[box type=”bio”] Learning Point of the Article: [/box]
Postoperative dissembly of prosthesis can lead to catastrophe if not managed adequately.
Case Report | Volume 10 | Issue 5 | JOCR August 2020 | Page 75-77 | Ruchit Shah, Urvi Khambhati, Feral Daruwala. DOI: 10.13107/jocr.2020.v10.i05.1848
Authors: Ruchit Shah[1], Urvi Khambhati[2], Feral Daruwala[3]
[1]Department of Orthopedic, Era’s Medical College, Lucknow, Uttar Pradesh, India.
[2]Department of Radiology, Lilavati Hospital and Research Centre, Mumbai, Maharashtra, India.
[3]Department of Medical Writing. Nephrolife-The Complete Kidney Care, Surat, Gujarat, India.
Address of Correspondence:
Dr. Ruchit Shah,
Era’s Medical College, Department of Orthopedic, Lucknow, Uttar Pradesh. India.
E-mail: ruchit.acedemic@rediffmail.com
Abstract
Introduction: Hip fracture is an established health problem, especially in the elderly population and, its incidence is dramatically rising in the globe. The standard protocol of management in the elderly population for end-stage hip diseases and unstable femur fracture is bipolar hemiarthroplasty. Common complications of hip replacement include infection, fracture, dislocation, venous thrombosis, nerve palsy, chronic pain, and implant failure. In the literature, there are very few reported cases of disassembly of the implant in hemi replacement arthroplasty.
Case Report: We, hereby, present a case of the spontaneous disassembly of the bipolar hip prosthesis, which was timely recognized and treated adequately in an elderly patient.
Conclusion: The use of the cemented bipolar prosthesis can also lead to disassembly of the implant components and thereby the need for open reduction. Identification of the distinction between dislocation of head and disassembly of the prosthetic components is vital for favorable patient prognosis.
Keywords: Hemi replacement arthroplasty, implant failure, disassembly.
Introduction
Hip fracture is a major health concern in elderly people [1, 2]. The standard line of management is hip arthroplasty (replacement), depending on whether it is intracapsular or extracapsular [3]. Hemi replacement arthroplasty is the preferred surgery in the geriatric population, as less mobility and the large diameter of the femur head reduces the chances of dislocation [4, 5, 6]. To date, here mentioned four surgical techniques for hemi replacement arthroplasty are well established: Anterior (Smith-Petersen), anterolateral (Watson-Jones), lateral (Hardinge or Liverpool), and posterior (Moore). There are few reported cases of dislocation and disassembly of the implant between the head and the shell [7]. The availability of different sizes of head and neck in bipolar implant enables the treating surgeon to select appropriate prosthetic taking into consideration the age of the patient and desired range of motion required. By this way, the complications are significantly reduced for the bipolar implant than unipolar. However, there are severe but few complications associated with bipolar implant such as dislocation and disassembly of the prosthesis. [8]. Patients are usually treated by the closed reduction in case of hip dislocations, whereas disassembly of the prosthesis requires the need for open reduction. For timely management and a better outcome, recognition at the right time, as well as differentiation between dislocation and disassembly of the prosthesis, is of paramount importance.
Case Report
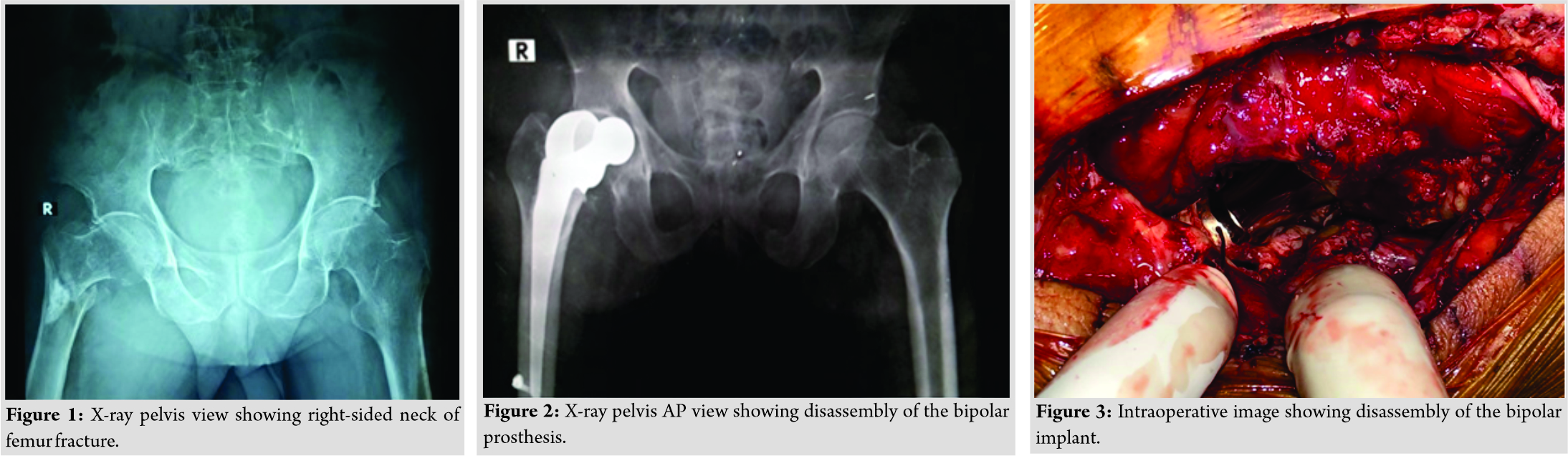
A 70-year-old male presented with chief complaints of hip pain, swelling, and restricted mobility following fall in his house 1 day back in the month of May 2018 before consulting to us. He underwent a clinical and radiological examination, in which he was diagnosed as a case of fractured neck of the femur of the right hip secondary to age-related osteoporosis, as shown in (Fig. 1).
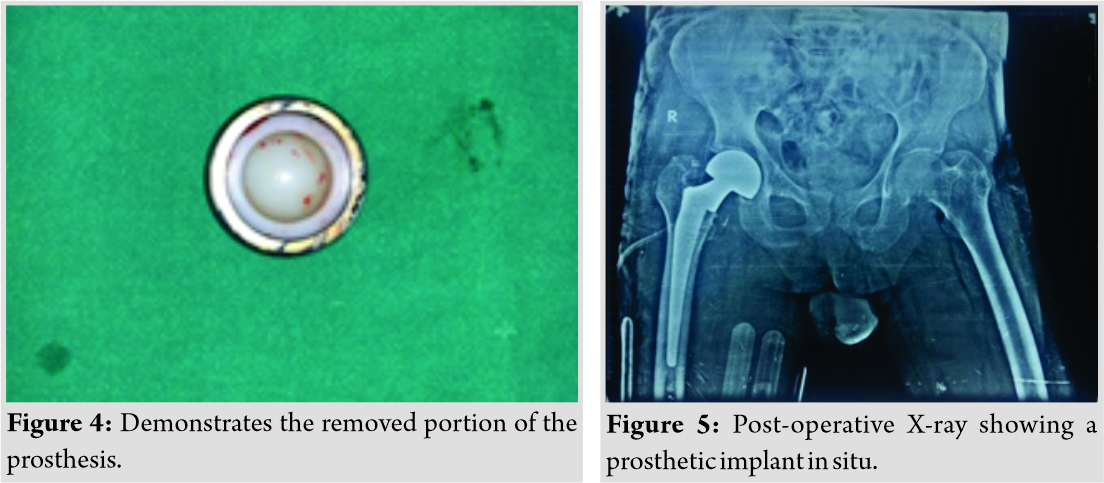
Considering the age of the patient, he was operated for hemi replacement arthroplasty by posterior approach, for which cemented bipolar prosthesis was used. Postoperatively on the 5th day, the patient felt clicking in her right hip while walking and was unable to move her hip as usual. The patient came back to the hospital for the following complaints and was admitted again, after which he underwent clinical and radiological investigations. On examination, there was swelling in the hip region with no open wound, scar, or dilated veins. On palpation, there was tenderness over the right Scarpa’s area with bitrochanteric compression test positive. There were no neurological signs or symptoms. The hip radiographs demonstrated dissociation of the components of the bipolar hemiarthroplasty at the femoral head and neck junction (Fig. 2). Open reduction was performed through the old surgical scar using the posterior approach. The femoral head component was found intraoperatively in the acetabulum and was covered with a well-healed capsule. The tapered part at the inner head and stem neck did not show any scratch marks or defects. (Fig. 3) shows intraoperative photos while removing dissociated bipolar hip prosthesis.
(Fig. 4) shows the extracted bipolar prosthesis. After the revised surgery, the patient has been followed up for 1 year, and he is asymptomatic with a favorable outcome. (Fig. 5) shows the post-operative X-ray of the pelvis with a new femoral head with longer offset assembled to the old femoral stem.
Discussion
Over decades, hip hemiarthroplasty has been used successfully to manage end-stage hip disorders and fracture of femur neck. For this purpose, initially, the unipolar prosthesis was used but due to several disadvantages such as recurrent dislocation, decreased range of mobility, more wear, and friction of the acetabulum, they were superseded by the bipolar prosthesis. In agreement with reported literature, dislocation of the prosthesis is a known complication after primary hemiarthroplasty; however, disassembly of the implant is very rarely encountered, causing significant permanent disability. There is a 2.6% incidence of dislocation reported by Burge et al. [9] in hips treated with bipolar hemiarthroplasty. In the present case, the most vital cause for disassembly is the weakened bond between the cement and the metal-based socket. The advantages of cemented prostheses are improved post-operative outcome and low rates of implant-related complications such as dislocation, disassembly, or periprosthetic femoral fracture. However, the modular design of the cemented bipolar prosthesis can very rarely lead to disassembly of the components, and Ito et al. [10] reported a disassembly rate of 4% in the study. With this case report, we, hereby, present such a complication.
Conclusion
In summary, the dissociation of bipolar hemiarthroplasty is a complex complication that requires operative treatment. The mechanism and cause of failure should be identified before the operation. To prevent this condition, pre-operative planning and proper techniques should be done as an index procedure. Early diagnosis of this rare complication by orthopedic surgeons and its timely management by open reduction and revision surgery plays a crucial role in decreasing morbidity of the patient and its successful outcome. The post-operative radiographic examination should be kept routinely as a part of the treatment protocol with patients who have undergone bipolar hemiarthroplasty.
Clinical Message
Hip fracture is a universally well-known health problem which is managed by bipolar hemiarthroplasty. People are aware of its common complications. However, disassembly of the implant is a rare complication. By this report, we want to create awareness regarding this complication to modern generation orthopedics.
References
1. Royal College of Physicians. National Hip Fracture Database (NHFD) Annual Report. London: Royal College of Physicians; 2017. Available from: https://www.rcplondon.ac.uk/projects/outputs/national-hip-fracture-database-annual-report-2017. Accessed on 29 May, 2020.
2. National Health Service Scotland. Scottish Hip Fracture Audit: Hip Fracture Care Pathway Report 2017. Edinburgh, United Kingdom: NHS National Services Scotland; 2017. Available from: https://www.shfa.scot.nhs.uk/reports/_docs/2019-08-20-shfa-report.pdf. Accessed on 29 May,2020
3. Court-Brown C, McQueen MM, Tornetta P, Einhorn TA, editors. Trauma. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.
4. Hopley C, Stengel D, Ekkernkamp A, Wich M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: Systematic review. BMJ 2010;340:c2332.
5. Wang F, Zhang H, Zhang Z, Ma C, Feng X. Comparison of bipolar hemiarthroplasty and total hip arthroplasty for displaced femoral neck fractures in the healthy elderly: A meta-analysis. BMC Musculoskelet Disord 2015;16:229.
6. Carroll C, Stevenson M, Scope A, Evans P, Buckley S. Hemiarthroplasty and total hip arthroplasty for treating primary intracapsular fracture of the hip: A systematic review and cost-effectiveness analysis. Health Technol Assess 2011;15:1-74.
7. Broos PL. Prosthetic replacement in the management of unstable femoral neck fractures in the elderly. Analysis of the mechanical complications noted in 778 fractures. Acta Chir Belg 1999;99:190-4.
8. Plummer DR, Haughom BD, Valle CJ. Dual mobility in total hip arthroplasty. Orthop Clin North Am 2014;45:1-8.
9. Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 2007;22:465-75.
10. Ito H, Matsuno T, Kaneda K. Bipolar hemiarthroplasty for osteonecrosis of the femoral head. A 7-to 18-year follow-up. Clin Orthop Relat Res 2000;374:201-11.
 |
 |
 |
| Dr. Ruchit Shah | Dr. Urvi Khambhati | Mrs. Feral Daruwala |
| How to Cite This Article: Shah R, Khambhati U, Daruwala F. A Rare Case Report of Spontaneous Disassembly of Bipolar Hip Prosthesis in Elderly Patient. Journal of Orthopaedic Case Reports 2020 August;10(5): 75-77. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com