[box type=”bio”] Learning Point of the Article: [/box]
Septic hip sequelae with contained femoral head but with femoral shortening and abductor lurch can effectively be treated by distal trochanteric advancement and femoral lengthening by simple technique of monorail external fixator.
Case Report | Volume 10 | Issue 5 | JOCR August 2020 | Page 43-47 | Nagaraj Manju Moger, J Pragadeeshwaran, Vivek Singh1, R Akshay, Rama Priya Yasam, Varun Garg. DOI: 10.13107/jocr.2020.v10.i05.1832
Authors: Nagaraj Manju Moger[1], J Pragadeeshwaran[1], Vivek Singh[1], R Akshay[1], Rama Priya Yasam[1], Varun Garg[1]
[1]Department of Orthopaedics, All India Medical Sciences, Rishikesh, Uttarakhand, India.
Address of Correspondence:
Dr. Vivek Singh,
Department of Orthopaedics, All India Medical Sciences, Rishikesh, Uttarakhand, India.
E-mail: singhvr27@gmail.com
Abstract
Introduction: Acute septic arthritis of the hip in children requires prompt diagnosis and treatment. The resulting sequelae of septic arthritis are diverse. Varieties of procedures have been described in the orthopedic literature. The common goal of treatment of all these procedures is to achieve a mobile, stable, pain-free hip joint with minimal limp and limb length inequality.
Case Report: We present two cases of Choi’s Type 2 septic hip sequelae, a 14-year-old female and a 13-year-old male, both had painless limp and limb length discrepancy managed by greater trochanteric advancement with limb lengthening by monorail external fixator at single sitting.
Conclusion: Distal greater trochanteric advancement with limb lengthening by monorail external fixator is a useful technique to treat septic hip sequelae with stable hip joint.
Keywords: Septic sequelae hip, Ilizarov hip reconstruction, monorail external fixator, greater trochanteric advancement.
Introduction
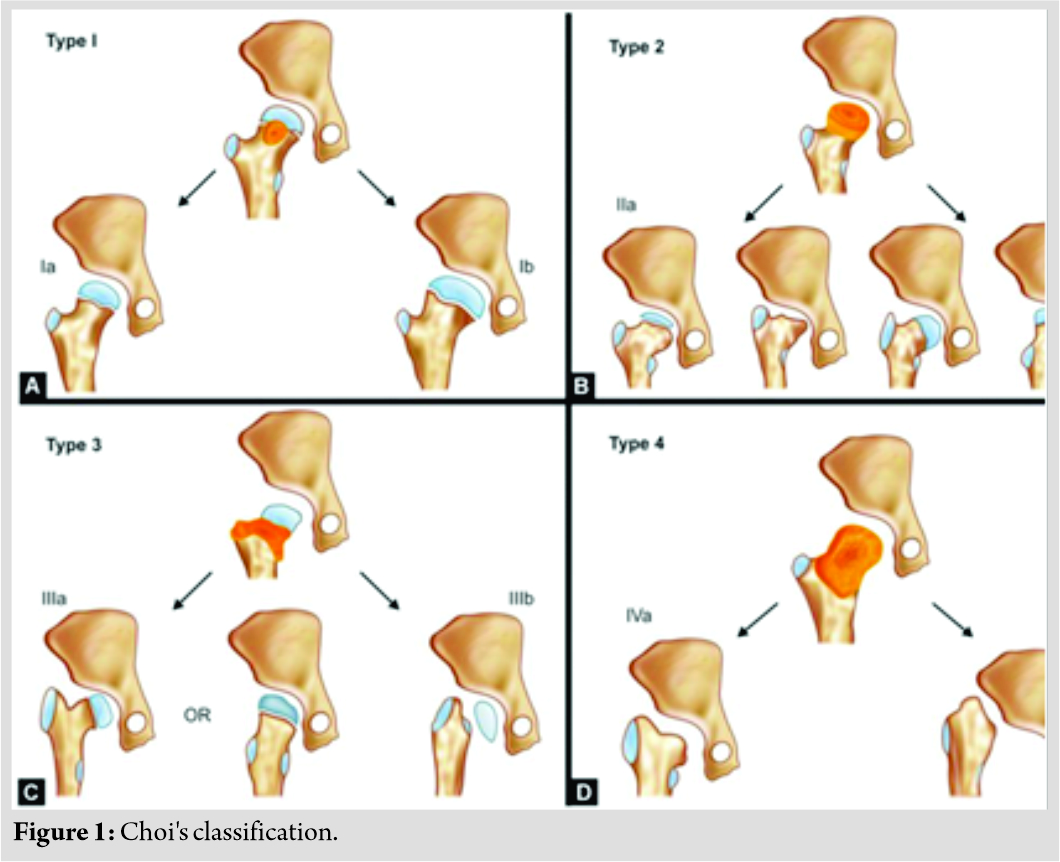
Acute septic arthritis of the hip in children requires prompt diagnosis and treatment. However, this may not be possible, because of missed diagnosis at an early stage of the disease. This is especially true in the setting of developing countries like India where access to specialist pediatric orthopedic care is extremely limited. The resulting sequelae of septic arthritis are diverse and may include minimal residual deformity, coxa breva with deformed head, or coxa vara or valga due to asymmetrical physeal closure, or complete destruction of femoral head and neck with no articulation at hip joint [1, 2, 3]. Choi’s radiographic classification is the most commonly used classification for this condition (Table 1 and Fig. 1) [4].
Varieties of procedures have been described in the orthopedic literature for various stages of disease and range from simple observation to complex procedures such as limb lengthening and Ilizarov hip reconstruction (IHR) [2]. The common goal of treatment of all these procedures is to achieve a mobile, stable, pain-free hip joint with minimal limp and limb length inequality. The problem in Choi’s Type 2 hip is femoral shortening due to premature physeal closure and abductor dysfunction due to coxa vara. We report here two cases of this type treated with a simple operation of distal trochanteric advancement and equalization of limb length by monorail external fixator.
Case Report
Case 1
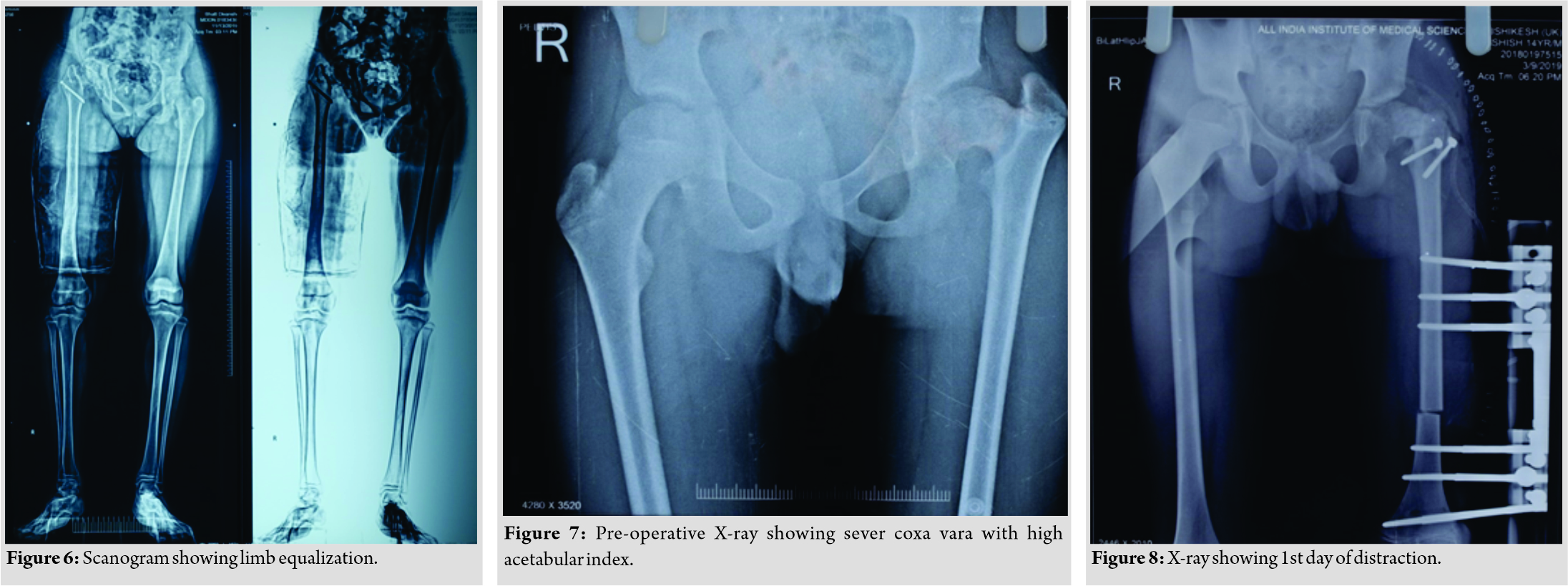
A 13-year-old female patient presented with complaints of painless limp in the right lower limb. The patient had a significant history of septic arthritis of the right hip joint which was managed conservatively in the past. On examination, it was found that the patient had a stable (negative telescopic test) and mobile hip with moderate restriction of abduction (20°). There was no fixed deformity. There was 7 cm of true femoral shortening. The child walked with a Trendelenburg gait with an added component of shortening which was partially compensated by ankle equinus. Radiological investigations revealed severe coxa vara with the steep acetabular inclination and was classified as Choi’s Type 2 septic hip sequel. Based on this workup, it was found that the child was having abductor lurch and femoral shortening, and both needed to be addressed. The patient was put on a lateral position in the operation theater and proximal femur was opened by a posterolateral approach. The hip abductors were carefully identified at their insertion on the greater trochanter (GT) and also the vastus lateralis distally. Piriformis tendon was also carefully identified. A 2 cm thickness of GT with attached abductors proximally and vastus lateralis distally was elevated with an oscillating saw (Fig. 2). 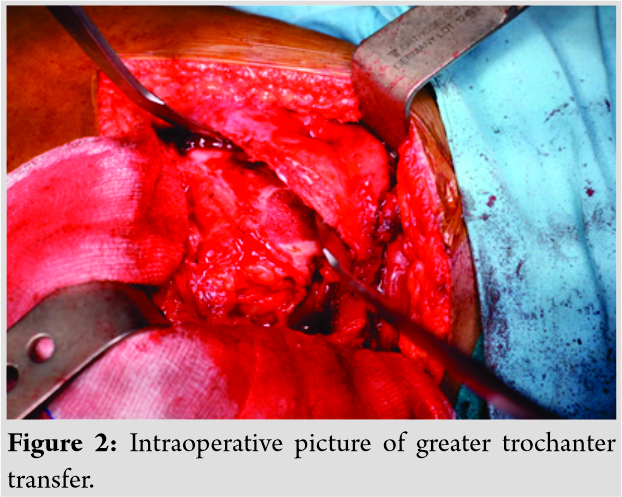
The actual follow-up 10 months following index surgery. The lengthening procedure was carried out for almost 4 months, with 6 months of further follow-up following fixator removal. Any complications such as pin-tract infection or fracture of the regenerate usually happen during the first 6 months of following fixator removal. This case has no such complication during this period another possibility of further growth of femur is also negated us the patient is approaching 14 years of age. Hence, 6 months of follow-up are adequate to see the outcome.
Post-operative rehabilitation protocol:
· Immediately following surgery knee range of motion exercises was started and was carried out during lengthening procedure and further follow-up
· Hip abduction exercises are started 8 weeks following index procedure when the trochanteric fragment started showing signs of union
· Protected weight-bearing with a PVC thigh brace was started 6 weeks following fixator removal and unsupported full weight-bearing mobilization started 6 weeks following fixator removal.
Case 2
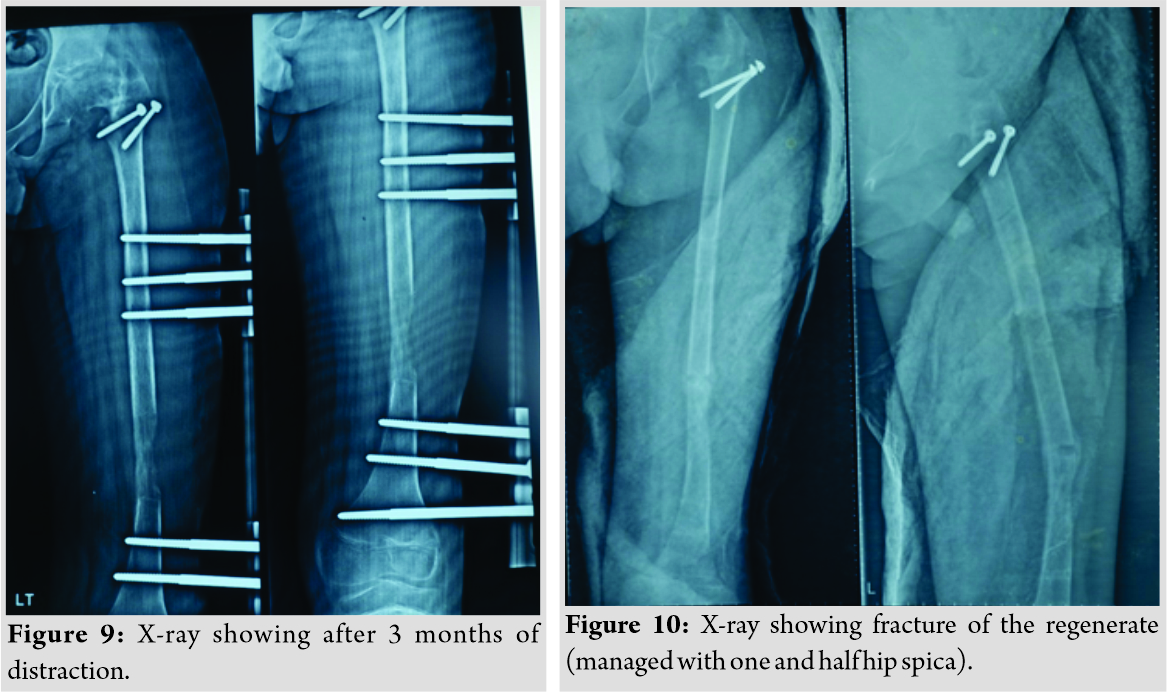
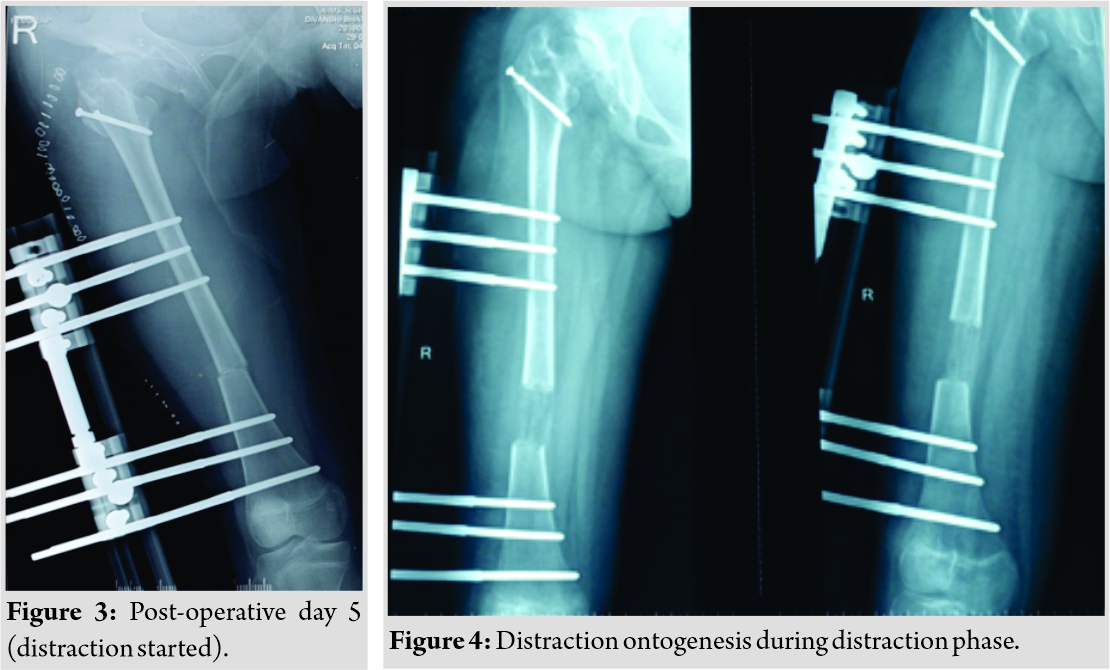
The second patient, a 14-year-old male, presented to us with complaints of limping in the left lower limb without any pain in the hip joint. He also had a history of septic arthritis in the left hip which was managed non-operatively in a village hospital. There was no history of trauma, weight loss, or tuberculosis. On examination, it was found that the patient had limited terminal hip ROM with severe restriction in hip abduction (25°). There was a true shortening of 6 cm in the left femur and the patient walked with abductor lurch without any ankle equinus with excessive flexion in the opposite knee. An X-ray revealed severe coxa vara on the left side with increased acetabular index (Fig. 7). There was minimal joint space narrowing medially. The femoral diaphysis was thin as compared to the opposite side. The power of the muscles around the hip and knee was comparable to the opposite side. Based on these findings, it was classified as a case of Choi’s Type 2 septic sequelae of the hip with 6 cm of femoral shortening. The patient underwent trochanteric advancement distally as described in the previous case along with a simultaneous application of monorail external fixator and corticotomy in the distal femur. The distraction started on the 5th post-operative day in equal increments of 0.25 mm every 6 hourly (Fig. 8 and 9). After achievement of limb length equalization, the fixator was removed after 114 days. Three weeks after this, the patient presented with a fracture of the regenerate with minimal angulation and was managed further by one and a half spica cast for further 4 weeks (Fig. 10). At latest 12 months follow-up, the patient was walking normally with minimal abductor lurch.
Discussion
The treatment of sequelae of the septic hip depends on the stability of the hip joint, the desire of the patient for a mobile hip and limb length. Surgical options vary from pelvic support osteotomy to modified Albee hip arthroplasty to IHR to arthrodesis and hip arthroplasty [1]. Unstable hip with positive telescopy sign is usually treated by pelvic support osteotomy where an osteotomy is done in the proximal femur at the level of ischial tuberosity so that the lesser trochanter sits into the residual acetabulum creating a stable hip [5]. The problem with this procedure is, it places the extremity in valgus alignment with a deviation of the mechanical axis of the limb. To address this problem, Ilizarov developed a procedure where two-level osteotomy is done, one at the proximal femur and one distal so that mechanical axis of the limb is aligned simultaneously with the equalization of limb length. Various authors have reported good to excellent results with this technique and are summarized in Table 2. IHR is a technically demanding procedure with requirement of two-level corticotomy, one proximally for lengthening and second distally for aligning the limb parallel to the opposite side. Furthermore, in our experience, the acceptability of Ilizarov to the patient is poorer than the monorail fixator. Another factor is cost, which is more in Ilizarov ring fixator. In view of all this issues, we opted for monorail fixator. There are various procedures described in the literature for the management of patients with a stable hip. Most of these studies have concentrated on femoral lengthening only with various techniques such as Ilizarov or lengthening over an intramedullary nail [3, 5]. In our experience, in the management of infantile septic hip sequelae, Choi Type 2 with femoral shortening is a relatively uncommon condition. To address this problem, one must concentrate not only on achieving limb equalization but also reduction of abductor lurch. The later can very well be taken care of by distalization of GT with care taken not to injure the abductors. In both of our cases, it was addressed and at the end of 12 months follow-up, the children were having a mobile hip, equalized limb length, and minimal abductor lurch. We had a complication of fracture of the regenerate and are a well-known complication as reported in the literature [6, 7]. To address this complication, we recommend that the fixator must be kept on the limb for the same time it was kept for distraction. One should not worry too much if a fracture of the regenerate occurs as this can be managed easily by POP cast application for further 4–6 weeks.
Conclusion
Distal greater trochanteric advancement with limb lengthening by monorail external fixator is a useful technique to treat septic hip sequelae with stable hip joint.
Clinical Message
Infantile septic sequelae with femoral shortening and stable hip joint need limb lengthening as well as correction of abduction lurch, both these issues can be addressed effectively by limb lengthening over monorail external fixator and simultaneous distal trochanteric advancement. Both of which are technically easier procedure than available literature.
References
1. El-Tayeby HM. Osteochondroplasty of the femoral head in hip reconstruction for Type II late sequelae of septic arthritis: A preliminary report. J Child Orthop 2008;2:431-41.
2. El-Rosasy MA, Ayoub MA. Midterm results of Ilizarov hip reconstruction for late sequelae of childhood septic arthritis. Strategies Trauma Limb Reconstr 2014;9:149-55.
3. Baghdadi T, Saberi S, Eraghi AS, Arabzadeh A, Mardookhpour S. Late sequelae of hip septic arthritis in children. Acta Med Iran 2012;50:463-7.
4. Choi IH, Pizzutillo PD, Bowen JR, Dragann R, Malhis T. Sequelae and reconstruction after septic arthritis of the hip in infants. J Bone Joint Surg Am 1990;72:1150-65.
5. Laubscher M, Mitchell C, Timms A, Goodier D, Calder P. Intramedullary femoral lengthening with an unstable hip without prior stabilisation: Preliminary results of a case series. S Afr Orthop J 2017;16:44-8.
6. Burke NG, Cassar-Gheiti AJ, Tan J, McHugh G, O’Neil BJ, Noonan M, et al. Regenerate bone fracture rate following femoral lengthening in paediatric patients. J Child Orthop 2017;11:210-5.
7. Launay F, Younsi R, Pithioux M, Chabrand P, Bollini G, Jouve JL. Fracture following lower limb lengthening in children: A series of 58 patients. Orthop Traumatol Surg Res 2013;99:72-9.
8. Umer M, Rashid H, Umer HM, Raza H. Hip reconstruction osteotomy by Ilizarov method as a salvage option for abnormal hip joints. Biomed Res Int 2014;2014:835681.
9. Rozbruch SR, Paley D, Bhave A, Herzenberg JE. Ilizarov hip reconstruction for the late sequelae of infantile hip infection. J Bone Joint Surg Am 2005;87:1007-18.
10. Mudiganty S, Sipani AK, Das SK. A case of late sequela of infantile hip infection treated by Ilizarov hip reconstruction using monolateral fixator. JMS J Med Soc 2015;29:109-12.
11. Ghanghurde B, Agashe M, Rustagi T, Rathod C, Mehta R, D’Silva D, et al. Treatment of unstable hips in children with Ilizarov hip reconstruction: A retrospective analysis of six cases. Paediatr Orthop Relat Sci 2017;3:23.
 |
 |
 |
 |
 |
| Dr. Nagaraj Manju Moger | Dr. J Pragadeeshwaran | Dr. Vivek Singh | Dr. R Akshay | Dr. Rama Priya Yasam |
| How to Cite This Article: Moger NM, Pragadeeshwaran J, Singh V, Akshay R, Yasam RP, Garg V. Trochanteric Advancement and Limb Lengthening by Monorail External Fixator in Sequelae of the Septic Hip in Children – A Simpler Alternative to Other Complex Procedures. Journal of Orthopaedic Case Reports 2020 August;10(5): 43-47. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com