[box type=”bio”] Learning Point of the Article: [/box]
Severe radiculopathy and trunk imbalance can be caused by the extremely rare association of lumbar osteoblastoma and aneurysmal bone cyst; surgeons must know this and be ready to appropriately treat it.
Case Report | Volume 10 | Issue 6 | JOCR September 2020 | Page 18-22 | Carlo Iorio, Osvaldo Mazza, Federico Tundo, Alessandra Stracuzzi, Marco Crostelli. DOI: 10.13107/jocr.2020.v10.i06.1858
Authors: Carlo Iorio[1], Osvaldo Mazza[1], Federico Tundo[1], Alessandra Stracuzzi[2], Marco Crostelli[1]
[1]Spine Surgery Unit, Department of Surgery, Bambino Gesù Pediatric Hospital, Piazza sant’Onofrio 4, 00191, Rome, Italy,
[2]Pathological Anatomy Unit, Department of Diagnostic and Laboratory Medicine, Bambino Gesù Pediatric Hospital, Piazza sant’Onofrio 4, 00191, Rome, Italy.
Address of Correspondence:
Dr. Carlo Iorio,
Spine Surgery Unit, Bambino Gesù Pediatric Hospital, Piazza Sant’Onofrio, 4, 00165 Rome, Italy.
E-mail: carlo.iorio@opbg.net
Abstract
Introduction: Osteoblastomas are primary bone tumors, rarer than osteoid osteomas, and <10% of these lesions occurs in the spine. Aneurysmal bone cysts (ABCs) are rare, benign lesion of the bone and approximately 8–30% of ABCs arise in the spine, mostly in the thoracic and the lumbar regions. The association between them is quite rare in the general population.
Case Report: We report a case of a 14-year-old boy, soccer player, with an osteoblastoma of the left posterior neural arc of L2 and a secondary aneurismal bone cyst compressing the left L2 nerve root, causing severe antalgic scoliosis and back pain with radiculopathy. A complete surgical excision with radicular decompression has been performed, and the histologic examination confirmed the diagnostic hypothesis (osteoblastoma + ABC). At 6 months follow-up, the patient presented a complete resolution of symptoms, but the trunk imbalance was not completely resolved.
Conclusion: Spine localization of osteoblastoma + ABC is rare and its diagnosis and treatment are often challenging. Complete surgical excision seems to be confirmed as the gold standard of treatment, but the option of instrumented arthrodesis should be carefully evaluated.
Keywords: Osteoblastoma, aneurysmal bone cyst, antalgic scoliosis, trunk imbalance.
Introduction
Osteoblastomas are primary bone tumors, rarer than osteoid osteomas, and <10% of these lesions occurs in the spine [1, 2, 3, 4]. They were first described by Lichtenstein in the 1950s [5] and are commonly located in the posterior elements involving the pedicle and lamina, tending to predominate during the 2nd decade of life [6]. Classical X-ray and computed tomography (CT) scan finding include matrix calcifications, radiolucent nidus, and surrounding osseous sclerosis. Pain, which is the most common presenting symptom, is generally unresponsive to aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs); however, they can occasionally cause pathological fracture or neurological deficits, as well as antalgic scoliosis [7]. Aneurysmal bone cysts (ABCs) are rare, benign lesion of the bone and approximately 8–30% of ABCs arise in the spine, mostly in the thoracic and the lumbar regions [8, 9]. Although ABCs are generally considered to have a non-neoplastic origin, they are expansile tumors containing thin-walled, blood-filled cystic cavities that frequently affect the pediatric population [4]. Similarly to osteoblastomas, ABCs most commonly affect the posterior elements of the spine; they also present potential extension into the vertebral bodies, neural foramina, and spinal canal [10]. The association between osteoblastoma and ABC is quite rare in the general population [9, 11], and it’s even rarer when localized in the lumbar spine. We report a case of a 14-year-old boy with an osteoblastoma of the left posterior neural arc of L2 and a secondary ABC compressing the left L2 nerve root, causing severe coronal trunk imbalance and back pain with radiculopathy.
Case Report
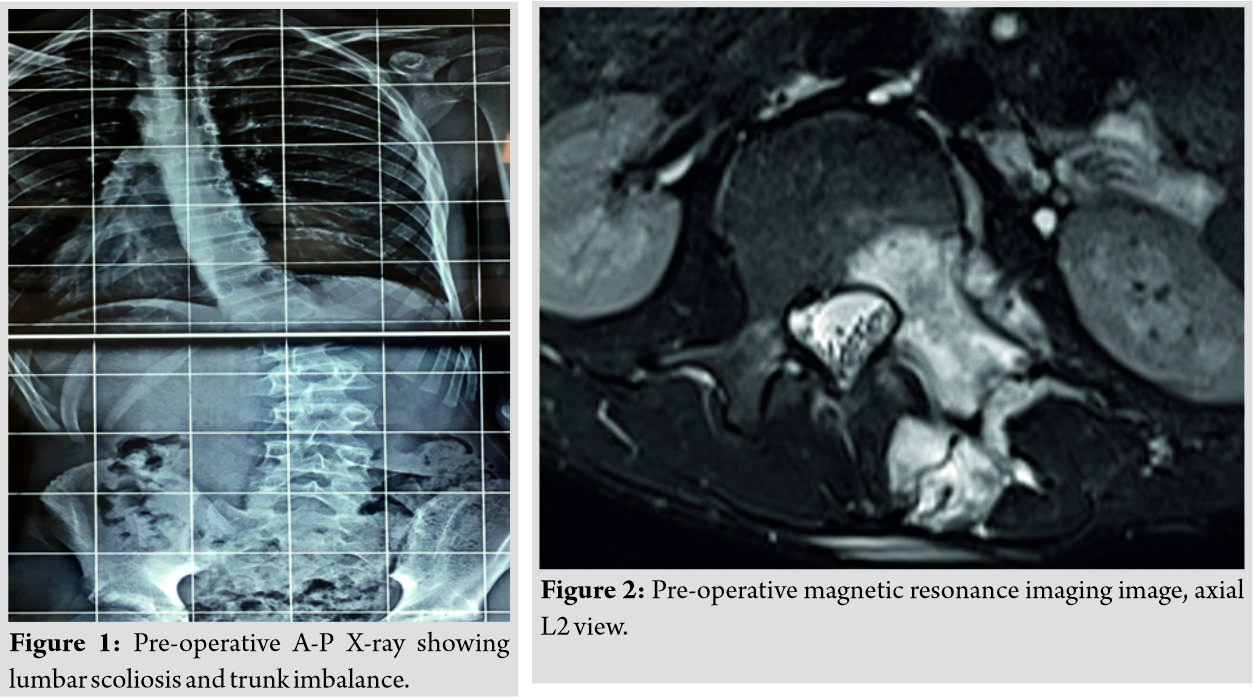
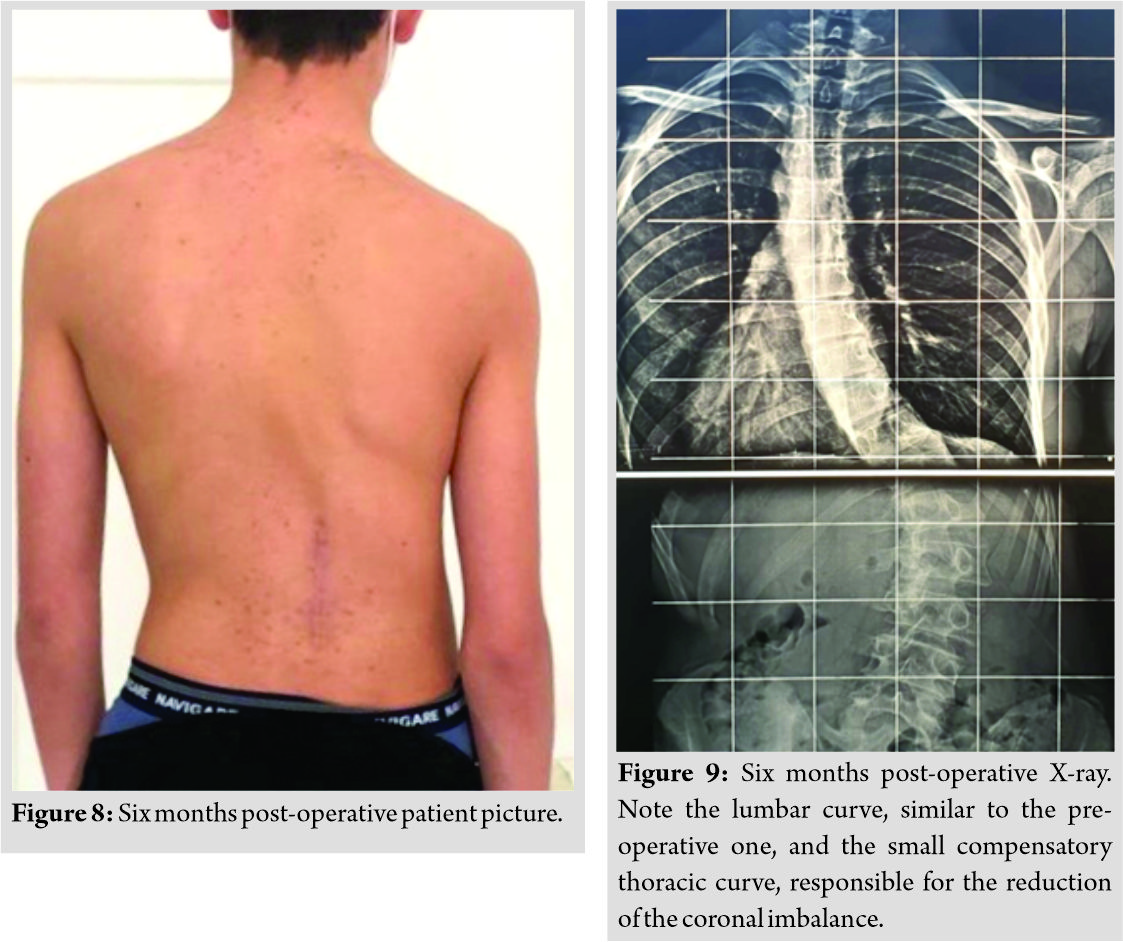
A 14-year-old boy, with nothing relevant in his medical history, came to our observation for a strong back pain associated to a right lumbar scoliosis and a severe coronal imbalance (Fig. 1). The pain started almost 1 year before, after a playing soccer. He was first treated by a physiatrist, who prescribed postural gymnastics, swimming, and physiotherapy. Then, a thoracolumbosacral orthosis (TLSO) was prescribed too (after the scoliosis was diagnosed).
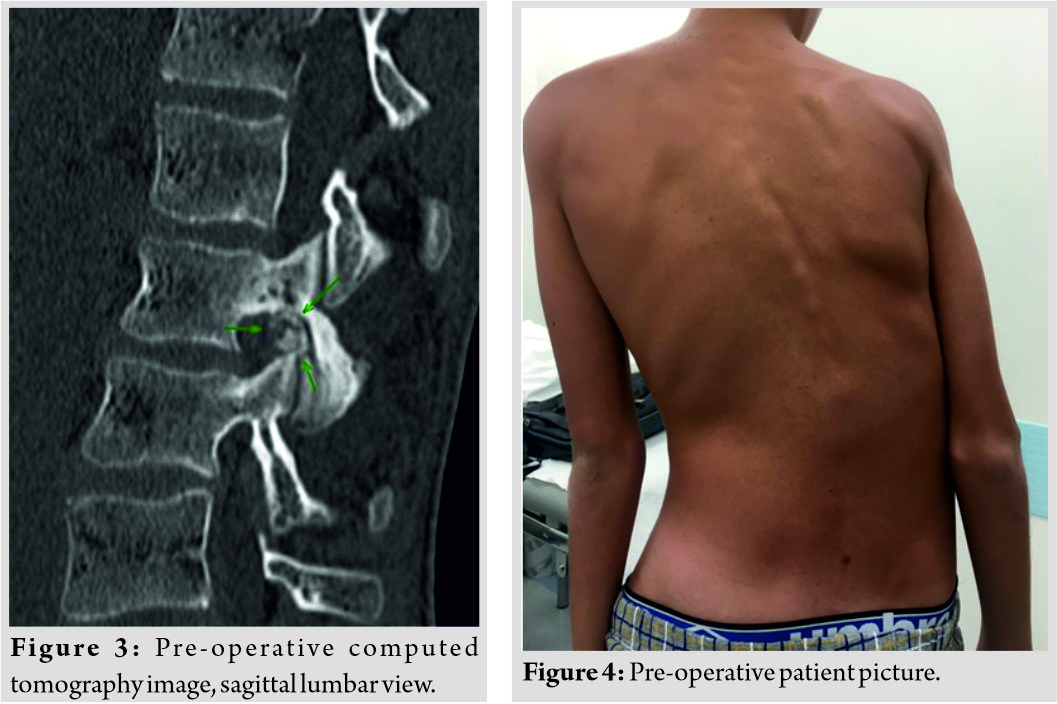
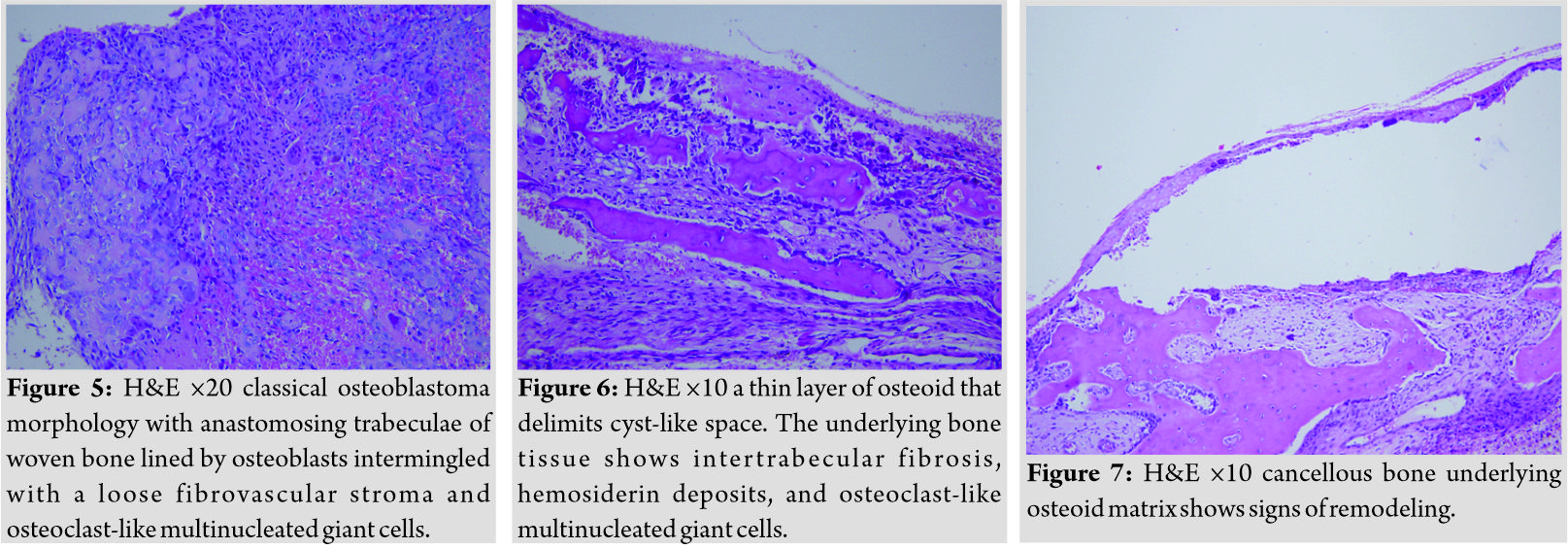
As he was referred to us, an MRI and a CT scan were prescribed, and the radiological report stated as follows: “Findings orientate to a slow-growing expansive lesion with wear of the L2-L3 arcal structures on the left. It could be an osteoblastoma of the left neural hemiarch of L2 with associated cyst-type hematological lesion ABC (secondary ABC) in intraforaminal development with compression of the L2 root in the intraforaminal area” (Fig. 2, 3).
Clinically, he presented an important trunk imbalance (Fig. 4), a severe lumbar pain with irradiation to the proximal third of the thigh. The patient has been operated by posterior approach wide excision of the lesion with removal of left inferior L1 articular process, of left L2 hemilamina to the basis of the left L2 pedicle, and of left L3 superior articular process; excision interested whole bone cyst compressing intraforaminal tract of the left L2 nervous root; wide excision of bony structures with excision margins within healthy bone tissue assures best chance of removing the entire lesion minimizing local recurrence risks.
After bone structures excision, soft tissues that surrounded left L2 nervous root have been removed too, as to completely free the root, leaving nervous structure without any compression. The patient experienced no post-surgical complications and was discharged after 2 days from the procedure. A TLSO was prescribed for the first 6 weeks. At the 6 months follow-up control, the patient was completely pain free, he returned to all his previous sport activity. The trunk imbalance was still slightly noticeable (Fig. 8) and the X-rays showed a similar lumbar curve with a small compensatory thoracic curve that reduced the coronal imbalance (Fig. 9).
Histology
Histological examination showed a classic osteoblastoma. At scanning magnification, we observed a thin layer of osteoid matrix that delimited a cyst-like space. The bone tissue underlying this lesion showed remodeling, intertrabecular fibrosis, hemosiderin deposits, and osteoclast-like multinucleated giant cells. According to the radiological data, a diagnosis of osteoblastoma with a secondary hemorrhagic cyst was rendered (Fig. 5, 6, 7).
Discussion
Osteoblastomas of the spine typically affect the pediatric population, predominately children 10–15 years of age [12] and, unlike most other primary osseous tumors, typically arise in the spine [13]. Some studies have reported equal frequency of these tumors in the cervical, thoracic, and lumbar spine [14]. On plain radiographs, osteoblastomas are typically radiolucent [12]. They can have variable features, though. One pattern of representation is similar to osteoid osteomas, with a radiolucent nidus and surrounding sclerotic changes. A CT scan may reveal calcification and mineralization of the nidus, while another pattern, which is the most common, involves an expansile lesion with several small calcifications and a prominently sclerotic rim [12]. Histologically, osteoblastomas display both osteoblastic and osteolytic characteristics. They generally are 2 cm or larger in maximal diameter, and only the nidus is taken into consideration when drawing conclusions about their size. The average size of an osteoblastoma is 3–4 cm, and those isolated to the sacrum are often much larger [15]. As they are the more aggressive counterparts of osteoid osteomas, osteoblastomas tend to respond less robustly to NSAIDs [16] and they are quite frequently associated to scoliosis, especially in males [12, 17], like in our patient. The curvature is thought to arise as a reaction to pain and the convex side of the scoliotic curve is often contralateral to the lesional side of the spinal column [12, 18]. ABCs are non-neoplastic, primarily vascular lesions characterized by thin-walled, blood-filled cystic cavities, usually occurring during adolescence (80% before 20 years of age). Like in osteoblastomas, males are slightly more affected than females and their most common symptom is local pain [7]. ABCs can be located in all bone types and often found in femur, tibia, and small bones of the hands and feet [9]. Approximately 8%–30% of ABCs arise in the spine, mostly in the thoracic and the lumbar regions [8, 9]. In gross, the lesion consists of a soft fibrovascular core containing blood-filled cyst-like cavities surrounded by a bone shell [8] and some patients present neurologic dysfunction due to cord compression and spinal instability [9]. On rare occasions, some of these bone cysts become quiescent or undergo spontaneous regression. Progressive growth appears the more common clinical scenario [4]. On histologic examination, fibroblasts, multinucleated osteoclast-like giant cells, immature trabecular bone, hemosiderin granules, macrophages, and thin capillary vasculature are typically observed [8, 10, 19]. ABCs on plain films demonstrate a “blown-out” lytic expansile lesion [20]. CT studies demonstrate septated lesions surrounded by normal cortical bone [10]. Gross resection is the optimal treatment for both osteoblastomas and ABCs [4, 8, 21]. In ABC cases, it could be associated to a pre-operative adjuvant selective arterial embolization, as it reduces operative blood loss, while chemotherapy and radiation seem to have limited use [4, 22]. It is, however, important to note how fatalities have been reported with selective arterial embolization, especially on cervical spine lesions [23]. Total excision of an osteoblastoma has been shown reducing relapse rates [24] as well as to have a more favorable outcome compared to subtotal excision (curettage) combined with radiation therapy [12]. Indeed, the gold standard of treatment is complete surgical excision of both osteoblastoma and ABCs to offer the best chance for cure and reduce the risk of recurrence [7, 9]. We decided not to perform scoliosis correction with instrumentation due to the fact that the patient’s symptoms arise <15 months before [25], and in our previous experiences, we obtained good results in most cases without performing instrumented vertebral arthrodesis, especially in those early diagnosed and treated [26]. Furthermore, in this case, it has been not possible for us to establish whether the patient had a “true” scoliosis or an antalgic one, as he was referred to us only after the X-rays showing lumbar scoliosis were made. To the best of our knowledge, this is the first reported case of such a severe coronal trunk imbalance caused by an association of osteoblastoma and ABC of the lumbar spine. Our 6 months results (persistent slight clinical coronal imbalance and a similar 6 months post-operative lumbar curve) may strengthen the hypothesis that long-term course of antalgic scoliosis development should be addressed with surgical correction and posterior instrumented arthrodesis, and the limit defining “long-term” should be probably reduced to 12 months.
Conclusion
Spine localization of osteoblastoma + ABC is rare and its diagnosis and treatment are often challenging. Complete surgical excision seems to be confirmed as the gold standard of treatment, but the option of instrumented arthrodesis should be carefully evaluated.
Clinical Message
The rare association of osteoblastoma and ABC in the lumbar spine should be considered when in the presence of back pain with trunk imbalance. Most appropriate treatment choice is often arduous and has to be rapidly but carefully planned.
References
1. Kan P, Schmidt MH. Osteoid osteoma and osteoblastoma of the spine. Neurosurg Clin N Am 2008;19:65-70.
2. Zileli M, Cagli S, Basdemir G, Ersahin Y. Osteoid osteomas and osteoblastomas of the spine. Neurosurg Focus 2003;15:E5.
3. Flemming DJ, Murphey MD, Carmichael BB, Bernard SA. Primary tumors of the spine. Semin Musculoskelet Radiol 2000;4:299-320.
4. Harrop JS, Schmidt MH, Boriani S, Shaffrey CI. Aggressive benign primary spine neoplasms osteoblastoma, aneurysmal bone cyst, and giant cell tumor. Spine (Phila Pa 1976) 2009;34:S39-47.
5. Lichtenstein L. Benign osteoblastoma; a category of osteoid-and bone-forming tumors other than classical osteoid osteoma, which may be mistaken for giant-cell tumor or os-teogenic sarcoma. Cancer 1956;9:1044-52.
6. Mishra A, Pruthi N, Nandeesh BN, Shukla D. Cervical spine osteoblastoma with an aneurysmal bone cyst in a 2-year-old child: A case report. Pediatr Neurosurg 2019;54:46-50.
7. Pavanello M, Melloni I, Fiaschi P, Consales A, Piatelli G, Ravegnani M, et al. A rare case of osteoblastoma associated to aneurysmal bone cyst of the spine. Case report. Br J Neurosurg 2016;30:106-9.
8. Boriani S, De Iure F, Campanacci L, Gasbarrini A, Bandiera S, Biagini R, et al. Aneurysmal bone cyst of the mobile spine: Report on 41 cases. Spine (Phila Pa 1976) 2001;26:27-35.
9. Hu H, Wu J, Ren L, Sun X, Li F, Ye X. Destructive osteoblastoma with secondary aneurysmal bone cyst of cervical vertebra in an 11-year-old boy: Case report. Int J Clin Exp Med 2014;7:290-5.
10. Ramme AJ, Smucker JD. Balancing spinal stability and future mobility in the cervical spine: Surgical treatment of a case of osteoblastoma with secondary aneurysmal bone cyst. Spine J 2011;11:e5-12.
11. Rocca CD, Huvos AG. Osteoblastoma: Varied histological presentations with a benign clinical course. An analysis of 55 cases. Am J Surg Pathol 1996;20:841-50.
12. Galgano MA, Goulart CR, Iwenofu H, Chin LS, Lavelle W, Mendel E. Osteoblastomas of the spine: A comprehensive review. Neurosurg Focus 2016;41:E4.
13. Boriani S, Weinstein JN. Oncologic Classification of Vertebral Neoplasms. New York: Thieme; 2006.
14. Jacobs WB, Fehlings MG. Primary Vertebral Column Tumors. New York: Thieme; 2006.
15. Pobiel R, Pitt A. Radiologic Imaging of Tumors of the Spine, Spinal Cord, and Peripheral Nerves. New York: Thieme; 2006.
16. Nemoto O, Moser RP Jr., Van Dam BE, Aoki J, Gilkey FW. Osteoblastoma of the spine. A review of 75 cases. Spine (Phila Pa 1976) 1990;15:1272-80.
17. Akbarnia BA, Rooholamini SA. Scoliosis caused by benign osteoblastoma of the thoracic or lumbar spine. J Bone Joint Surg Am 1981;63:1146-55.
18. Nguyen VD, Hersh M. A rare bone tumor in an unusual location: Osteoblastoma of the vertebral body. Comput Med Imaging Graph 1992;16:11-6.
19. Liu JK, Brockmeyer DL, Dailey AT, Schmidt MH. Surgical management of aneurysmal bone cysts of the spine. Neurosurg Focus 2003;15:E4.
20. Burch S, Hu S, Berven S. Aneurysmal bone cysts of the spine. Neurosurg Clin N Am 2008;19:41-7.
21. Marsh BW, Bonfiglio M, Brady LP, Enneking WF. Benign osteoblastoma: Range of manifestations. J Bone Joint Surg Am 1975;57:1-9.
22. Guibaud L, Herbreteau D, Dubois J, Stempfle N, Bérard J, Pracros JP, et al. Aneurysmal bone cysts: Percutaneous embolization with an alcoholic solution of zein-series of 18 cases. Radiology 1998;208:369-73.
23. Peraud A, Drake JM, Armstrong D, Hedden D, Babyn P, Wilson G. Fatal ethibloc embolization of vertebrobasilar system following percutaneous injection into aneurysmal bone cyst of the second cervical vertebra. Am J Neuroradiol 2004;25:1116-20.
24. Yin H, Zhou W, Yu H, Li B, Zhang D, Wu Z, et al. Clinical characteristics and treatment options for two types of osteo-blastoma in the mobile spine: A retrospective study of 32 cases and outcomes. Eur Spine J 2014;23:411-6.
25. Pettine KA, Klassen RA. Osteoid-osteoma and osteoblastoma of the spine. J Bone Joint Surg Am 1986;68:354-61.
26. Crostelli M, Mazza O. Spinal column tumors: Osteoblastomas and osteoid osteoma. In: Landi A, Gregori F, Delfini R, editors. Spinal Cord and Spinal Column Tumors. Ch. 30. New York: Nova Medicine and Health; 2019.
 |
 |
 |
 |
 |
| Dr. Carlo Iorio | Dr. Osvaldo Mazza | Dr. Federico Tundo | Dr. Alessandra Stracuzzi | Dr. Marco Crostelli |
| How to Cite This Article: Iorio C, Mazza O, Tundo F, Stracuzzi A, Crostelli M. Lumbar Spine Osteoblastoma with Secondary Aneurysmal Bone Cyst Causing Severe Trunk Imbalance and Radiculopathy: A Case Report. Journal of Orthopaedic Case Reports 2020 September;10(6): 18-22. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com