic Case Reports 2020 Jan-Feb;10(1): 16-18. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com