[box type=”bio”] Learning Point of the Article: [/box]
Desepiphysiodesis and reconstruction with autologous iliac crest apophyseal cartilage graft can be considered a valid option for the treatment of growth plate injuries.
Case Report | Volume 10 | Issue 1 | JOCR January – February 2020 | Page 70-73| Cosimo Gigante, Adriana Ivette Castaneda Martinez. DOI: 10.13107/jocr.2020.v10.i01.1642
Authors: Cosimo Gigante[1], Adriana Ivette Castaneda Martinez[1]
[1]Department of Orthopaedics, Orthopaedic Clinic, University of Padua, Via Giustiniani 2, 35128 Padua, Italy.
Address of Correspondence:
Dr. Adriana Ivette Castañeda Martinez,
Department of Orthopaedics, Orthopaedic Clinic, University of Padua, Via Giustiniani 2, 35128 Padova, Italy.
E-mail: ivette.castaneda.mtz@gmail.com
Abstract
Introduction: The term “desepiphysiodesis” consists of removing a partial premature epiphyseal closure due to the formation of an osseous bridge and replacing it by interpositional inert material; in spite of the experimental evidence supporting the efficacy of autologous cartilage as interposition material into resection cavity to permit the remaining growth, this option, curiously, is not found in clinical practice and literature. Indeed, surgical treatment for partial growth injury, autogenous, fat, and non-biological grafts is most frequently transplanted after physeal bar resection to prevent and/or correct angular deformities.
Case Report: This is a case report of a 10-year-old boy with an angular defect of the right distal radial growth plate which was the result of a post-traumatic lesion. The bone bridge was resected and replaced with an autologous block from the apophyseal cartilage of iliac crest.
Conclusion: We are aware of this is the second case reported, in which autologous physeal graft was successfully used, observing a satisfactory long-term evolution of the patient. This research shows that the treatment of growth arrest with autologous iliac crest apophyseal cartilage graft is an effective method that can yield excellent results.
Keywords: Physeal bar resection, iliac crest, angular deformity.
Introduction
The different patterns of growth plate injury have been classified by Salter and Harris in 1963. They divided these injuries into five types. The Type 5 results of a crushing force-producing longitudinal compression of the physis, which damaged the germinal layer of physeal cells, causing growth arrest [1]; the most common physeal fracture site is finger phalanges (37.4%) followed by the distal radius (17.9%) [2].
Although most of these fractures heal without complication, some result in partial or complete physeal arrest with a formation of a bone bridge. This is usually localized to one part of the physis and results either in progressive shortening or a combination of shortening and progressive deformity [3]. Surgical treatment depends on the bridge size and location. Bone bridges that comprise <50% of the physeal area may be treated successfully with bridge excision and interposition of inert material, autogenous fat, and non-biological grafts are clinically transplanted after bony bridge resection. This procedure prevents the progression of disordered growth and has been devised by Langenskiöld (1967), following resection of the bony tether, interposition of fat, and additional osteotomy is, therefore, required to correct the deformity [4]; in spite of the experimental evidence supporting the efficacy of autologous cartilage as interpositional material in desepiphysiodesis, this option is not found in clinical practice and literature.
We report a case of a 10-year-old boy patient with a post-traumatic distal radius growth arrest that was treated with physeal bar resection and reconstruction of the physis by autologous cartilage of the iliac crest.
Case Report
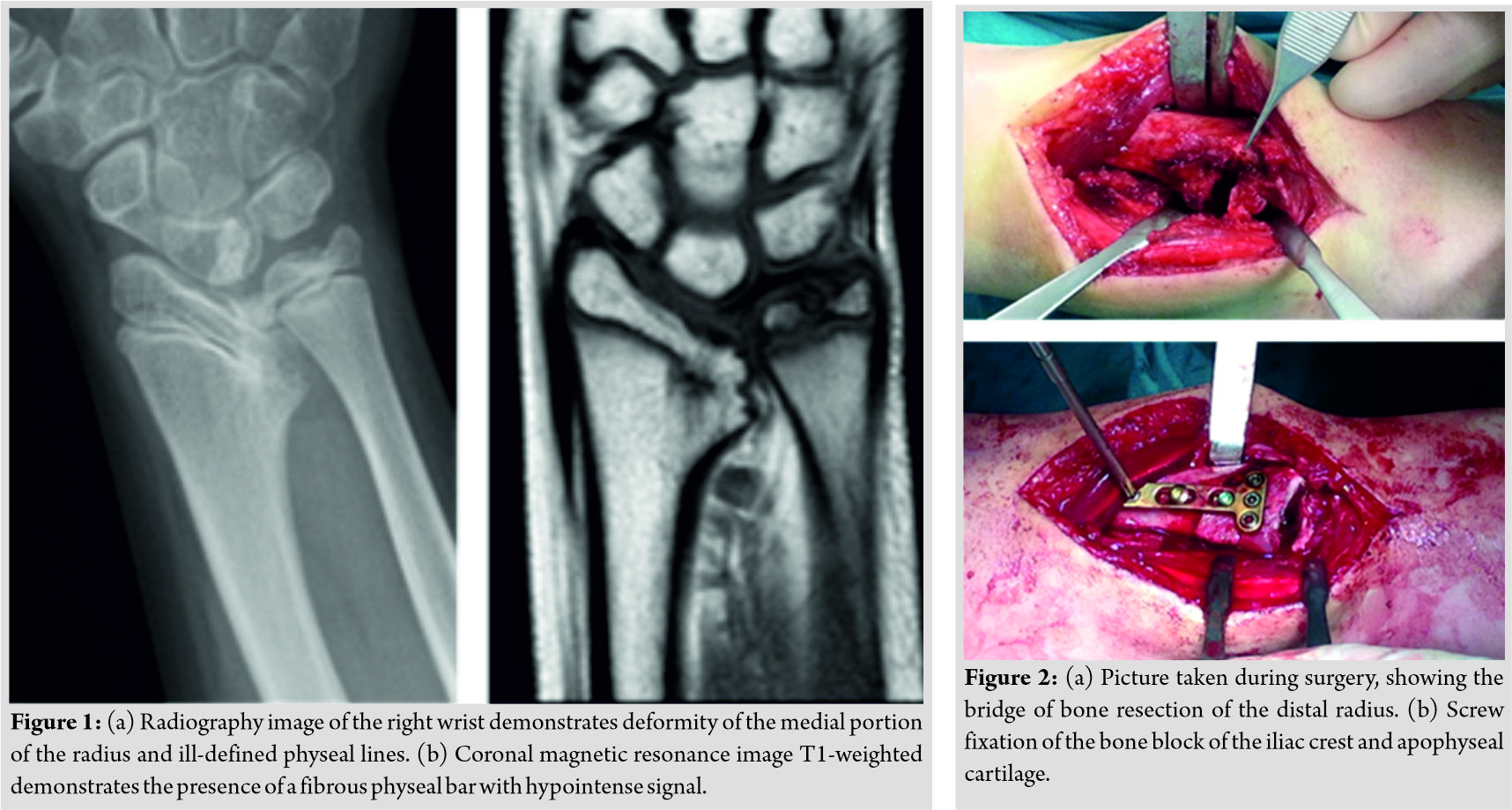
A 10-year-old boy with a history of right distal radius trauma without medical attention that came at our service 2 years later because of a progressive deformity of the wrist; he has not previous image studies. Radiography on admission showed a marked deformity at the medial border of the right distal radius at the level of the distal radioulnar joint due to the formation of a small bony bridge between epiphysis and metaphysis at the site of fracture (Fig. 1). Physical examination revealed the limitation of pronation/supination of the forearm. Neurologic and vascular examination was unremarkable.
Magnetic resonance image sequence demonstrates the presence of fibro-osseous physeal bar with hypointense signal, besides angular deformity of the radius.
When the boy was 12 years old, the bone bridge was resected and replaced with an autologous block from the apophyseal cartilage of iliac crest. The cartilaginous transplant was oriented such as the side of the graft closer to the bony iliac crest was placed in direct contact with the metaphysis of the radius. The angular deformity was corrected by an osteotomy followed by plate fixation (Fig. 2).
Post-operative radiography, taken at 5 weeks, showed consolidation of the osteotomy. During the follow-up, the continuity of the open physis and the progressive lengthening of the right distal radius was documented by X-rays (Fig.3). The plate and screws were removed at 12 months. At follow-up, 4 years after surgery, the range of movement in both wrists was symmetrical (Fig. 4). 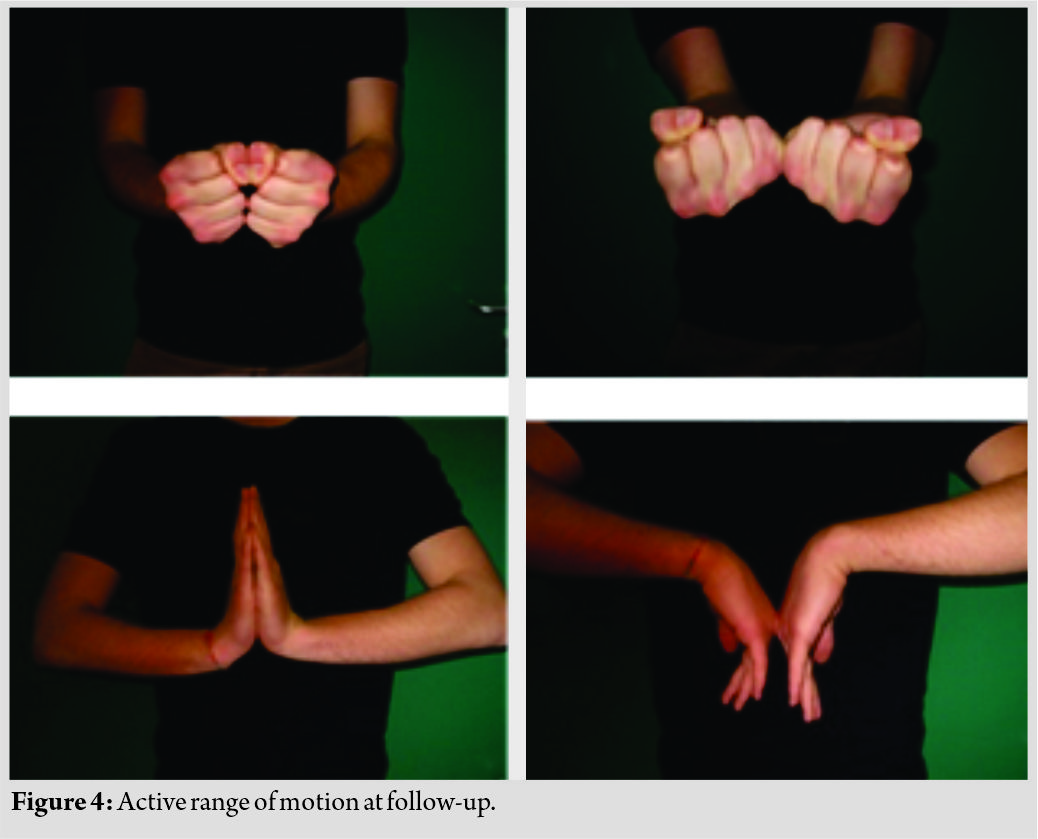
Discussion
Once it has been established that the previous growth plate injury has caused a progressive defect of growth, surgical treatment may be assistance. The technique described is based on experimental observations (Table 1).
Langenskiöld first described the principles of growth plate arrest and resection in 1967. He showed that following growth plate injury, the formation of a bony bar between the epiphysis and the metaphysis can be prevented by interposition material. Langenskiöld used fat as an interposition material [4].
Österman (1972) found that the reformation of a resected bone bridge was prevented by replacement with autogenous fat [5].
Bright (1974) found that the reformation of a bridge may be prevented by the interposition of silicone rubber [6].
The term “desepiphysiodesis” is used by French authors to describe this operation, with the aim of preventing and correcting axial deviation, and shortening of the affected limb; using the surgical technique introduced in France by Mallet, which consists of resecting the osseous bridge of epiphysiodesis and replacing it by a “plug” of interpositional inert material[7].
Mallet (1978) reported five cases of post-traumatic partial epiphysiodesis treated by surgical resection of the bony bridge and interposition of acrylic cement to avoid recurrence; corrective osteotomy was also performed[8].
After Langenskiöld’s report, surgical treatments for human using various grafts to prevent the bony bridge reforming were reported such as methyl methacrylate [8, 9], synovial chondrocytes and mesenchymal stem cells [10], and bone wax [11]. However, there are no available reports enough on the regeneration of injured growth plate cartilage in humans.
The experimental work published by Eulert et al.(1979) demonstrated good results with replacement of a long bone epiphysial plate by iliac crest cartilage in 279 rabbits. Nearly, all transplants showed increasing growth [12].
The above was confirmed by Olin et al. (1984), who based on an experimental study, developed a procedure to transplant-free autogenous iliaccrest physeal grafts into defects of the distal femoral physis of rabbits. This study demonstrated that transplantation of an iliaccrest physis into a defect of the lateral aspect of the distal femoral physis can prevent bonebridge formation, growth arrest, and the development of valgus deformity. The iliac apophysis is composed of a fibrocartilaginous layer, cartilage similar to epiphyseal cartilage, and a physis. The graft included the physis and some overlying epiphyseal cartilage, and the fibrocartilaginous layer and perichondrium were removed because these two tissues were believed to inhibit diffusion. The transplanted physis participated in endochondral bone formation [13].
Based on some previously reported experimental observations, it was decided for the graft placement of autologous apophyseal cartilage, following the resection of the bone block and the corrective osteotomy of the radius. Our radiographic results showed realignment of the angular deformity and restarting of the physeal growth at the site of the bone block; this suggests that the growth plate has potential to be partially repaired by the transplantation of autologous apophyseal cartilage of iliac crest.
In our knowledge, this is the second case reported in literature, in which autologous physeal graft was successfully used, observing a satisfactory long-term evolution of the patient.
A combination of procedures may be required to obtain the length and correct alignment of disordered growth caused by physeal injury in the younger patient.
When the most reasonable choice is that of “desepiphysiodesis,” the interposition of autologous iliac apophyseal cartilage would seem to offer, on clinical and experimental bases, greater probability of success than other conventional interposition materials and should be preferred.
Conclusion
Physeal bar resection is an important tool to consider in treating children with an acquired limb deformity. Apophyseal cartilage of iliac crest could be a long-term, safe, and adequate graft for the treatment of growth plate injuries.
Clinical Message
This research shows that the treatment of growth arrest with autologous iliac crest apophyseal cartilage graft is an effective method that can yield excellent results, being an option to consider in the treatment of deformity secondary to growth plate injury.
References
1. Salter RB, Harris WR. Injuries involving the epiphyseal. Plate Bone Joint Surg 1963;54:587.
2. Peterson HA, Madhok R, Benson JT, Ilstrup DM, Melton LJ 3rd. Physeal fractures: Part 1. Epidemiology in Olmsted county, Minnesota, 1979-1988. J PediatrOrthop1994;14:423-30.
3. Evans GA. Management of disordered growth following physeal injury. Injury 1990;21:329-33.
4. Langenskiöld A. The possibilities of eliminating premature partial closure of an epiphyseal plate caused by trauma or disease. Acta OrthopScand1967;38:267.
5. Osterman K. Operative elimination of partial premature epiphyseal closure. An experimental study. Acta OrthopScand Suppl 1972;147:3-79.
6. Bright RW. Operative correction of partial epiphyseal plate closure by osseous-bridge resection and silicone-rubber implant. J Bone Joint Surg Am 1974;56:655.
7. Bronfen C, Rigault P, Glorion C, Touzet P, Padovani JP, Finidori G, et al desepiphysiodesis–elimination of partial premature epiphyseal closure. experience of 17 cases. Eur J Pediatr Surg 1994;4:30-6.
8. Mallet J. Traitementdesèpphysiodèsespartiellestraumatiques chez l’enfant par dèsèpiphysiodèse. Int Orthop (SICOT) 1978;1:309-15.
9. Peterson HA. Partial growth plate arrest and its treatment. JPediatrOrthop1984;4:246.
10. Otsuki D, Yoshida K, Kobayashi M, Hamano D, Higuchi C, Yoshikawa1 H, et al. Costal cartilage transplantation for treatment of growth plate. Injury in a rabbit model. J Child Orthop2017;11:20-7.
11. Yoshida T, Kim WC, Tsuchida Y, Hirashima T, Oka Y, Kubo T, et al. Experience of bone bridge resection and bone wax packing for partial growth arrest of distal tibia. J Orthop Trauma 2008;22:142-7.
12. Eulert J, Floetemeyer E, Winkler G. Remplacementd’une plaque épiphysaire des os longs par du cartilage de la crêteiliaque Etude expérimentale. Ann Chir1979;33:9-16.
13. Olin A, Creasman C, Shapiro F. Free physeal transplantation in the rabbit. An experimental approach to focal lesions. J Bone Joint Surg Am 1984;66:7-20.
 |
 |
| Dr. Cosimo Gigante | Dr. Adriana Ivette Castaneda Martinez |
| How to Cite This Article: Gigante C, Martinez AIC. Desepiphysiodesis and Reconstruction of the Distal Radial Growth Plate with an Autologous Iliac Crest Cartilage Graft: A Case Report and Review of Literature. Journal of Orthopaedic Case Reports 2020 Jan-Feb;10(1): 70-73. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com