[box type=”bio”] Learning Point of the Article: [/box]
This case report illustrates the complex, atypical healing pattern of Pagetic bone as it progresses over several decades. Considerations for orthopedic intervention in Pagetic bone are discussed.
Case Report | Volume 10 | Issue 3 | JOCR May – June 2020 | Page 19-22 | Garrett K. Berger, Alexander R. Graf, Adam N. Wooldridge, Donald A. Hackbarth. DOI: 10.13107/jocr.2020.v10.i03.1730
Authors: Garrett K. Berger[1], Alexander R. Graf[1], Adam N. Wooldridge[1], Donald A. Hackbarth[1]
[1]Department of Orthopaedic Surgery, Medical College of Wisconsin, 9200 W. Wisconsin Ave. P.O. Box 26099, Milwaukee, WI 53226-0099, Wisconsin.
Address of Correspondence:
Mr. Garrett K. Berger,
Department of Orthopaedic Surgery, Medical College of Wisconsin, 9200 W. Wisconsin Ave, P.O. Box 26099, Milwaukee, WI 53226-0099, Wisconsin.
E-mail: gkberger@mcw.edu
Abstract
Introduction: Paget’s disease (PD) is the most common metabolic bone disorder after osteoporosis. Clinically, it can result in pain, bony deformity, pathologic fractures, and, in the late stage, progression to malignancy. At a pathophysiological level, PD manifests as an imbalance between the homeostasis of bone destruction and formation. Bones most often involved with this disease process include the pelvis, femur, tibia, vertebra, and skull. The goals of orthopedic intervention in PD are two-fold: Prevention of pathologic fracture with internal stabilization and reconstruction following fracture, which is often complicated by poor bone quality and advanced deformity. In this case report, authors detail a patient with PD who presented with a pathologic left subtrochanteric femur fracture requiring a novel complex femoral reconstruction with a 29-year follow-up period. To the best of our knowledge, no such report exists, particularly with this degree of long-term follow-up.
Case Report: A 70-year-old Caucasian man with PD presented with an atypical subtrochanteric femur fracture after a ground level fall. Due to his significant femoral deformity and osteopenia, proximal femoral resection followed by composite femoral allograft reconstruction with total hip arthroplasty was performed. Long-term durability of this novel reconstruction method as well as longitudinal clinical and radiographic outcomes is described.
Conclusion: Complex pathologic fractures in patients with PD can be effectively treated with composite femoral allograft reconstruction and total hip arthroplasty with good long-term radiographic and clinical outcomes. Broadly, it is important to note the unique healing pattern seen in PD bone and to consider the implications it may have when planning surgical intervention.
Keywords: Osteitis deformans [MeSH], femoral fracture [MeSH], follow-up studies [MeSH], atypical femur fracture, Paget’s disease of the bone.
Introduction
Paget’s disease (PD), or osteitis deformans, is the second most common metabolic bone disorder after osteoporosis [1]. Its clinical characteristics include pain, bony deformities, pathologic fractures, an enlarging skull with resultant deafness, and, in the late stage, progression to malignancy [2]. Pathologically, PD is characterized by a disruption in the normal physiologic balance between bone destruction and formation. It is believed that an osteoclastic defect leads to disorganized bone resorption which, in turn, provokes suboptimal bone formation that is biomechanically weaker, more disorganized, less dense, hypervascular, and more prone to fracture and deformation under stress [3, 4, 5]. Bones most often involved with this disease process include the pelvis, femur, tibia, vertebra, and skull [6]. Orthopedic intervention in PD involving the femur is indicated both prophylactically in the setting of impending fracture and following pathologic fracture [7, 8]. In advanced disease, femoral bowing and poor bone quality pose a unique reconstructive challenge. In this case report, authors detail a patient with PD who presented with a pathologic left subtrochanteric femur fracture requiring a novel complex femoral reconstruction with a 29-year follow-up period.
Case Report
A 70-year-old retired fire fighter and World War II veteran presented to his internist with progressive left hip and thigh pain. Radiographs were obtained which showed cortical thickening, diffuse trabecular changes throughout the pelvis and femur and significant femoral bowing. Orthopedic oncology referral was made where femoral osteotomy with prophylactic fixation was planned after medical optimization. However, before medical optimization with bisphosphonate therapy, the patient suffered a pathologic left subtrochanteric femur fracture from a ground level fall. Given the patient’s poor bone stock and significant femoral deformity, composite allograft reconstruction of the proximal left femur and a total hip arthroplasty was chosen to simultaneously treat his fracture, correct his longstanding deformity, and permit early ambulation and functional independence.
Operative report
With the patient positioned in the right lateral decubitus position, an extensile posterolateral approach was performed to expose the left hip, femoral shaft, and lateral knee. The short external rotators were released from the proximal femur, the tensor fasciae latae was split, and the vastus lateralis was reflected off the femur anteriorly. A greater trochanteric osteotomy was performed to access the hip joint and a capsulotomy was performed before hip dislocation. The femoral cortex appeared thin with a grayish hue. Subperiosteal muscle release was then performed and the femur was osteotomized distal to the bowed diaphysis at the junction of the proximal ¾ and distal ¼ of the femur just proximal to the knee. Before performing the osteotomy, a dynamic condylar screw system lag screw was placed into the distal femoral condyles fitting a trial distal condylar plate for the reconstruction. The acetabulum was minimally reamed and a Howmedica Osteonics (now Stryker, Warsaw, IN) cup was inserted. A full length frozen left femoral allograft was used that matched the patient’s femoral size. It was cultured and thawed per protocol in warm saline and then in antibiotic solution. The femoral head and greater trochanter were osteotomized on the back table. The distal osteotomy was made at the appropriate level of the graft creating a step cut osteotomy in the graft with a reciprocal step cut in the residual distal femur. The proximal femoral allograft was then reamed and broached. A long-stem femoral component manufactured by Howmedica Osteonics was cemented into the allograft on the back table using three batches of tobramycin-impregnated polymethylmethacrylate cement. The composite hip arthroplasty was then internally fixed to the patient’s native distal femur using a 16-hole plate attached to the dynamic condylar lag screw. Six bicortical screws and two cancellous lag screws were placed through the plate distal to the stem and three unicortical screws were inserted through the plate proximally at the level of the femoral stem. A Dall-Miles cable was then used at distal junction site to provide stability at the allograft native femur interface.
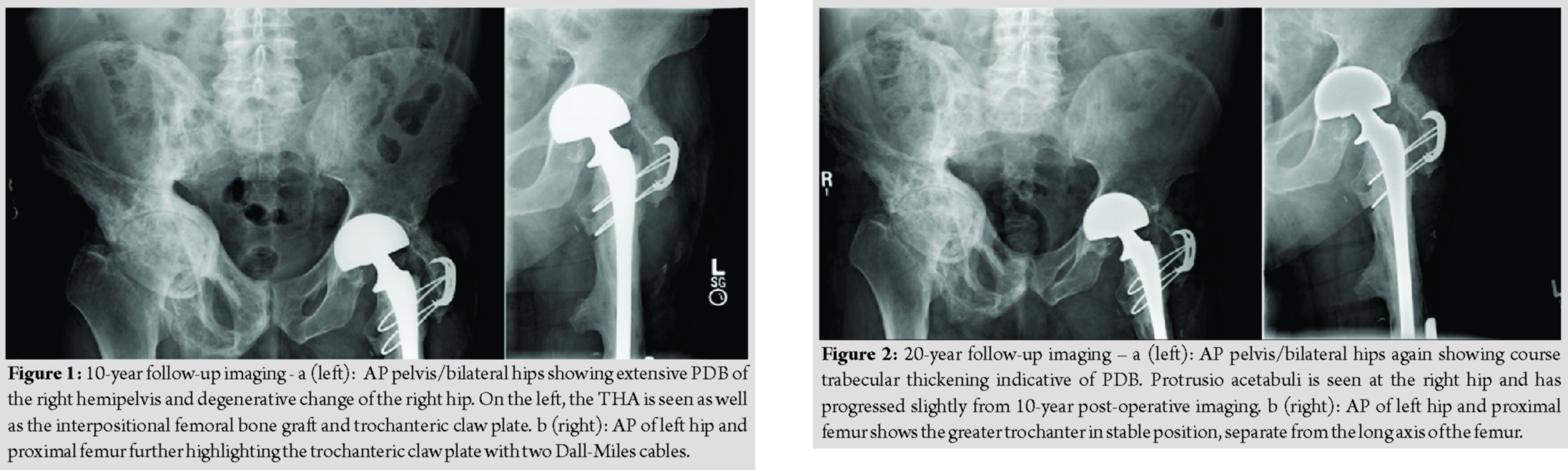
To minimize dislocation risk, a bipolar head was then attached to the femoral trunnion. The composite femoral reconstruction was then reduced and fit nicely into the acetabular component. The native greater trochanter was attached to the proximal allograft with a trochanteric claw device and two Dall-Miles cables, one of which was passed through the allograft lesser trochanter and one below it. The capsule was then repaired, and wound closure was performed in standard fashion. The patient was extubated and transferred to the inpatient floor where he followed an uneventful post-operative course. He was discharged to home after 2 weeks of inpatient rehabilitation with 60 pounds weight-bearing for 3 months. He then progressed to weight-bearing as tolerated with crutches and subsequently with a cane. He returned to full pre-operative activity levels within the 1st year. The allograft native femur junction healed robustly with a significant callus formation. The greater trochanter osteotomy, however, resulted in painless non-union. In the decade following his reconstruction, the patient’s PD progressed throughout his pelvis and left hip and began to invade the medial aspect of the allograft. He was followed by his endocrinologist who treated him with bisphosphonate therapy. He noted minimal left hip or thigh pain after the first 3 months following his reconstruction. He lived at home with his wife, walked with a cane, and cared for his home and yard (Fig. 1a and b). In the 2nd decade following his reconstruction, the invading PD on the medial aspect of the allograft remained stable. There were no signs of loosening of the cement mantle of the long-stem bipolar prosthesis, though the prosthesis itself had migrated somewhat medially. The cables remained intact but had started to cut medially into the allograft. His right hip progressed to moderate arthritis, though he did not complain of pain. He did not have any left hip pain or stiffness (Fig. 2a and b). Twenty years after his reconstruction, the patient was 90 years old and experienced only mild left hip pain worsened with activity. The patient remained relatively active and was able to ambulate independently. The greater trochanter osteotomy remained in stable, asymptomatic non-union. At the post-operative year 21 mark, the left acetabulum began demonstrating radiographic signs of wear with thinning superiorly. At the 24-year mark, the bipolar component began to exhibit signs of early acetabular protrusio. At the 28-year mark, the bipolar component developed further acetabular protrusio. During the entire period of follow-up, the cement mantle within the allograft around the femoral stem remained intact without signs of loosening or subsidence (Fig. 3a, b, c, d). At 28 years post-operative, the patient sustained a right hemispheric stroke that resulted in the left lower extremity weakness. He then transitioned to an assisted living facility. He is presently 99 years old and is mobile with a wheel chair without any left hip or thigh discomfort.
Discussion
PD is a relatively common metabolic bone disorder with significant morbidity [9, 10]. There are three classic phases of PD: Osteolytic, mixed osteoblastic/osteolytic, and sclerotic [11]. While these phases typically occur in sequence, they may be present in different phases at different bone sites. Most often, PD presents with singular bony involvement, though it may involve multiple bones. While PD may be asymptomatic, patients commonly present with bone pain, deformity and even fracture [3]. Orthopedic intervention is indicated in a variety of clinical scenarios including impending pathologic fractures, deformity correction, fracture fixation, and complex post-traumatic reconstruction, as demonstrated in this case [12, 13]. Because PD is associated with a marked increase in vascularity within the involved bone, bisphosphonate therapy is recommended for at least 6 weeks before surgery to prevent excess blood loss [12]. Massive bony allografts present unique patterns of healing, varied with junction composition (cortical-cortical, cancellous-cancellous, and cortical-cancellous) [14]. While union rates in cortical-cortical junctions occur more slowly, cancellous bone heals more rapidly as native bone develops an internal callous, invading the allograft [14]. In this case, the distal allograft native femur junction was 2 cm × 2 cm of cortical-cancellous bone. Within a few years post-operative, the junction had completely healed with no visible junction line, an atypical finding. It is likely that the increased vascularity and osteoblastic activity inherent to PD accelerated this healing period [13, 15]. This same osteoblastic activity may explain the PD from the native periosteum invading the medial cortex of the allograft resulting in the peculiar “spike” of the bone appearance. This is another finding not typically seen in allografts, except in cases of infection of chronic inflammatory states [14]. At 29 years post-operative, there was no loosening of the cement mantle around the stem. As reported by Enneking and Mindell, this is likely an advantage of the paucity of revascularization and subsequent bone resorption that is seen in the central canal of massive allografts [14].
Conclusion
Treatment of pathologic subtrochanteric femur fractures in patients with PD can be challenging, secondary to poor bone quality, increased vascularity, and complex deformity. Understanding the unique pathophysiology, pre-operative optimization using a multidisciplinary approach and careful pre-operative planning can help optimize long-term outcomes. Acceptable junctional healing can result after composite allograft reconstruction despite aberrant bone biology. This is an older technique to consider in the modern era of megaprostheses as it can provide durable pain relief and functional independence, incorporate into host bone, and leave salvage options in the future for the younger patient with this common and complex disease.
Clinical Message
This case report illustrates the complex, atypical healing pattern of Pagetic bone as it progresses over several decades. Considerations for orthopedic intervention in Pagetic bone are discussed.
References
1. Menendez-Bueyes LR, Soler Fernandez MD. Paget’s disease of bone: Approach to its historical origins. Reumatol Clin 2017;13:66-72.
2. Cundy T. Paget’s disease of bone. Metabolism 2018;80:5-14.
3. Kravets I. Paget’s disease of bone: Diagnosis and treatment. Am J Med 2018;131:1298-303.
4. Muschitz C, Feichtinger X, Haschka J, Kocijan R. Diagnosis and treatment of Paget’s disease of bone: A clinical practice guideline. Wien Med Wochenschr 2017;167:18-24.
5. Rebel A, Basle M, Pouplard A, Malkani K, Filmon R, Lepatezour A. Bone tissue in Paget’s disease of bone. Ultrastructure and immunocytology. Arthritis Rheum 1980;23:1104-14.
6. Kanis JA. Pathophysiology and Treatment of Paget’s Disease of Bone. Oxford: Taylor and Francis; 1998.
7. Hanna SA, Dawson-Bowling S, Millington S, Bhumbra R, Achan P. Total hip arthroplasty in patients with Paget’s disease of bone: A systematic review. World J Orthop 2017;8:357-63.
8. Popat R, Tsitskaris K, Millington S, Dawson-Bowling S, Hanna SA. Total knee arthroplasty in patients with Paget’s disease of bone: A systematic review. World J Orthop 2018;9:229-34.
9. Bone HG. Nonmalignant complications of Paget’s disease. J Bone Miner Res 2006;21 Suppl 2:P64-8.
10. Wermers RA, Tiegs RD, Atkinson EJ, Achenbach SJ, Melton LJ 3rd. Morbidity and mortality associated with Paget’s disease of bone: A population-based study. J Bone Miner Res 2008;23:819-825.
11. Schneider D, Hofmann MT, Peterson JA. Diagnosis and treatment of Paget’s disease of bone. Am Fam Physician 2002;65:2069-72.
12. Kaplan FS, Singer FR. Paget’s disease of bone: Pathophysiology, diagnosis, and management. J Am Acad Orthop Surg 1995;3:336-44.
13. Al-Rashid M, Ramkumar DB, Raskin K, Schwab J, Hornicek FJ, Lozano-Calderon SA. Paget disease of bone. Orthop Clin North Am 2015;46:577-85.
14. Enneking WF, Mindell ER. Observations on massive retrieved human allografts. J Bone Joint Surg Am 1991;73:1123-42.
15. Ludkowski P, Wilson-MacDonald J. Total arthroplasty in Paget’s disease of the hip. A clinical review and review of the literature. Clin Orthop Relat Res 1990;255:160-7.
 |
 |
 |
 |
| Mr. Garrett K. Berger | Dr. Alexander R. Graf | Dr. Adam N. Wooldridge | Dr. Donald A. Hackbarth |
| How to Cite This Article: Berger GK, Graf AR, Wooldridge AN, Hackbarth DA. Complex Femoral Reconstruction Following Pathologic Subtrochanteric Femur Fracture Secondary to Paget’s Disease of the Bone: A Case Report with Long-Term Follow-up. Journal of Orthopaedic Case Reports 2020 May-June;10(3): 19-22. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com