[box type=”bio”] Learning Point of the Article: [/box]
Timely diagnosis and proper management of an uncommon event of pseudoaneurysm of profunda femoris artery following fixation of intertrochanteric femoral fracture
Case Report | Volume 10 | Issue 3 | JOCR May – June 2020 | Page 53-56 | Prabhat Agrawal, Saubhik Das, Naveen Kumar. DOI: 10.13107/jocr.2020.v10.i03.1746
Authors: Prabhat Agrawal[1], Saubhik Das[2], Naveen Kumar[3]
[1]Department of Orthopaedics, All India Institute of Medical Sciences (AIIMS), Patna, India,
[2]Department of Orthopaedics, Rajendra Institute of Medical Sciences (RIMS), Ranchi, India,
[3]Department of Radiodiagnosis, Rajendra Institute of Medical Sciences (RIMS), Ranchi, India
Address of Correspondence:
Dr. Saubhik Das,
Department of Orthopaedics, Rajendra Institute of Medical Sciences (RIMS), Bariatu, Ranchi-834009,India.
E-mail:drsaubhikk@hotmail.com
Abstract
Introduction: Pseudoaneurysm of profunda femoris artery is an uncommonly reported vascular mishap after orthopedic procedures around proximal femur. Diagnostic dilemma and resulting delay are quite common due to varied clinical presentations.
Case Presentation: Herein, we report a case of a 65-year-old lady who was diagnosed in our institution with pseudoaneurysm of profunda femoris artery 3 months after getting operated for intertrochanteric fracture of right femur in a private hospital. She started having gradually enlarging painful thigh swelling of the involved limb 1 month after operation. She also developed concurrent weakness, anemia, and received multiple blood transfusions before being referred to our institution. Diagnosis was clinched with duplex ultrasound imaging and subsequent digital subtraction angiography with coil embolization was performed. She made an uneventful and speedy recovery, and doing well till the last follow-up.
Conclusion: Timely diagnosis is paramount to avoid limb- and life-threatening sequelae; surgeons should keep strong vigil to administer the timely intervention. Various preventive strategies during fixation of intertrochanteric fracture should be deployed to keep this untoward entity in abeyance.
Keywords: Intertrochanteric fracture, pseudoaneurysm, profunda femoris artery, intramedullary nailing, coil embolization.
Introduction
Intertrochanteric fractures continue to remain in the limelight to orthopedic surgeons. Despite treatment strategy, fixation methods and principles are well described and codified, various complications are frequently observed and continue to test the judgment and practice of surgeons. Among a wide array of complications, vascular misadventures are the most dreaded one which can end up in limb- or life-threatening sequelae. Pseudoaneurysm (PSA) of the profunda femoris artery (PFA) is the most common vascular insult following fixation of proximal femoral fractures, albeit it is uncommon and sparsely reported in literature [1, 2]. Here, we present a case of Intertrochanteric fracture treated with proximal femoral nailing who developed pseudoaneurysm of the PFA postoperatively and was remained undiagnosed for 3 months after the index surgery. Only a handful of cases have been reported from India; therefore, our case is believed to enrich the knowledge about this rare entity and emphasize the overwhelming need of high clinical suspicion to administer timely interventions.
Case Presentation
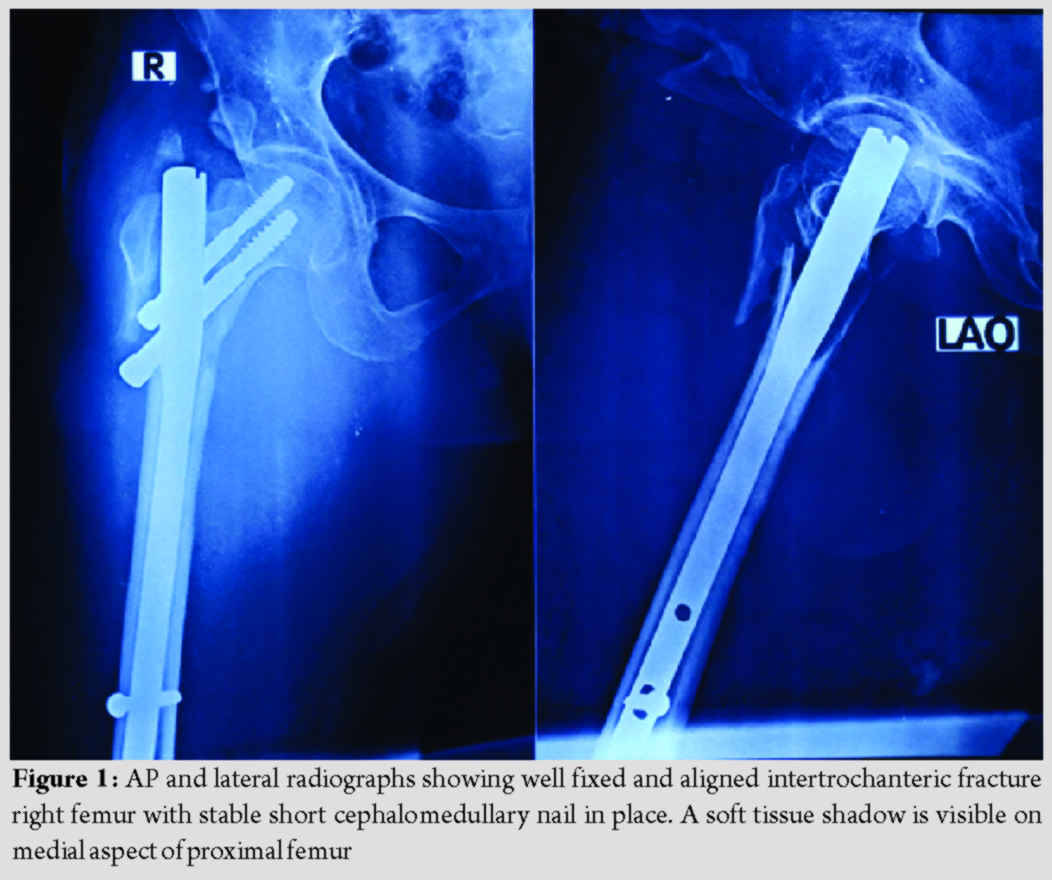
A 65-year-old lady had a domestic fall following which she was taken to a private hospital nearby where she was diagnosed as having intertrochanteric fracture of the right femur and was operated the next day with short cephalomedullary nailing. The operation was uneventful, and she was recovering well with subsequent rehabilitation post-surgery. She started noticing a slowly enlarging painful swelling in her medial aspect of the right thigh after a month of surgery. She was also complaining of weakness and vertigo and, therefore, was taken to the index surgeon. After reviewing fresh radiographs, which was reported unremarkable, the treating surgeon referred her to a general physician. Her hemoglobin was found to be on the lower side (6.9 g/dl) for which she had undergone two units of packed red cell transfusion and was advised iron supplement. She remained fine for a few weeks, but again, her condition started deteriorating and was kept on symptomatic management and received two more units of packed red cell transfusion. Finally, she was referred to our institution for further management 3 months after the index surgery. She was ambulatory with walker support. Past medical history included hypertension and rheumatoid arthritis. On examination, she looked pale and her vitals were stable. There was a tender, firm, ill-defined swelling over anteromedial aspect of the proximal part of right thigh; there was no erythema, overlying skin was intact, regional lymph nodes were not palpable, and hip range-of-motion of the affected side was painful. There was no pulsation or bruit felt over the swelling, and her distal pulses and capillary refilling were optimum. Routine laboratory, biochemical, and coagulation parameters were within normal range except for low hemoglobin levels (8.2 g/dl). Repeat radiographs of the extremity revealed satisfactory alignment and fixation of Intertrochanteric fracture with short cephalomedullary nail; there was a soft tissue shadow on medial aspect of the proximal femur with no evidence of calcification, cortical erosion, or periosteal reaction (Fig. 1).
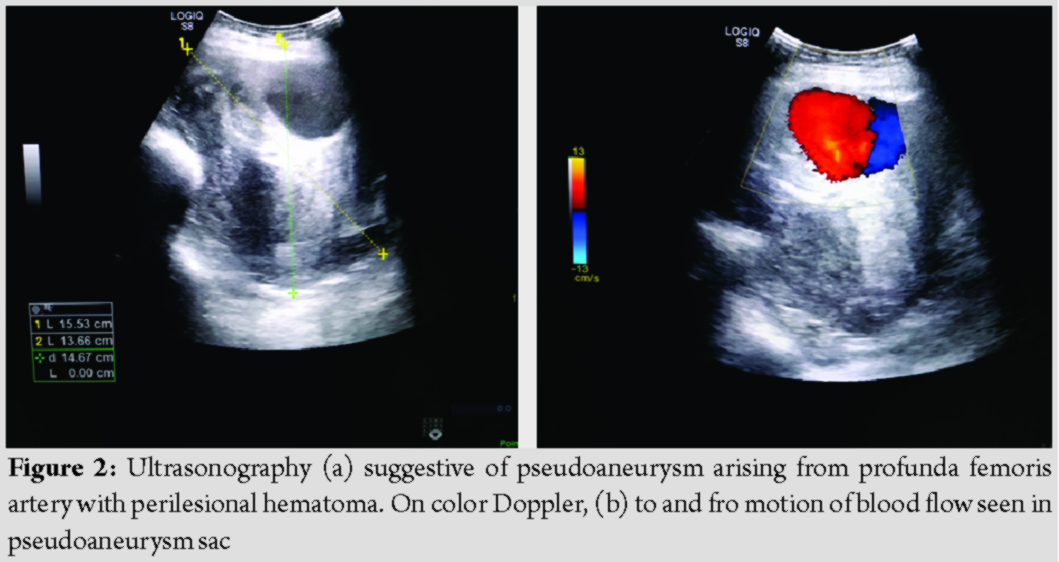
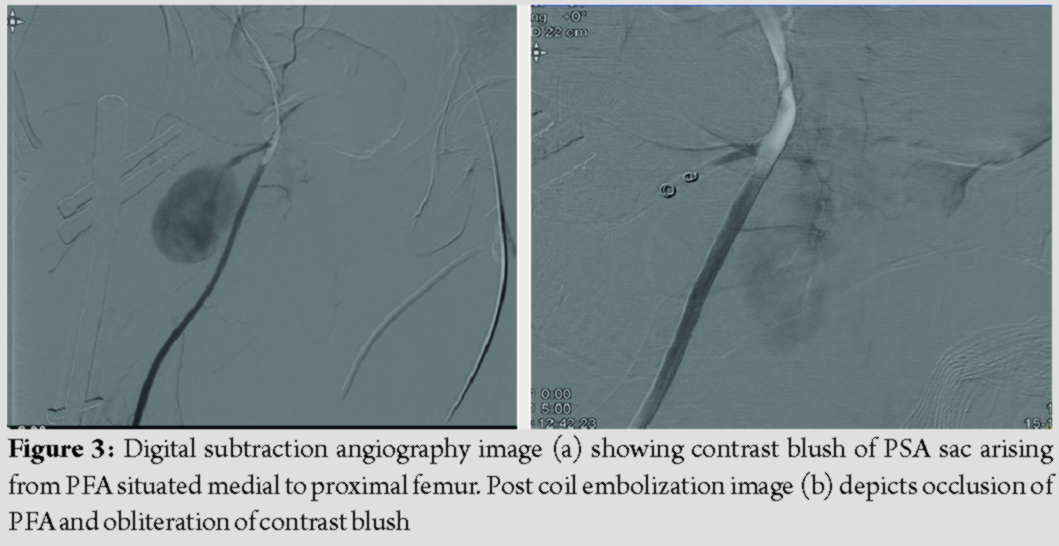
Duplex ultrasound demonstrated an anechoic saccular lesion with characteristic “yin-yang” sign suggestive of PSA arising from right PFA (Fig. 2). We, therefore, proceeded with right lower limb digital subtraction angiography (DSA) which confirmed PSA measuring 6.4 ×4.5 cm with a narrow neck. Selective embolization was performed at the same setting with 2 microcoils of size 18.2.0.2; post coiling image revealed complete occlusion of the PSA and good filling of the PFA proximal to the PSA (Fig. 3). The procedure was uneventful; she had a speedy recovery and discharged after 5 days. Follow-up duplex ultrasound demonstrated thrombosed PSA sac. At 9 months following embolization, she is free from symptoms with the resolution of swelling and healing of fracture as well.
Discussion
Pseudoaneurysm of PFA has been reported to happen following blunt or penetrating trauma and various orthopedic procedures around proximal femur such as external fixation, core-decompression, hip replacement, and fixation of pertrochanteric fractures with dynamic hip screw (DHS) or intramedullary nailing[3].With an overall frequency of 0.49%, this uncommon vascular insult can give rise to substantial morbidity and mortality[1]. With burgeoning number of elderly population being treated for intertrochanteric fractures, this frequency is expected to rise in the near future.
Pseudoaneurysm represents a pulsating encapsulated hematoma resulting from partial arterial vessel damage which possesses a permanent arterial blood circulation through its communication with the adjacent vessel. Profunda femoris artery is the most common culprit in thigh because of anatomical virtue of its close relationship with the proximal femur. Injury can be perpetrated by various non-iatrogenic or iatrogenic factors such as spike of displaced lesser trochanter or other bone fragments, forceful traction, deep posteromedial placement of retractors, clamps, overshot drill bit, and tap protruding from the medial femoral cortex, and large protruding screws [4, 5, 6]. Barquet et al. in their systematic review pointed out iatrogenic factors being the prevalent mechanism (96.15%), and its association with A2 trochanteric fractures predominate [1]. Moreover, traction during fracture fixation elongates and fixes the vessels, and with added adduction and internal rotation, PFA came to lie in the proximity of proximal femur, making it susceptible to injuring agent [6, 7]. For obvious reasons, elderly patients with atherosclerotic rigid and fragile arteries are more prone to develop PSA [1]. In our patient, the location of PSA appeared more proximal, away from the protruding distal locking screw tip which is in contrary to the usual location of PFA pseudoaneurysm opposite to the 3rd/4th screw hole of DHS side plate, which also corresponds to distal interlocking screw hole site of the short nail (Fig. 1 and 3) [4]. We surmise inadvertent placement of retractor proximally during fracture manipulation and reduction, or misplaced and overshot guidewire during placement of proximal lag screws could have caused partial vessel damage. Guidewire could easily go astray in osteoporotic bone in this elderly lady with rheumatoid arthritis. Intuitively, the onset of symptoms is more acute in the case of iatrogenic injury, whereas slow vascular erosion by impinging protruding screw leads to delayed presentation [7, 8]. Our case assumes significance since it presented late despite the most probable mechanism of being iatrogenic in nature. Clinical presentation varies widely based on the nature of the injury and can present acutely or on delayed fashion weeks, months, or years later [2, 7, 8]. Chong et al. described a triad of thigh swelling, bleeding from the incision site, and anemia with the falling trend of hemoglobin as the warning signals [9]. Pulsatility and systolic bruit are hard to ascertain due to the deep location of PSA. Distal limb perfusion is seldom compromised unless it is associated with occlusive disease of the superficial femoral artery [2, 9]. Clinical features are subtle and nonspecific which are most often attributed to usual post-operative thigh swelling, moderate anemia, and weakness and can mask the diagnosis [1]. Moreover, diagnostic dilemma arises since PSA can mimic local soft-tissue hematoma, inguinal lymphadenopathy, abscess, DVT, or even soft tissue sarcoma. Timely diagnosis is paramount to avoid sinister complications such as rupture with massive hemorrhage, infection, compartment syndrome, mass effect on the adjacent structure causing tissue destruction, neuropathy, venous obstruction, and thromboembolism [2, 3]. Diagnostic delay also prevailed in our case due to non-specific, innocuous clinical features; post-operative thigh swelling with unremitting anemia could have aroused suspicion earlier had there been proper scrutiny by the index surgeon. Therefore, the merit of this case lies in keeping surgeons abreast about this entity. Clinical suspicion can be aided by appropriate diagnostic modality. Plain radiographs usually are unremarkable, albeit can show cortical scalloping of the proximal femur in long-standing cases [7]. Duplex ultrasound is the initial modality of choice which can delineate size, extent of the sac, and presence of thrombus. CT angiography, a superior non-invasive modality, allows better visualization and can aid in decision making. Digital subtraction angiography (DSA) is considered the gold standard for both diagnosis and therapeutic intervention. It can accurately delineate site, size, the feeding vessel of PSA, and the patency of distal flow [2, 5, 10]. Still, there is no consensus as to the gold standard treatment for PSA of PFA. Small (<1 inch) and asymptomatic lesions can be treated conservatively with the premise of spontaneous obliteration. For larger, symptomatic lesion a slew of treatment modalities are described ranging from surgical exploration (aneurysmectomy, repair, and ligation) to various sophisticated radiological interventions such as ultrasound-guided compression, percutaneous thrombin injection, endovascular treatment with embolization, or stent-graft placement [1, 2, 11]. Presently, endovascular interventions are emerging as the therapeutic modality of choice with surgery reserved for cases not amenable for endovascular treatment. Our patient was successfully treated with selective embolization (Fig. 3); it is increasingly being regarded as a safe, effective, and standard of care with the added advantage of avoidance of another surgical intervention in elderly, frail patients [3, 8, 11]. Orthopedic surgeons should be mindful about this uncommon yet ominous complication; diligent care ought to be taken for prevention. Excessive traction with adduction and internal rotation to be avoided during fracture fixation, limb should be brought to the neutral rotation with less traction during placement of distal locking screw of short intramedullary nails. Careful fracture manipulation, monitoring the displacement of lesser trochanter fragment, use of guarded drill bit and careful drilling, keeping retractor and clamp close to the bone to avoid deep posteromedial placement, and choosing appropriate size screw are some of the key factors to adhere to during surgery [1, 4, 6, 7]. Extra care should be exercised during drill bit or guidewire introduction in osteoporotic bone. An astute surgeon should always keep a high index of suspicion and render appropriate diagnostic modality in case of any inexplicable post-operative thigh swelling to institute timely intervention.
Conclusion
Diagnosis of PSA of PFA demands strong vigil in view of its sparse occurrence following fixation of intertrochanteric fractures and varied clinical presentations; delayed presentation is, therefore, not uncommon. The importance of timely intervention cannot be overstated to avert sinister sequelae. Surgeons should also institute various preventive strategies during the fixation of intertrochanteric fractures to avoid this complication.
Clinical Message
Pseudoaneurysm of profunda femoris artery is an uncommon mishap perpetrated during the fixation of intertrochanteric fractures. Delayed diagnosis and treatment might lead to limb- or life-threatening complications. Minimally invasive treatment modality with selective embolization has been established as an effective remedy.
References
1. Barquet A, Gelink A, Giannoudis PV. Proximal femoral fractures and vascular injuries in adults: Incidence, aetiology and outcomes. Injury 2015;46:2297-313.
2. Hamoui M, Larbi A, Bommart S, Fauré P, Largey A, Canovas F. False aneurysm of perforating branch of the profunda femoris artery following intertrochanteric fracture, a rare vascular complication: Clinical, radiological features and management: Case report and review of the literature. Eur J Orthop Surg Traumatol 2010;20:59-65.
3. Rana N, Dhaked G, Sharma S, Tripathi S. Unusual presentation of pseudoaneurysm with trochanteric fracture femur with associated long-term antiepileptic therapy. Case Rep Orthop 2014;2014:896968.
4. Laohapoonrungsee A, Sirirungruangsarn Y, Arpornchayanon O. Pseudoaneurysm of profunda femoris artery following internal fixation of intertrochanteric fracture: Two cases report. J Med Assoc Thai 2005;88:1703-6.
5. Ritchie ED, Haverkamp D, Schiphorst TJ, Bosscha K. False aneurysm of the profunda femoris artery, a rare complication of a proximal femoral fracture. Acta Orthop Belg 2007;73:530-2.
6. Rajaesparan K, Amin A, Arora S, Walton NP. Pseudoaneurysm of a branch of the profunda femoris artery following distal locking of an intramedullary hip nail: An unusual anatomical location. Hip Int 2008;18:231-5.
7. Vande VK, Dauwe J, Van Oost J. Late presentation of an iatrogenic pseudoaneurysm of the profunda femoris artery following intramedullary nailing. Case Rep Orthop 2018;2018:8270256.
8. Chan WS, Kong SW, Sun KW, Tsang PK, Chow HL. Pseudoaneurysm and intramuscular haematoma after dynamic hip screw fixation for intertrochanteric femoral fracture: A case report. J Orthop Surg (Hong Kong) 2010;18:244-7.
9. Chong KC, Yap EC, Lam KS, Low BY. Profunda femoris artery pseudoaneurysm presenting with triad of thigh swelling, bleeding and anaemia. Ann Acad Med Singapore 2004;33:267-9.
10. Albert S, Daniel S, Gouse M, Cherian VM. Case of pseudoaneurysm mimicking a soft tissue sarcoma: A diagnostic pitfall. Malays J Med Sci 2015;22:61-4.
11. Pandey NN, Raju SN, Rajagopal R, Kumar S. Iatrogenic profunda femoris artery pseudoaneurysm: Late presentation with successful endovascular microcoil embolisation. BMJ Case Rep 2018;11:e228314.
 |
 |
 |
| Dr. Prabhat Agrawal | Dr. Saubhik Das | Dr. Naveen Kumar |
| How to Cite This Article: Agrawal P, Das S, Kumar N. Misery of Orthopaedic Surgeon: Delayed Diagnosis of Pseudoaneurysm of Profunda Femoris Artery Following Fixation of Intertrochanteric Femoral Fracture: A Case Report and Review of Literature. Journal of Orthopaedic Case Reports 2020 May-June;10(3):53-56. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com