[box type=”bio”] Learning Point of the Article: [/box]
Pre-surgical planning for sacroiliac joint arthrodesis is particularly important for patients with sacral dysmorphism induced by lumbosacral transitional vertebrae.
Case Report | Volume 10 | Issue 1 | JOCR January – February 2020 | Page 54-57 | Daisuke Kurosawa, Eiichi Murakami, Toshimi Aizawa, Takashi Watanabe0, Hiroshi Ozawa. DOI: 10.13107/jocr.2020.v10.i01.1634
Authors: Daisuke Kurosawa[1], Eiichi Murakami[1], Toshimi Aizawa[2], Takashi Watanabe[3], Hiroshi Ozawa[4]
[1]Department of Orthopaedic Surgery, Low Back Pain and Sacroiliac Joint Center, JCHO Sendai Hospital, Sendai, Japan,
[2]Department of Orthopaedic Surgery, Tohoku University School of Medicine, Sendai, Japan,
[3]Department of Hospital Medicine, JCHO Sendai Hospital, Sendai, Japan,
[4]Department of Orthopaedic Surgery, Tohoku Medical and Pharmaceutical University School of Medicine, Sendai, Japan.
Address of Correspondence:
Dr. Daisuke Kurosawa,
Department of Orthopaedic Surgery, Low Back Pain and Sacroiliac Joint Center, JCHO Sendai Hospital, 3-16-1 Tsutsumi-machi, Aoba-ku, Sendai, Japan.
E-mail: d-kurorin@m3.dion.ne.jp
Abstract
Introduction: Lumbosacral transitional vertebrae (LSTV) can cause sacral dysmorphism. Sacroiliac joint (SIJ) arthrodesis has been widely performed as the last resort for severe SIJ pain. We report three kinds of technical pitfalls identified in the surgical records of SIJ arthrodesis for the patients with sacral dysmorphism induced by LSTV.
Case Report: For the cases of a 34-year-old man with LSTV Castellvi’s Type IV, anterior SIJ arthrodesis using a plate and screws was performed. The most cranial sacral foramen was larger and irregularly round, and the nerve root ran to the lateral side from the deformed foramen more than usual. A firm medial traction of the nerve root together with the psoas major muscle for the purpose of attaching a plate and inserting screws on the sacrum side could cause the temporary radiculopathy. For a 26-year-old woman with a thin sacral alar due to IIIb, SIJ arthrodesis using multi screws with the posterolateral approach was performed. The most cranial screw penetrated the anterior margin of the sacrum and caused nerve root injury. For a 35-year-old man with Ib, posterior SIJ arthrodesis was attempted using screws and cylinder cages. The insertion of the implants using the posterior approach was technically challenging due to the small size of the sacrum.
Conclusions: Pre-surgical planning for SIJ arthrodesis, including a surgical approach, is particularly important when we see patients with sacral dysmorphism induced by each type of LSTV. The presented surgical pitfalls will be valuable when surgeons perform SIJ arthrodesis for patients with LSTV.
Keywords: Sacroiliac joint, lumbosacral transitional vertebrae, arthrodesis, pitfall.
Introduction
The sacroiliac joint (SIJ) is increasingly recognized as a significant cause of low back pain and leg symptoms [1]. Recently, SIJ arthrodesis has been widely performed to the patients with painful SIJ due to the development of new fixation products [2, 3]. Lumbosacral transitional vertebrae (LSTV) are congenital anomalies showing either sacralization of the lowest lumbar segment or lumbarization of the superior sacral segment of the spine. LSTV could cause sacral dysmorphism combined with sacroiliac articular morphological changes [4]. During the SIJ arthrodesis through the anterior, posterolateral, or posterior approach, we have occasionally experienced technical pitfalls in patients with sacral dysmorphism induced by LSTV. It should be very important to know whether there are sacral dysmorphism and LSTV in SIJ surgery. Here, we reported three kinds of pitfalls related with such dysmorphism and discussed the causes.
Case Report
The LSTV were evaluated based on Castellvi’s classification [5].
Case 1
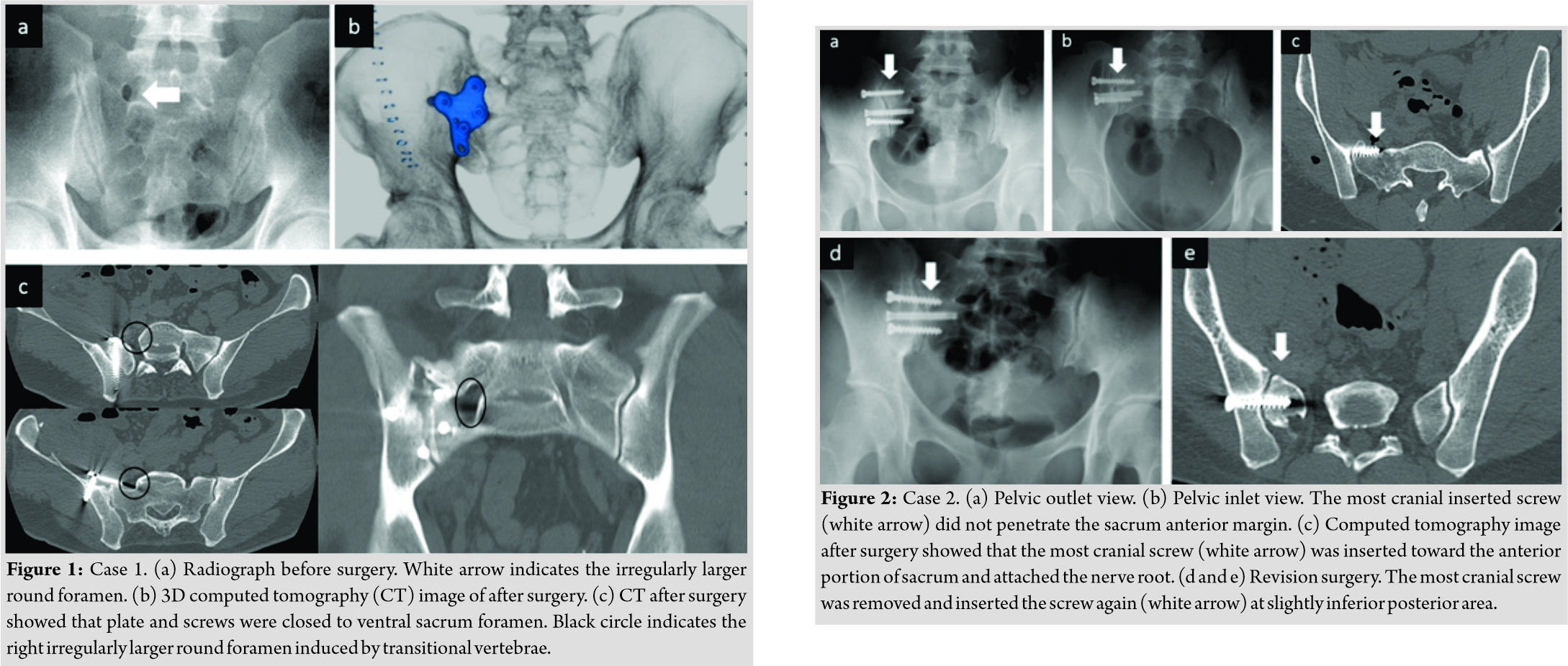
A 34-year-old man exhibited bilateral SIJ pain. The patient had LSTV Type Ⅳ, which manifested itself on the right side of the diarthrodial joint. A definitive diagnosis of SIJ pain was confirmed by SIJ injections. Fluoroscopy-guided local anesthetic injections performed on the right side of the diarthrodial joint were less effective than those in the SIJ. Conservative therapies performed for 9 months provided only temporary relief of his symptoms. His SIJ pain was more severe on the right. First, we attempted to fix the right SIJ using the anterior approach. Through a pararectal approach [6], the upper anterior surface of the SIJ was exposed between the psoas major muscle and the iliac muscle. A femoral nerve was retracted laterally toward the iliac muscle. The psoas major muscle was retracted medially to attach a plate and to insert screws on the sacrum side. Usually, the nerve root from the S1 ventral foramen was not exposed while retracting the psoas major muscle. However, in this surgery, the nerve root ran from the irregularly larger round foramen to the lateral side more than usual, and therefore, the nerve root was exposed (Fig. 1). Gently retracting the nerve with the psoas major muscle medially was needed to prevent nerve injury. After surgery, he complained of temporary right leg pain and numbness. We confirmed that the symptoms were radiculopathy by seeing complete pain relief just after selective nerve root block. Moreover, using selective nerve root contrast medium infiltration, we also confirmed that the nerve root did not come into contact with the plate.
Case 2
A 26-year-old woman had right SIJ pain and LSTV Type IIIb. A definitive diagnosis of SIJ pain was confirmed by SIJ injections. Conservative therapies done for 3 years and 2 months could not relieve her symptoms. We performed SIJ arthrodesis inserting three cancellous screws using the posterolateral approach. In this surgery, the sacral alar was thinner than usual due to sacral dysmorphism induced by LSTV. Therefore, the most cranial sacral vertebral body for the most cranial screw was relatively small. It was confirmed that all three screws had not penetrated the anterior margin of the sacrum under the inlet view. However, after surgery, the patient complained of the right buttock and lower extremity pain. Computed tomography (CT) imaging showed that the most cranial screw penetrated the anterior margin of the sacrum and attached to the nerve root. Immediately, the screw was removed and reinserted in a slightly posterior area (Fig. 2). In this case, the anterior margin of the small cranial portion of the sacrum was not shown clearly by inlet view during surgery due to overhanging the anterior margin of the caudal portion of the sacrum (Fig. 3).
Case 3
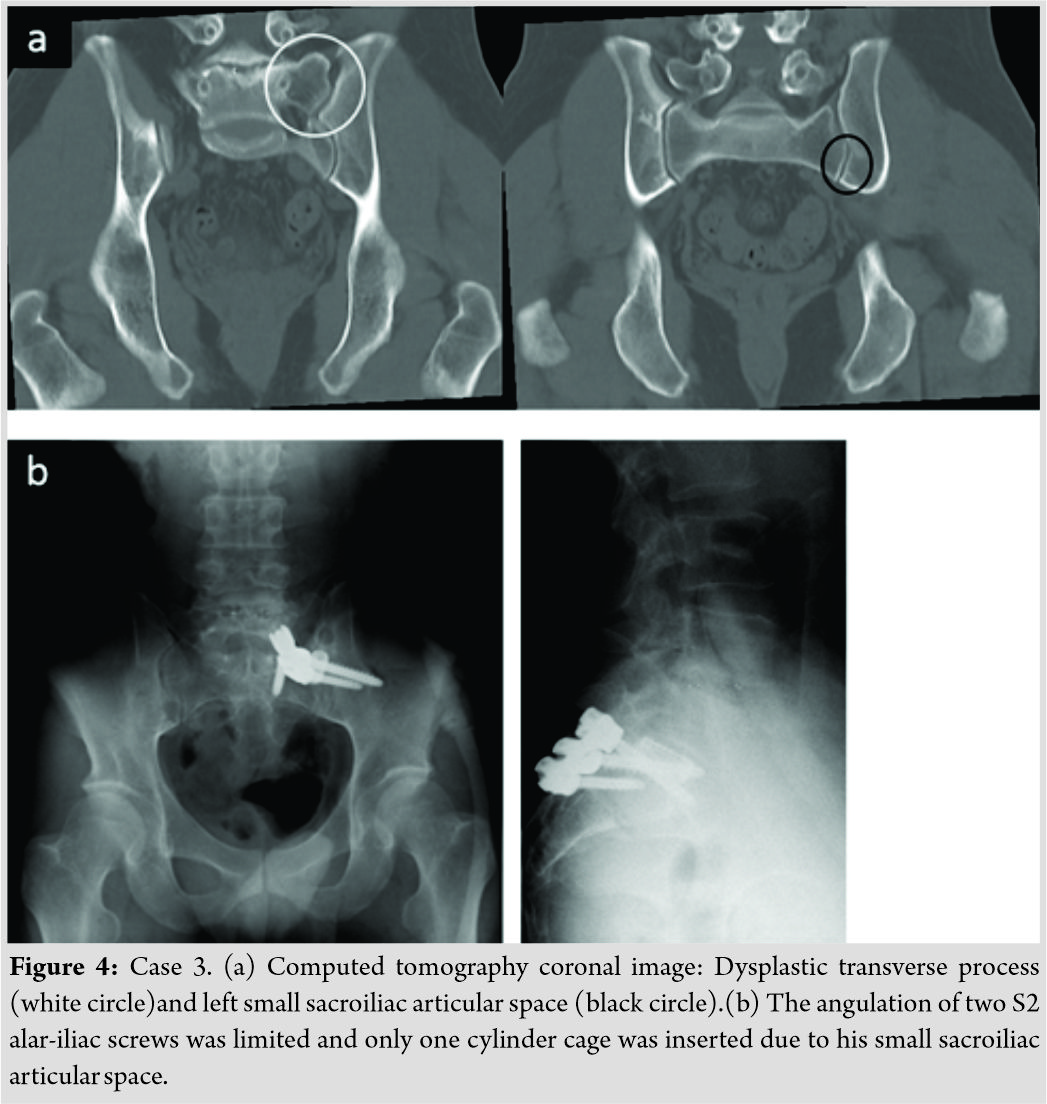
A 35-year-old man had the right SIJ pain and had LSTV Type Ib. A definitive diagnosis of SIJ pain was confirmed by SIJ injections. Conservative therapies performed for 8 months could not relieve his symptoms. We attempted to perform SIJ arthrodesis with the posterior approach using an S1 pedicle screw, two S2 alar-iliac screws, and two cylinder cages. In this anomaly, the sacrum was very small. The angulation of two S2 alar-iliac screws was limited due to the patient’s small sacroiliac articular space. When we connected the heads of the three screws (one S1 pedicle screw and two S2 alar-iliac screws) with the rod, the three screw heads were tightly touching each other due to the posterior narrow sacral space (Fig. 4). The S1 pedicle screw should have been inserted more cranially in this case when there was a lack of space to insert the other two screws. For this patient, only one cylinder cage could be inserted in the joint.
Discussion
We have experienced all approaches for SIJ arthrodesis in the past 20 years (Fig. 5). In surgical procedures of anterior SIJ arthrodesis, the psoas major muscle is retracted medially to attach a plate and to insert screws on the sacrum side [6]. In LSTV Type Ⅳ in our series, most cranial sacrum foramen was larger and irregularly round, and the nerve root ran to the lateral side from the deformed foramen more than usual. The psoas major muscle should be retracted gently to attach a plate in patients with this kind of anomaly. In LSTV Types Ⅱ, Ⅲ and Ⅳ surgeons should know the risk of nerve injury due to the nerve running changes from a deformed sacrum foramen if they use the anterior approach. Particularly, in Types Ⅱ and Ⅳ, most cranial sacrum foramen tends to be larger and irregularly round on the diarthrodial side. When we use the posterolateral approach for SIJ arthrodesis with multi screws or triangular titanium implants [3], we should pay attention to prevent the screw/implant from penetrating the anterior margin of the sacrum. For this purpose, intraoperative C-arm imaging which included a pelvic inlet view, outlet view, and lateral view was crucial. Particularly, it was important to prevent screws from being inserted toward the pelvic cavity by checking that the tip of the screw did not penetrate the anterior margin of the sacrum in the inlet view. In our Case 2, however, the most cranial screw penetrated the anterior margin of the sacrum, which caused S1 radiculopathy. As the cranial sacral body (sacral alar) could be thinner than usual when the patients had any type of LSTV except for Type Ⅰ, the inlet view is not enough to insert the most cranial screw safely. In such situation, the lateral pelvic view is more credible [7]. Pre-surgical planning to determine the implant insertion point is necessary based on the CT image, particularly in the sagittal plane. Intraoperative CT imaging and navigation may reduce the risk of screw malposition in patients with sacral dysmorphism [8]. Regarding the posterior SIJ arthrodesis using S1 pedicle screw and S2 alar-iliac screws, we had technical difficulty when the patient had a small sacrum induced by LSTV Type I. Regretfully, in this study, it was unclear whether patients with LSTV had sacralization of L5 or lumbarization of S1 because CTs or MRIs for the whole spine were not performed. However, regardless of inaccurate identification of the spinal segment, the sacrum becomes small when the S1 vertebra seems to change toward the lumbar vertebra. Therefore, the S1 pedicle screw should insert more cranially than usual for the insertion of two S2 alar-iliac screws and two cylinder cages could not be put into the SI joint space.
Conclusion
Pre-surgical planning for SIJ arthrodesis, including a surgical approach, is particularly important when we see patients with sacral dysmorphism induced by each type of LSTV. Particularly, in Types II and IV, most cranial sacrum foramen are larger and irregularly round on the diarthrodial side. The cranial sacral body (sacral alar) is thinner than usual when the patients had any type of LSTV except for Type Ⅰ. In Type Ⅰ, the sacrum becomes small when the S1 vertebra changes into the lumbar vertebra. This study indicated three kinds of surgical pitfall in the SIJ arthrodesis for sacral dysmorphism induced by LSTV. These facts will be valuable when surgeons perform SIJ arthrodesis for patients with LSTV.
Ethical Issues
The study was approved by the Institute Review Board of JCHO Sendai Hospital. All the patients were informed that their data would be submitted for publication, and the patients provided their consent. All authors have made substantial contributions to all four categories as follows:(1) Conception and design, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be published, and (4) agree to be accountable for all aspects of the work if questions arise related to its accuracy or integrity.
Clinical Message
LSTV could cause sacral dysmorphism combined with sacroiliac articular morphological changes. There are several technical pitfalls when we perform SIJ arthrodesis for patients with sacral dysmorphism induced by LSTV. We should make a surgical plan, including surgical approaches, while considering the kind of sacral dysmorphism in each LSTV type.
References
1. Bernard TN, Classidy JD. The sacroiliac joint syndrome. Pathophysiology, diagnosis and management. In: Frymoyer JW, editor. The Adult Spine: Principles and Practice. Philadelphia, PA: Lippincott-Raven Publishers; 1997. p. 2343-63.
2. FuchsV, RuhlB. Distraction arthrodesis of the sacroiliac joint: 2-year results of a descriptive prospective multi-center cohort study in 171 patients.Eur Spine J2018;27:194-204.
3. RudolfL, CapobiancoR. Five-year clinical and radiographic outcomes after minimally invasive sacroiliac joint fusion using triangular implants.Open Orthop J2014;8:375-83.
4. MahatoNK. Pedicular anatomy of the first sacral segment in transitional variations of the lumbo-sacral junction.Spine (Phila Pa 1976)2011;36:E1187-92.
5. CastellviAE, GoldsteinLA, ChanDP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects.Spine (Phila Pa 1976)1984;9:493-5.
6. MurakamiE, KurosawaD, AizawaT. Sacroiliac joint arthrodesis for chronic sacroiliac joint pain: An anterior approach and clinical outcomes with a minimum 5-year follow-up.J Neurosurg Spine2018;29:279-85.
7. KönigMA, SundaramRO, SavilleP, JehanS, BoszczykBM. Anatomical considerations for percutaneous trans ilio-sacroiliac S1 and S2 screw placement.Eur Spine J2016;25:1800-5.
8. KhanJM, LaraDL, Marquez-LaraA, RosasS, HastyE, PilsonHT. Intraoperative CT and surgical navigation for iliosacral screws: Technique for patients with sacral dysmorphism.J Orthop Trauma2018;32 Suppl 1:S24-5.
 |
 |
 |
 |
 |
| Dr. Daisuke Kurosawa | Dr. Eiichi Murakami | Dr. Eiichi Murakami | Dr. Takashi Watanabe | Dr. Hiroshi Ozawa |
| How to Cite This Article: Kurosawa D, Murakami E, Aizawa T, Watanabe T, Ozawa H. Pitfalls during Sacroiliac Joint Arthrodesis for Patients with Severe Sacroiliac Joint Pain: Report of Three Cases with Sacral Dysmorphism Induced by Lumbosacral Transitional Vertebrae. Journal of Orthopaedic Case Reports 2020 Jan-Feb;10(1): 54-57. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com