[box type=”bio”] Learning Point of the Article: [/box]
Local Delivery of single dose Intraepiphseal Zolidronic acid is a promising new treatment modality for preventing progression of Legg-Calvé-Perthes disease , paving way for larger case series. Essential to exercise alert judgement in indicated children.
Case Report | Volume 10 | Issue 5 | JOCR August 2020 | Page 65-68 | R Sivakumar, V Somashekar, Prahalad Kumar Singhi, M Chidambaram. DOI: 10.13107/jocr.2020.v10.i05.1842
Authors: R Sivakumar[1], V Somashekar[1], Prahalad Kumar Singhi[1], M Chidambaram[1]
[1]Department of Orthopaedics, Preethi Hospitals (P) Ltd., Madurai, Tamil Nadu, India.
Address of Correspondence:
Dr. Somashekar Venkatappa,
Consultant in Orthopaedics, Preethi Hospitals (P) Ltd., No 50, Melur Main Road, Madurai – 625 107, Tamil Nadu, India.
E-mail: somuortho@gmail.com
Abstract
Introduction: Legg-Calve´-Perthes disease (LCPD) or avascular necrosis of the capital epiphysis is an idiopathic disease characterized by interruption of the blood supply to the capital femoral epiphysis resulting in necrosis of the epiphysis. There are a variety of treatment modalities such as containment with braces early in disease to surgical procedures for children presenting late in their age group. The newer modalities of treatment are intravenous bisphosphonates, bone morphogenic protein in clinical subjects.
Case Report: Two children (Aged 7 years with catterall Stage II unilateral affection, aged 11 years catterall Stage III bilateral affection) were advised single-dose of zoledronic acid(2 mg) into epiphysis as day care procedure after due discussion with parents about other treatment modalities. Both the children were followed up quarterly with clinical examination and radiology. At the latest follow-up of 4 years both had satisfactory outcome. Child one was able to do normal play with intact lateral pillar. Child two had minimal collapse of left hip however clinically pain free.
Conclusion: Local delivery of single dose of intra epiphyseal zoledronic acid is a relatively harmless procedure and effective in preventing the progression of disease pathology, especially in children with age group of 6–10 years.
Keywords: Legg-Calve´-Perthes disease, avascular necrosis capital epiphysis, intra epiphyseal zoledronic acid, catterall stage.
Introduction
Legg-Calve´-Perthes disease (LCPD) or avascular necrosis of the capital epiphysis is an idiopathic disease characterized by interruption of the blood supply to the capital femoral epiphysis resulting in necrosis of the capital epiphysis [1]. The vascular disruption of the femoral capital epiphysis occurs by undefined mechanism, with resulting epiphyseal osteonecrosis, followed by resorption of necrotic tissue, repair and remodeling, and replacing necrotic bone by healthy new bone [2]. Early in the pathology extrusion of femoral head and resultant deformation due to weight bearing is the prima facie cause for all the morbidity of the disease. There are a variety of treatment modalities like containment with braces early in disease to surgical procedures of varus derotation osteotomy for children presenting later in the age group. In the middle are the newer modalities of intravenous Bisphosphontes, Bone Morphogenic Protein in clinical subjects and Intraepiphyseal Bisphosphonates in animal studies. We present two cases of children with Stage II and Stage III Perthes treated with intra-articular zoledronic acid with 4 years of follow-up with satisfactory outcome.
Case 1
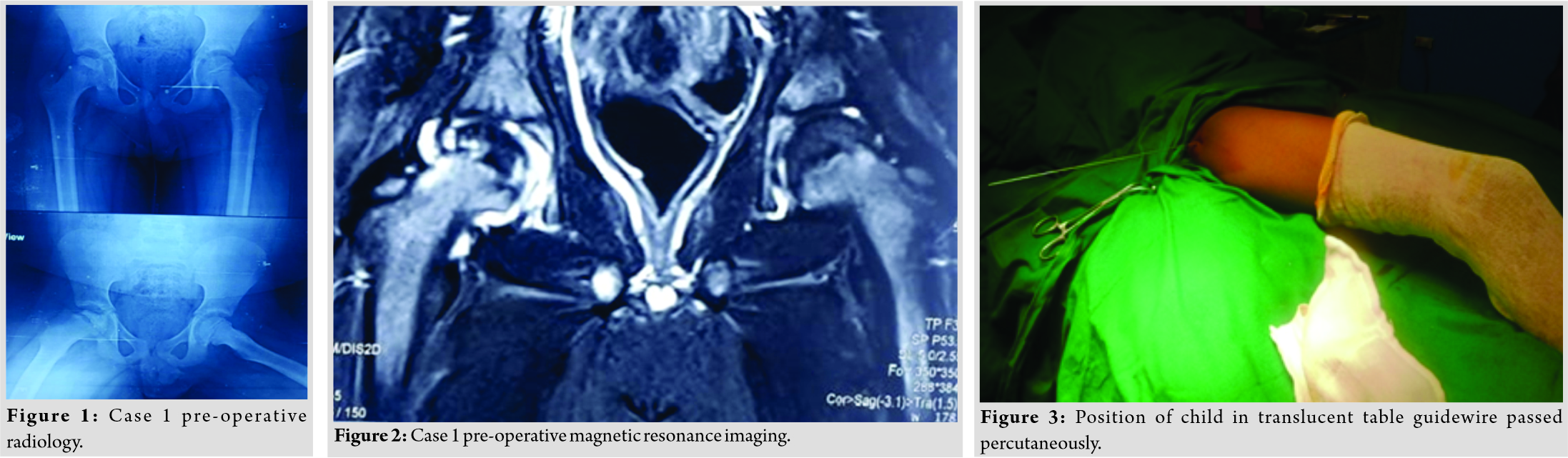
A 7 years old boy presented with pain and limp while walking in the right hip joint over a period of 18 months. Pain relived intermittently with analgesics and activity restriction. On clinical and radiological examination showed Grades II–III Catterall Perthes disease [3] (Fig. 1). Magnetic resonance imaging (MRI) confirmed the same (Fig. 2). He was advised intra-articular zoledronic acid after failed attempt of containment measures and with due discussion with child’s parents. Hospital ethical committee approval was taken before the commencement of the study.
Technique
Child was taken up for day care surgical procedure after routine requisite preparation. Child was placed on translucent table with soft roll placed under ipsilateral gluteal region. Under appropriate anesthesia hip joint painted, draped, and pre-operative single dose of antibiotic given. Initially under fluoroscopy guidance 1.5 mm guide wire is passed percutaneously into capital epiphysis by adducting the thigh (Fig. 3). Position of wire is confirmed in both anteroposterior and frog leg lateral view (Fig. 4). Inadvertent rotation is avoided to prevent bending or breakage of guide wire. Then, outer cannula of vertebroplasty J needle is threaded over guide wire positioning the cannula, guide wire is removed (Fig. 5). A 1 ml of Hypaque is injected to confirm that cannula is not in the joint. Then, 2 mg of reconstituted zoledronic acid is injected into capital epiphysis over a period of 10 min (Fig. 6, 7). Then, the cannula removed and adhesive dressing applied. Child is discharged on same day with analgesics and supportive treatment. Child is examined serially at 3 months interval for pain, limitation of day to day activities, and radiological examination.
Case 2
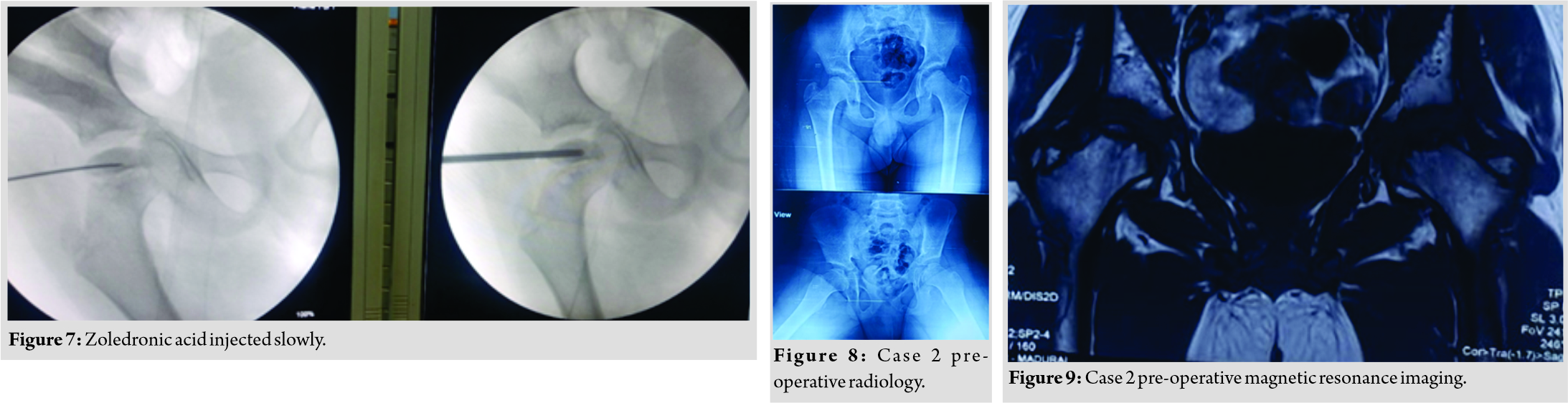
A 11 years old boy presented with pain in both the hip joints for more than 2 years. Pain was treated intermittently with analgesics and activity restriction at local hospital. On clinical and radiological examination, it was confirmed with Grade III Catterall Perthes (Fig. 8). MRI revealed fragmentation, subchondral collapse, and mild synovial effusion (Fig. 9). Hip range of motion was near normal and parents not willing for surgical intervention he was advised bilateral intra-articular zoledronic acid (2 mg in each hip) after due consent regarding the prognosis and outcome of the procedure.
Results
Case 1 was seen regularly with latest follow up of 4 years, had significantly reduced pain and was able to play well at school. On clinical examination, he was able to squat and sit cross legged. Radiology revealed minimal collapse of lateral pillar Stage II Collapse (Fig. 10, 11).
Case 2 was followed regularly for the past 5 years. He is pain free, has uninterrupted play at school except contact sports. On clinical examination had terminal restriction of the left hip compared to right. Radiology revealed Stage III collapse with cyst in the left hip and Stage II in the right hip. Although radiology revealed severe form of perthes, adolescent is symptom free (Fig. 12, 13).
Discussion
LCPD is a relatively common condition affecting around 4–5 in 100,000 children aged 4–10 years [4]. Even though the etiology is idiopathic, the many authors have suggested possible pathology being vascular disturbance leading onto intravascular thrombosis of the vessels to the femoral head and resultant coagulopathy [5]. Protocols are being advocated to treat the children with changing scenario. Age is one of the prognosticating factors where earlier the presentation, much better is the outcome. Rosenthal et al. in their retrospective study found onset of LCPD before the age of 6 years is favorable, with 80% having a good result with nonsurgical and supportive measures [6]. Similarly, in children with late onset of disease there is always trend toward surgical containment procedures either with varus derotational femoral osteotomy or salter osteotomy. Arkader et al. [7] found a trend towards better radiographic outcomes when varus derotational osteotomy was performed early in the disease with no statistical difference between surgical and conservative treatment. Pathophysiological studies in piglets have revealed ischemic necrosis of immature femoral head leads to mechanically weak femoral head leading onto collapse [8]. The necrotic bone with increased osteoclastic resorption, delayed laying of new bone and loading on this weak bone leads to collapse and deformation of the femoral head. Many medical interventional strategies have been studied to inhibit the osteoclastic activity with use of bisphosphonates, bone morphogenic proteins both in isolation and combination therapy. In a study, osteonecrosis was surgically induced in femoral head of rats, followed by zoledronic acid treatment and prophylaxis improved sphericity and architecture at 6 weeks [9]. Very few studies have been published in the literature regarding the use of bisphosphonates. Agarwala et al. showed oral bisphosphonate therapy improved in clinical function, a reduction in the rate of collapse and decrease in the requirement for total hip replacement, compared with the findings of other studies in which no treatment was given [10]. Local delivery of single injection of bisphosphonates was found to be effective in decreasing the deformity in immature pig as studied by Aya-Ay et al. [11]. In an another study done by Vandermeer et al. found that a combination of ibandronate and recombinant bone morphogenic protein-2 decreased femoral head deformity while stimulating bone formation in an immature animal model of ischemic osteonecrosis [12]. The above paper prompted us perform this procedure where a single dose of 2 mg of reconstituted zoledronic acid was injected into femoral epiphysis. Furthermore, low dose of zoledronic acid which is administered locally, acts where it is required and avoids systemic effects. The results of case 1 with unilateral perthes showed excellent clinical and radiological outcome. In case 2 with bilateral involvement, clinically the child is doing fine with pain relief and school activities. Radiologically, there appears to be collapse of the left hip with reasonably maintained right hip femoral head. Both the children need long-term follow-up to see their progression to total hip replacement. Further research should involve identifying early markers that can predict those children who would benefit from surgery and those with minimal intervention [13]. Till then, younger age group <6 years can be treated non-operatively, and those >6 years benefit from surgery or minimal intervention depending on head collapse [13]. This is a case study involving a very small number of children. However, with large number of study subjects dividing into age groups, stages, and long-term follow-up is very much required to propose a treatment protocol, which is also the limitation of this study.
Conclusion
Local delivery of single dose of intraepiphyseal zoledronic acid is a relatively harmless procedure and effective in preventing the progression of disease pathology. This treatment is beneficial in children with age group of 6–10 years avoiding early surgical intervention. Furthermore, these children need monitoring to see any progressive restrictions and deformities which can be addressed anytime later.
Clinical Message
Local delivery of single dose intraepiphyseal zoledronic acid is a promising new treatment modality for preventing progression of LCPD, paving way for larger case series. Essential to exercise alert judgment in indicated children.
References
1. Joseph B. Management of Perthes’ disease. Indian J Orthop 2015;49:10-6.
2. Jensen OM, Lauritzen J. Legg-Calvé-Perthes’ disease. Morphological studies in two cases examined at necropsy. J Bone Joint Surg Br 1976;58:332-8.
3. Catterall A. The natural history of Perthes’ disease. J Bone Joint Surg Br 1971;53:37-53.
4. Molloy MK, MacMahon B. Incidence of legge-perthes disease (osteochondritis deformans). N Engl J Med 1966;275:988-90.
5. Glueck CJ, Crawford A, Roy D, Freiberg R, Glueck H, Stroop D. Association of antithrombotic factor deficiencies and hypofibrinolysis with Legg-Perthes disease. J Bone Joint Surg Am 1996;78:3-13.
6. Rosenfeld SB, Herring JA, Chao JC. Legg-Calve-Perthes disease: A review of cases with onset before six years of age. J Bone Joint Surg Am 2007;89:2712-22.
7. Arkader A, Shankar WN, Amorim RM. Conservative versus surgical treatment of late-onset Legg-Calve-Perthes disease: A radiographic comparison at skeletal maturity. J Child Orthop 2009;3:21-5.
8. Kim HK, Su PH, Qiu YS. Histopathologic changes in growth-plate cartilage following ischemic necrosis of the capital femoral epiphysis. An experimental investigation in immature pigs. J Bone Joint Surg Am 2001;83:688-97.
9. Little DG, Peat RA, Mcevoy A, Williams PR, Smith EJ, Baldock PA. Zoledronic acid treatment results in retention of femoral head structure after traumatic osteonecrosis in young Wistar rats. J Bone Miner Res 2003;18:2016-22.
10. Agarwala S, Shah S, Joshi VR. The use of alendronate in the treatment of avascular necrosis of the femoral head: Follow-up to eight years. J Bone Joint Surg Br 2009;91:1013-8.
11. Aya-ay J, Athavale S, Morgan-Bagley S, Bian H, Bauss F, Kim HK. Retention, distribution, and effects of intraosseously administered ibandronate in the infarcted femoral head. J Bone Miner Res 2007;22:93-100.
12. Vandermeer JS, Kamiya N, Aya-Ay J, Garces A, Browne R, Kim HK. Local administration of ibandronate and bone morphogenetic protein-2 after ischemic osteonecrosis of the immature femoral head: A combined therapy that stimulates bone formation and decreases femoral head deformity. J Bone Joint Surg Am 2011;93:905-13.
13. Ramachandran M, Reed DW. Legg-Calve-Perthes: Disease of the hip. Orthop Trauma 2016;30:461-70.
 |
 |
 |
 |
| Dr. R Sivakumar | Dr. V Somashekar | Dr. Prahalad Kumar Singhi | Dr. M Chidambaram |
| How to Cite This Article: : Sivakumar R, Somashekar V, Singhi PK, Chidambaram M. Local Delivery of Single Dose Intra Epiphyseal Bisphosphonates to Prevent the Progression of Legg-Calve-Perthes Disease – Case Series. Journal of Orthopaedic Case Reports 2020 August;10(5): 65-68. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com