[box type=”bio”] Learning Point of the Article: [/box]
Every physician needs to keep in mind, while treating a tumor-like lesion, that a thorough and patient clinico laboratory examination needs to be performed before concluding to a diagnosis.
Case Report | Volume 10 | Issue 1 | JOCR January – February 2020 | Page 82-85 | S Papastergiou, D Grammatikopoulou, E Iosifidou, C Manika, D Metaxiotis, R Romanidis, K Tsitouridis. DOI: 10.13107/jocr.2020.v10.i01.1648
Authors: S Papastergiou[1], D Grammatikopoulou[1], E Iosifidou[2], C Manika[3], D Metaxiotis[2], R Romanidis[2], K Tsitouridis[2]
[1]Department of Orthopaedic, General Hospital of Thessaloniki “Agios Pavlos,” Thessaloniki, Greece,
[2]Department of Radiology, General Hospital of Thessaloniki “Agios Pavlos,” Thessaloniki, Greece,
[3]Department of Orthopaedic, General Hospital of Thessaloniki “Papageorgiou” and Elepap, Thessaloniki, Greece.
Address of Correspondence:
Dr. D Grammatikopoulou,
Department of Orthopaedic, General Hospital of Thessaloniki “Agios Pavlos,” Thessaloniki, Greece.
E-mail: danaigram87@yahoo.gr
Abstract
Introduction: Sports-related recurrent injuries (microtrauma and trauma) of the apophyses are common in children and adolescents and could result in specific pathologies. One of them is the apophysitis or apophysiolysis of ischial tuberosity (Valtancoli or Kremser’s disease) due to contraction of hamstrings, in sports with sudden accelerations and decelerations.
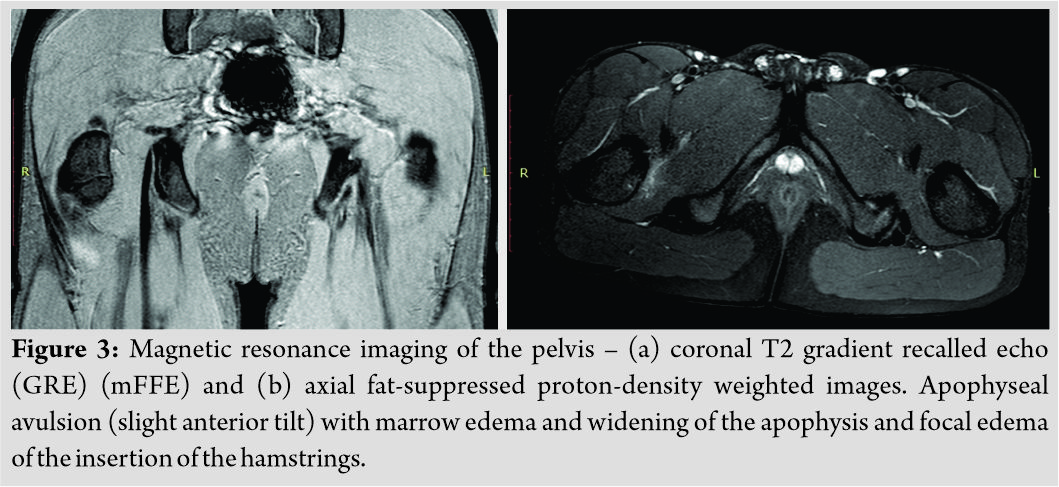
Case Report: We present the case of a male athlete who complained of pain in the left buttock and difficulty walking after a 3 months old reported trauma with pain and hematoma in his left thigh, during a kick with his contralateral leg. Due to a radiographic finding of a suspicious lesion near his left ischial tuberosity, an extensive investigation that included computed tomography, magnetic resonance imaging, bone scintigraphic scan, and blood analysis followed the diagnosis of apophysitis of the ischial tuberosity was determined and the proposed non-surgical treatment had satisfactory results.
Conclusion: The diagnosis of apophysitis of ischial tuberosity is usually delayed but has a good response to the appropriate treatment.
Keywords: Apophysitis, ischial tuberosity, teenage athlete.
Introduction
The immature skeleton is vulnerable to injury during sport activities, especially when caution is not practiced when putting together and following an appropriate training regime. About 15% of all adolescent injuries are to the physes and apophyses [1]. Apophysis is the secondary ossification center located where major tendons attach to bone and provide shape and contour to growing bone but do not add significantly to longitudinal growth. Apophysitis is a tuberosity stressed in traction; epiphysitis is a compression or shear injury, whereas epiphyseolysis is the widening of a growth plate under stress [2, 3]. The ischial apophysis is the secondary ossification center forming the ischial tuberosity, it appears between the ages of 13 and 15 years and fully fuses with the rest of the pelvis between the age of 15 and 25 years [3, 4]. Traumatic events and repetitive microtrauma are the basis for ischial apophysitis, the most common of the apophyseal injuries of the pelvis [5]. In the skeletally immature athlete, the epiphyseal plate is 2–5 times weaker than the adjacent tendon or bone and is, therefore, susceptible to injury due to musculotendinous traction during athletic activities requiring violent or repetitive strenuous muscular contractions [2]. The hamstring complex, that is comprised long, strong biarticular muscles, originates by a strong bony attachment to the ischial tuberosity and inserts distally below the knee. The semitendinosus and the long head of biceps femoris begin in a common proximal tendon with a crescent-shaped footprint at the mid-portion of the ischium and the semimembranosus begins laterally and anteriorly with a flattened tendon which continues in an equally flattened muscle [6, 7]. To specify, apophysitis or even avulsion fractures can occur with contractions of the hamstrings with the hip flexed and the knee extended during the swing phase of gait passive lengthening of hamstrings[3]. On the other hand, after the apophysis is closed in adults, the same mechanism of injury will yield a severe muscle tear rather than an avulsion. The presentation is rarely dramatic. Usually, a pop is felt, severe pain follows. An antalgic pose is adopted with the hip in extension and the patient complains of difficulty walking and sitting for a prolonged time. During clinical examination, loss of muscular function, hematoma, edema, and tenderness over the ischial tuberosity are present [3, 5]. On plain radiographs, typically, there is asymmetry of the ischial tuberosities in apophysitis; the involved apophyseal area becomes sclerotic, wider than the non-symptomatic apophysis, and later on, osteoporotic patches develop and the lower margin of the ischial tuberosity becomes irregular. The patients with avulsion report an acute trauma at the beginning of the symptoms and an avulsion fragment is seen in plain radiographs, either immediately after injury or later. A small bony or periosteal avulsion sometimes grows to a pseudotumor calcification [8]. Healing avulsions can have an aggressive appearance, including lytic lesions and areas of destruction [9]. For a more sensitive diagnostic approach, magnetic resonance imaging (MRI), bone scintigraphy, and, even, biopsy are employed. In MRI, apophysitis usually presents with widening of the apophysis and increased signal intensity in the apophysis and adjacent bone marrow and soft tissue [2]. Nuclear scintigraphy findings in apophysitis are non-specific. Increased radiotracer uptake in the apophysis on blood pool and delayed images has been described [10]. Histologic findings in apophysitis are described as increased osteoblastic activity, edema, proliferation of benign spindle cells and small vessels in the intertrabecular spaces, and inflammatory cell infiltration [11]. Sports with sudden accelerations and decelerations, competitive athletic endeavors, decreased quadriceps flexibility, a larger stride, low hamstring/quadriceps ratio, muscle fatigue, hamstring tightness, previous injury, and periods of rapid growth are a few of the risk factors for apophysitis and avulsion fractures of the ischial tuberosity [6]. Differential diagnosis includes acute and old bony or periosteal avulsions of the ischial tuberosity, apophyseolysis of the ischial tuberosity, painful unfused ischial apophysis, apophysitis of the ischiopubic junction (Van Neck disease), adult tug lesion, hamstring syndrome, proximal hamstring tendinopathy, and ischial bursitis and, in rare cases, infection or tumor, such as Ewing’s sarcoma, lymphoma, or an osteosarcoma [12,13].
Case Report
In July 2018, a 14-year and 9-month-old Caucasian male patient, in good general health, presented with an onset of acute pain while attempting a kick with his contralateral leg during an amateur football match. He, also, noticed that an ecchymosis in the dorsal aspect of the left thigh formed shortly after the traumatic event. He presumed, with no medical consultation, that the acute event was a muscle tear of the hamstrings and dealt with it as such. In September 2018, he consulted an orthopedic surgeon complaining of pain in the dorsal aspect of the left thigh and buttock for 3 months and difficulty walking, resulting in a slight limp.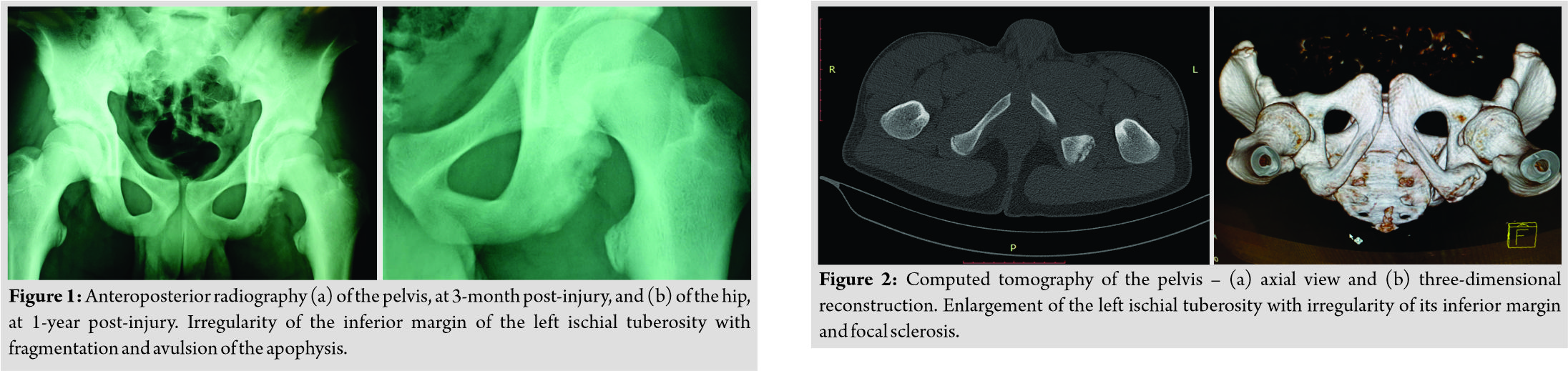
Discussion
Avulsion fracture and apophysitis of ischial tuberosity has been described many times for many years [14, 15]. The mean age of the patients with apophysitis (14.1 years) is lower than that of the subjects with avulsions (18.9 years) [8]. Due to its mild presentation, in most of the cases, the diagnosis is delayed, usually by several months. Non-surgical treatment is sufficient in most cases and the patient makes a full recovery and can resume previous physical activities. In rare cases, a surgical approach becomes crucial. Operative treatment is indicated in a painful fibrous non-union or avulsion fracture or detachment of hamstrings insertion more than 2 cm and/or great loss of function, especially in patients with high physical demands [3].
Conclusion
Many patients remain undiagnosed and continue pursuing their athletic recreation. This chronic irritation can result in hamstring syndrome, chronic posterior thigh pain, and severe loss of function [5]. Early diagnosis and appropriate treatment is the key for a full recovery and return to sports.
Clinical Message
The orthopedic clinician should always be vigilant. In our case, the young athlete suffered from benign disease, but the radiological irregularities were investigated. Even though his treatment was satisfactory without surgical intervention, his condition was diagnosed and the patient was given the tools to be in charge of his own musculoskeletal health from this point on. We need to remind clinicians that the mildness of a disease does not exclude a condition from having severe to catastrophic complications.
References
1. Pill SG, Flynn JM, Ganley TJ. Managing and preventing overuse injuries in young athletes: Early detection is vital to minimizing damage and long-term consequences. J Musculoskel Med 2003;20:434-42.
2. ArnaizJ, PiedraT, deLucas EM, ArnaizAM, PelazM, Gomez-DermitV, et al. Imaging findings of lower limb apophysitis.AJR Am J Roentgenol2011;196:W316-25.
3. FrushTJ, LindenfeldTN. Peri-epiphyseal and overuse injuries in adolescent athletes.Sports Health2009;1:201-11.
4. BrandserEA, el-KhouryGY, KatholMH, CallaghanJJ, TearseDS. Hamstring injuries: Radiographic, conventional tomographic, CT, and MR imaging characteristics.Radiology1995;197:257-62.
5. SchoenseeSK, NilssonKJ. A novel approach to treatment for chronic avulsion fracture of the ischial tuberosity in three adolescent athletes: A case series.Int J Sports Phys Ther2014;9:974-90.
6. Carlson C. The natural history and management of hamstring injuries.Curr Rev Musculoskelet Med2008;1:120-3.
7. GuancheCA. Hamstring injuries.J Hip Preserv Surg2015;2:116-22.
8. KujalaUM, OravaS. Ischial apophysis injuries in athletes.Sports Med1993;16:290-4.
9. StevensMA, El-KhouryGY, KatholMH, BrandserEA, ChowS. Imaging features of avulsion injuries.Radiographics1999;19:655-72.
10. RockettJF. Three-phase radionuclide bone imaging in stress injury of the anterior iliac crest.J Nucl Med1990;31:1554-6.
11. YamamotoT, AkisueT, NakataniT, KawamotoT, HitoraT, MaruiT, et al. Apophysitis of the ischial tuberosity mimicking a neoplasm on magnetic resonance imaging.Skeletal Radiol2004;33:737-40.
12. MilchH. Ischial apophysiolysis: A new syndrome.Bull Hosp Joint Dis1953;14:188-93.
13. BahkWJ, BrienEW, LuckJV Jr., MirraJM. Avulsion of the ischial tuberosity simulating neoplasm a report of 2 cases.Acta Orthop Scand2000;71:211-4.
14. Berry JM. Fracture of the tuberosity of the ischium due to muscular action. JAMA 1912;59:1450.
15. McMaster PE. Epiphysitis of the ischial tubérosity: A case report. J Bone Joint Surg 1945;27:493-5.
 |
| Dr. S Papastergiou |
| How to Cite This Article: Papastergiou S, Grammatikopoulou D, Iosifidou E, Manika C, Metaxiotis D, Romanidis R, Tsitouridis K. Apophysitis of the Ischial Tuberosity: A Case Report. Journal of Orthopaedic Case Reports 2020 Jan-Feb;10(1): 82-85. |
[Full Text HTML] [Full Text PDF]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com