[box type=”bio”] Learning Point of the Article: [/box]
For distal ulna osteochondroma with radial bowing simultaneous radial correction is avoided as the radius will remodel with time.
Case Report | Volume 10 | Issue 6 | JOCR September 2020 | Page 14-17 | Amit Kumar Yadav, Mangal Parihar, Eknath D. Pawar, Sagar Bansal, Prasanna Kumar G. S., Abhishek Harsoor. DOI: 10.13107/jocr.2020.v10.i06.1856
Authors: Amit Kumar Yadav[1], Mangal Parihar[1], Eknath D. Pawar[1], Sagar Bansal[1], Prasanna Kumar G. S.[1], Abhishek Harsoor[1]
[1]Department of Orthopaedics, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India.
Address of Correspondence:
Dr. Amit Kumar Yadav,
Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India.
E-mail: amit_aur09@yahoo.com
Abstract
Introduction: Osteochondroma is the group of benign bone tumours, which are composed of spongy bone covered by a cartilaginous cap. Patients with distal ulnar osteochondromas frequently cause forearm deformities with relative ulnar shortening, wrist joint deviation, and varus bowing. Surgical ulnar lengthening is necessary to restore the carpal balance.
Case Report: We report the case of multiple exostosis in a 13-year-old male with the right distal ulna osteochondroma with long-standing and progressive ulnar shortening and radial bowing treated with a limb reconstruction system. Our case is Type I Masada managed with excision of distal ulna osteochondroma and gradual ulnar lengthening without osteotomy of the radius.
Conclusion: Progressive ulna deformity can lead to increasing pain, joint instability, limited motion, and functional decline. For Type I, Masada ulnar lengthening is necessary, but over correction is inadvisable due to possible ulnocarpal impaction syndrome. As significant remodeling effects on the radius were observed, simultaneous radial correction can be delayed.
Keywords: Distal ulna osteochondroma, Limb reconstruction system, Type I Masada.
Introduction
Hereditary multiple exostoses (HME) are a disorder of endochondral bone growth-producing abnormal metaphyseal bony prominences capped with cartilage which is accompanied by defective metaphyseal remodeling and asymmetrical retardation of longitudinal bone growth [1]. Multiple exostosis is a rare, autosomal dominant disorder caused by loss of function mutations in either the exostosin-1 (EXT1 on chromosome 8) or exostosin-2 (EXT2 on chromosome 11) gene [2]. EXT1 and EXT2 mutations are found in over 90 % of all multiple exostosis cases [3]. Unlike a case of solitary osteochondroma, the abnormal growth pattern of long bones with HME can lead to joint instability and severe deformities of the involved extremity. Approximately 30% to 60% of patients with HME have some form of forearm deformity [4]. A common presentation of forearm deformity with HME presents with radial bowing and progressive subluxation of the radiocapitellar joint secondary to relative ulnar shortening [5]. This could eventually lead to wrist instability, pain, compromised grip strength, and loss of forearm rotation. Early management of these deformities can yield satisfactory results [6]. Neglected or recalcitrant deformities pose a treatment challenge. Surgical lengthening of the ulna is considered necessary to restore the carpal balance [7]. Depending on the individual situation, ulnar lengthening is often combined with excision of exostosis and simultaneous radial correction procedures, such as hemiepiphysiodeses and osteotomies [8]. We report the case of a long-standing progressive forearm deformity secondary to underlying HME in an adolescent managed with ulnar lengthening with limb reconstruction system (LRS). At present (2 years follow-up), the patient had a satisfactory outcome with a fully functional, pain-free forearm, and wrist. We are still following up on the patient until skeletal maturity.
Case Report
A 13-year-old male presented with complaints of painless swelling which was insidious in onset and gradually progressive over the right distal forearm for 3 years. He had multiple bony swelling all over the body which was asymptomatic.
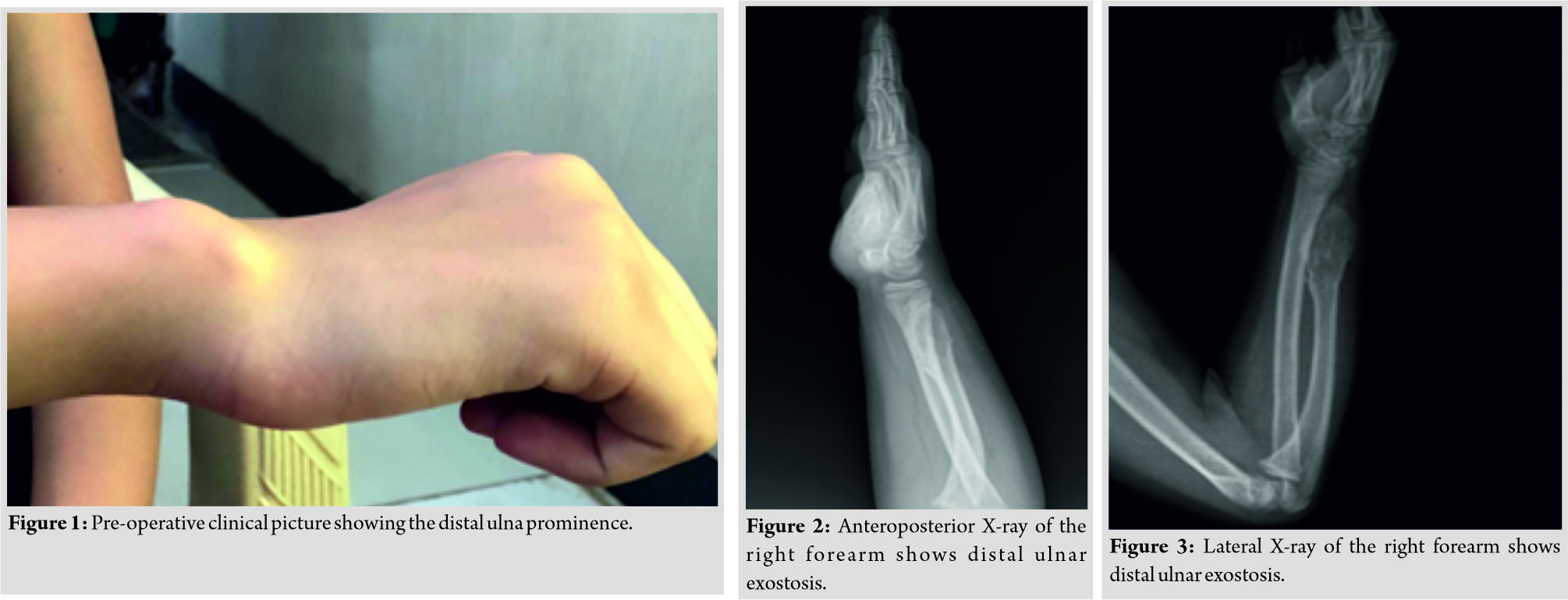
On examination of the right wrist, there was an ulnar deviation of the wrist, which was passively correctable. The distal radioulnar joint (DRUJ) was unstable. There was a palpable, non-tender, osseous prominence in the distal aspect of the ulna (Fig. 1). He had pain on the wrist range of motion and was unable to lift heavy objects. The skin over the affected site was normal with no distal neurovascular deficit. The examination of the ipsilateral elbow and other joints was normal.
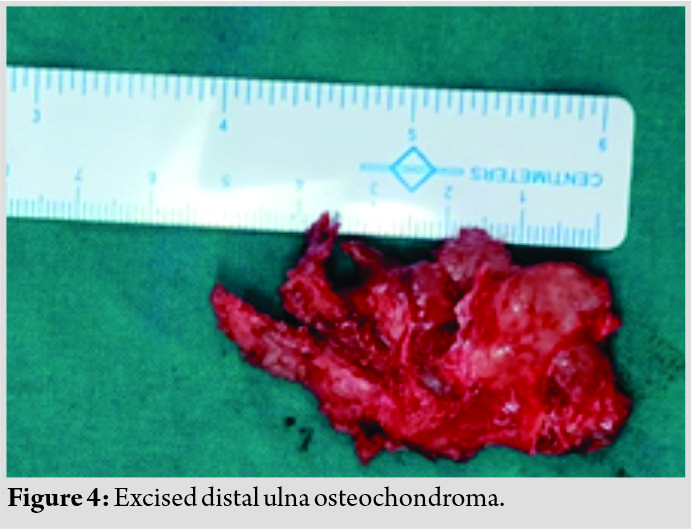
Anteroposterior and lateral radiographs of the right forearm show distal ulnar exostosis approximately 5*2 cm in size which was Type I according to Masada classification (Fig. 2, 3). At the wrist, a negative ulnar variance of 15 mm was observed. There was substantial radial bowing compared to the contralateral side and the length of the ulna was 3 cm shorter.
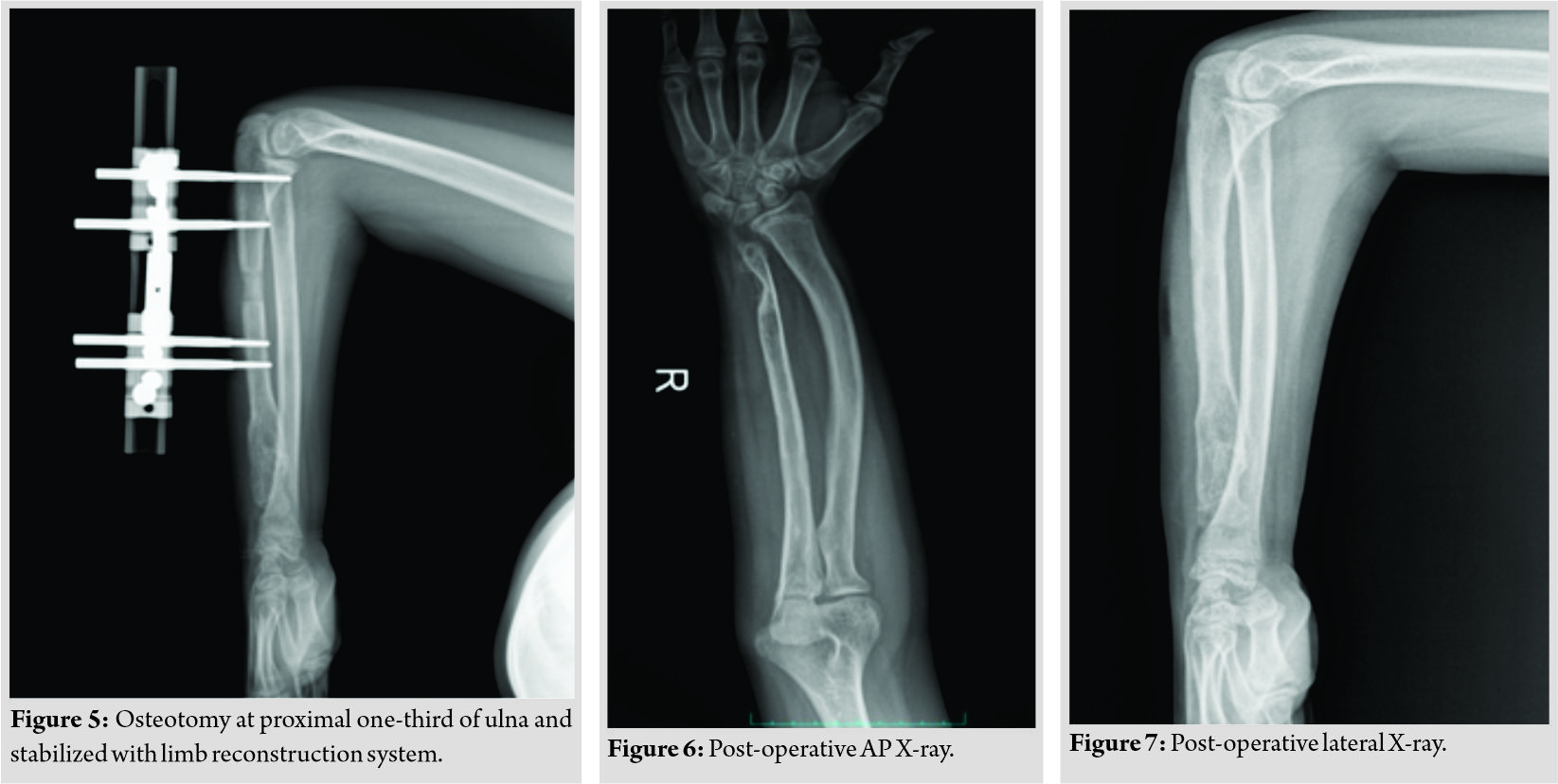
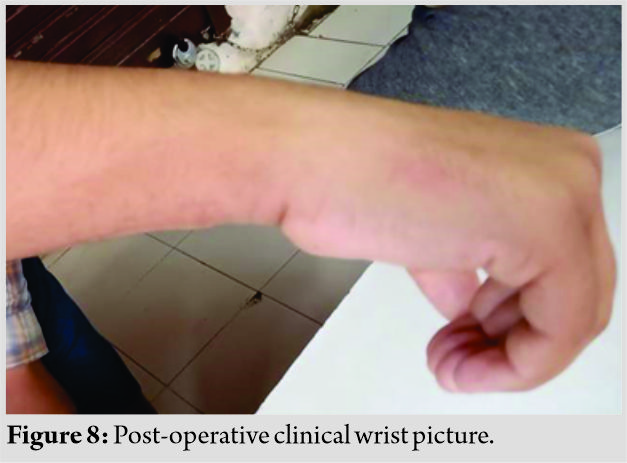
The patient was planned for excision of distal ulna osteochondroma through the Volar approach of the ulna (Fig. 4). The osteotomy was done at proximal one-third of the ulna and was stabilized with LRS (two-pin above and two-pin below) and gradual ulnar lengthening was done (Fig. 5). Deformity of the radius was not corrected as it will itself get remodeled with time (Fig. 6, 7). Postoperatively, the full range of motion of wrist and elbow is present (Fig. 8). DRUJ is stable at subsequent follow-up, no additional procedure was done for DRUJ. We are still following up on the patient until skeletal maturity.
Discussion
Firstly described by Sir Astley Cooper in 1818, osteochondromas are the largest group of benign bone tumors, which are composed of spongy bone covered by a cartilaginous cap [9]. This tumor is usually seen in patients in the adolescent age group with no effective predilection according to sex. The cause of osteochondroma remains unknown. Many theories have been proposed to explain the etiology of osteochondroma, all of them relating to alterations to the growth plate [10]. Recent research has indicated that multiple osteochondromas are an autosomal dominant inherited disease. Germline mutations in EXT1 and EXT2 genes located on chromosomes 8 and 11 have been associated with the cause of the disease [11]. Although it is the most common benign tumour of bone accounting for 35–40% of all benign bone tumors, it usually occurs in long bones. The tumors are thought to arise through a process of progressive endochondral ossification of aberrant cartilage of a growth plate. The rate of forearm involvement in these patients has been estimated to be <60%. The spectrum of forearm deformities ranges from the presence of a single asymptomatic osteochondroma to severe forearm bowing and radial head dislocation with substantial functional deficits.
These forearm deformities were classified by Masada et al. as follows:
• Type I ulnar shortening and bowing of the radius secondary to osteochondroma of the distal ulna
• Type II in addition to ulnar shortening, the radial head is dislocated. Bowing of the radius is less severe than in Type I deformity due to the dislocation
• Type IIa radial head is dislocated due to an osteochondroma at the proximal radius
• Type IIb more distal involvement of radius
• Type III main osteochondroma formation is in the metaphysis of the distal radius, and there is a relative shortening of the radius.
Indications for surgical management of these deformities include wrist instability, loss of elbow and forearm function, pain, and progressive increase in deformity. The surgical treatment options are varied depending on the type of deformity-
• Type I excision of osteochondroma, osteotomy of radius, and immediate ulnar lengthening
• Type IIa excision of osteochondroma, osteotomy of radius, and immediate ulnar lengthening excision of the radial head
• Type IIb excision of osteochondroma, osteotomy of radius, and gradual ulnar lengthening
• Type III excision of osteochondroma.
A study by Yip et al. on 5 cases with a mean age at operation 10.4 years and mean follow-up of 72 months had shown that excision of distal ulnar exostosis improves forearm rotation, radial articular angle, carpal slip, and ulnar variance [12]. A case report by Utomo et al. of a 14-year-old girl a case of multiple hereditary exostosis of the distal ulna with dislocation of the radial head shows that simple excision could improve the range of movement of the forearm but would not stop the progression of the disease [13]. Another study by Cho and Jung on four cases of multiple hereditary exostosis with dislocation of radial head treated with excision of osteochondroma and gradual lengthening of the ulna with an Ilizarov fixator reported improvement in pronation/supination, radial bowing, and ulnar shortening [14]. Beutel et al. reported a case report of distal ulna exostosis in an 11-year-old male showed that ulnar osteotomy and lengthening is successful. They recommend corrective surgery near skeletal maturity [15]. Our case is Type I Masada managed with excision of distal ulna osteochondroma and gradual ulnar lengthening without osteotomy of the radius. Radius deformity was remodeled with time and the patient had full wrist and elbow range of motion.
Conclusion
We conclude that for Type I Masada ulnar lengthening is necessary, but over correction is inadvisable due to possible ulnocarpal impaction syndrome. As significant remodeling effects were observed on the radius at a young age, simultaneous radial correction procedures can be delayed.
Clinical Message
For progressive, ulna deformity due to exostosis LRS is one of the treatment options. In ulnar lengthening, overcorrection is always avoided.
References
1. Akita S, Murase T, Yonenobu K, Shimada K, Masada K, Yoshikawa H. Long-term results of surgery for forearm deformities in patients with multiple cartilagenous exostosis. J Bone Joint Surg Am 2007;89:1993-9.
2. Wuyts W, van Hul W, Wauters J, Nemtsova M, Reyniers E, Van Hul EV, et al. Positional cloning of a gene involved in hereditary multiple exostoses. Hum Mol Genet 1996;5:1547-57.
3. Jennes I, Pedrini E, Zuntini M, Mordenti, M Balkassmi S, Asteggiano CG, et al. Multiple osteochondromas: Mutation update and description of the multiple osteochondromas mutation database. Hum Mutat 2009;30:1620-7.
4. Shapiro F, Simon S, Glimcher MJ. Hereditary multiple exostoses. Anthropometric, roentgenographic, and clinical aspects. J Bone Joint Surg Am 1979;61:815-24.
5. Masada K, Tsuyuguchi Y, Kawai H, Kawabata H, Noguchi K, Ono K. Operations for forearm deformity caused by multiple osteochondromas. J Bone Joint Surg Br 1989;71:24-9.
6. Matsubara H, Tsuchiya H, Sakurakichi K, Yamashiro T, Watanabe K, Tomita K, et al. Correction and lengthening for deformities of the forearm in multiple cartilaginous exostoses. J Orthop Sci 2006;11:459-66.
7. Ettl V, Wild A, Thorey F, Kirschner S, Krauspe R, Raab P. Correction of forearm deformities in children with multiple cartilaginous osteochondromas. Z Orthop Ihre Grenzgeb 2005;143:106-11.
8. Fogel GR, McElfresh EC, Peterson HA, Wicklund PT. Management of deformities of the forearm in multiple hereditary osteochondromas. J Bone Joint Surg Am 1984;66:670-80.
9. Schramm G. Pathogenesis of cartilaginous exostoses and enchondromas. Arch Orthop 1929;27:421.
10. D’Ambrosia R, Ferguson AB Jr. The formation of osteochondroma by epiphyseal cartilage transplantation. Clin Orthop Relat Res 1968;61:103-15.
11. Zhang F, Liang J, Guo X, Zhang Y, Wen Y, Li Q, Zhang Z, Ma W, Dai L, Liu X, Yang L. Exome sequencing and functional analysis identifies a novel mutation in EXT1 gene that causes multiple osteochondromas. PLoS One. 2013 Aug 29;8(8):e72316.
12. Yip LC, Choi AK, Tak CP, Yin CY. Excision of distal ulnar exostosis: A case series and literature review. J Orthop Trauma Rehabil 2018;25:49-53.
13. Utomo P, Idulhaq M, Brilianto BI. Multiple hereditary exostosis of distal ulna with dislocation of radial head: A case report. Indones J Med 2020;5:63-9.
14. Cho YJ, Jung ST. Gradual lengthening of the ulna in patients with multiple hereditary exostoses with a dislocated radial head. Yonsei Med J 2014;55:178-84.
15. Beutel BG, Klifto CS, Chu A. Timing of forearm deformity correction in a child with multiple hereditary exostosis. Am J Orthop 2014;43:422-5.
 |
 |
 |
 |
 |
 |
| Dr. Amit Kumar Yadav | Dr. Mangal Parihar | Dr. Eknath D. Pawar | Dr. Sagar Bansal | Dr. Prasanna Kumar G. S. | Dr. Abhishek Harsoor |
| How to Cite This Article: Yadav AK, Parihar M, Pawar ED, Bansal S, Kumar GSP, Harsoor A. Management of Forearm Deformity by Limb Reconstruction System in Children with Multiple Exostosis – A case Report. Journal of Orthopaedic Case Reports 2020 September;10(6): 14-17. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com