[box type=”bio”] Learning Point of the Article: [/box]
Importance of secondary survey in the context of even minor trauma to rule out concurrent injuries in pediatrics.
Case Report | Volume 10 | Issue 6 | JOCR September 2020 | Page 64-67 | Wan Wei Ang, Alexander Overton, Mudussar A Ahmad. DOI: 10.13107/jocr.2020.v10.i06.1878
Authors: Wan Wei Ang[1], Alexander Overton[1], Mudussar A Ahmad[1]
[1]Department of Trauma and Orthopaedic Surgery, Whittington Hospital, London, N19 5NF, United Kingdom.
Address of Correspondence:
Dr. Wan Wei Ang,
Department of Trauma and Orthopaedic Surgery, Whittington Hospital, London, N19 5NF, United Kingdom.
E-mail: wanwei.ang@nhs.net
Abstract
Introduction: Lateral condyle fractures and both bone forearm fractures account for 10–15% and 13–40% of all elbow fractures in children, respectively. About 5% of forearm fractures in children have associated supracondylar fractures; hence, any forearm fractures warrant a careful examination of the elbow, and any radiographs taken should visualize the elbow joint above and wrist joint below for other injuries. We report a case of multiple upper limb fracture in a child, comprising lateral condyle and both bone forearm fractures.
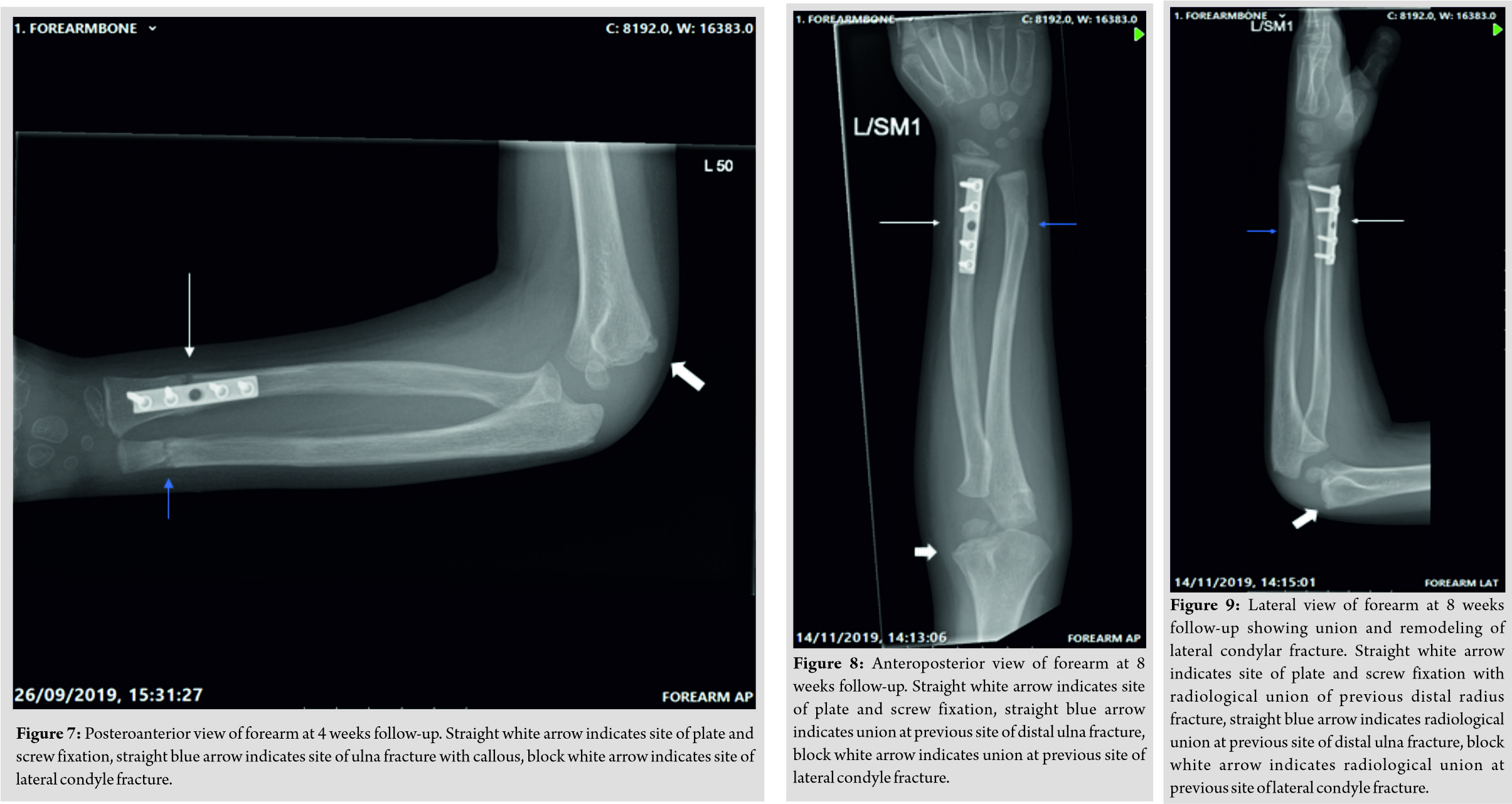
Case Report: A 5-year-old boy was admitted through the emergency department at our district general hospital having fallen from a ladder approximately 1.5 m high in a playground. The limb was significantly deformed, with no evidence of an open injury, and remained neurovascularly intact throughout. Radiographs demonstrated a minimally displaced lateral condyle fracture of the left elbow, a midshaft ulna fracture, and a displaced off-ended distal third radius and ulna fracture of the left wrist. Any metabolic bone disease and non-accidental injury was ruled out. The patient was initially managed in an above elbow plaster cast, with elevation and monitoring for any neurovascular compromise. Computed tomography imaging was performed to completely assess the fracture pattern and for discussion with our local regional trauma center. Given the minimal displacement of the lateral condyle fracture, a conservative course of management was decided for this. The displaced distal radial fracture was managed with open reduction and internal fixation with a plate and the ulna shaft fracture with manipulation and plaster cast application. By 12 weeks after surgery, there was a full range of movement of the elbow, wrist, and forearm with complete radiological union.
Conclusion: This case emphasizes the importance of a secondary survey in the context of even minor trauma to rule out concurrent injuries. We found that minimally displaced lateral condyle fractures can be managed conservatively, and single-bone fixation in both bone forearm fractures can lead to very satisfactory outcome, with preference for plate and screw fixation for unstable fractures within the metaphyseal/diaphyseal junction.
Keywords: Pediatric, multiple fracture, upper limb, fixation, lateral condyle.
Introduction
Lateral condyle fractures and both bone forearm fractures account for 10–15% and 13–40% of all elbow fractures in children, respectively [1, 2]. Approximately 18% of pediatric forearm fractures occur in the middle third, and these are the most common sites for refracture and pediatric open fractures [3, 4]. Kocher et al. demonstrated that 5% of forearm fractures in children have associated supracondylar fractures; hence, any forearm fracture warrants a careful examination of the elbow, and any radiographs taken should visualize the elbow joint above and wrist joint below for other injuries [5]. The mechanism of both bone forearm injuries tends to be fall onto an outstretched hand, whereas lateral condyle fractures are usually due to sudden traction of the common extensor origin by the extensor muscles, or when an axial load is transmitted through the forearm during a fall, resulting in the radial head crushing onto the lateral condyle [6, 7]. There is no published incidence of concurrent forearm and specifically a lateral condyle fracture, as the majority of lateral condyle fracture occur in isolation [7]. Even though there is widely published literature on the management of both bone forearms and lateral condyle fracture, respectively, there are limited studies on the management of concurrent forearm and lateral condyle fractures in children [2, 7, 8, 9].
Case Report
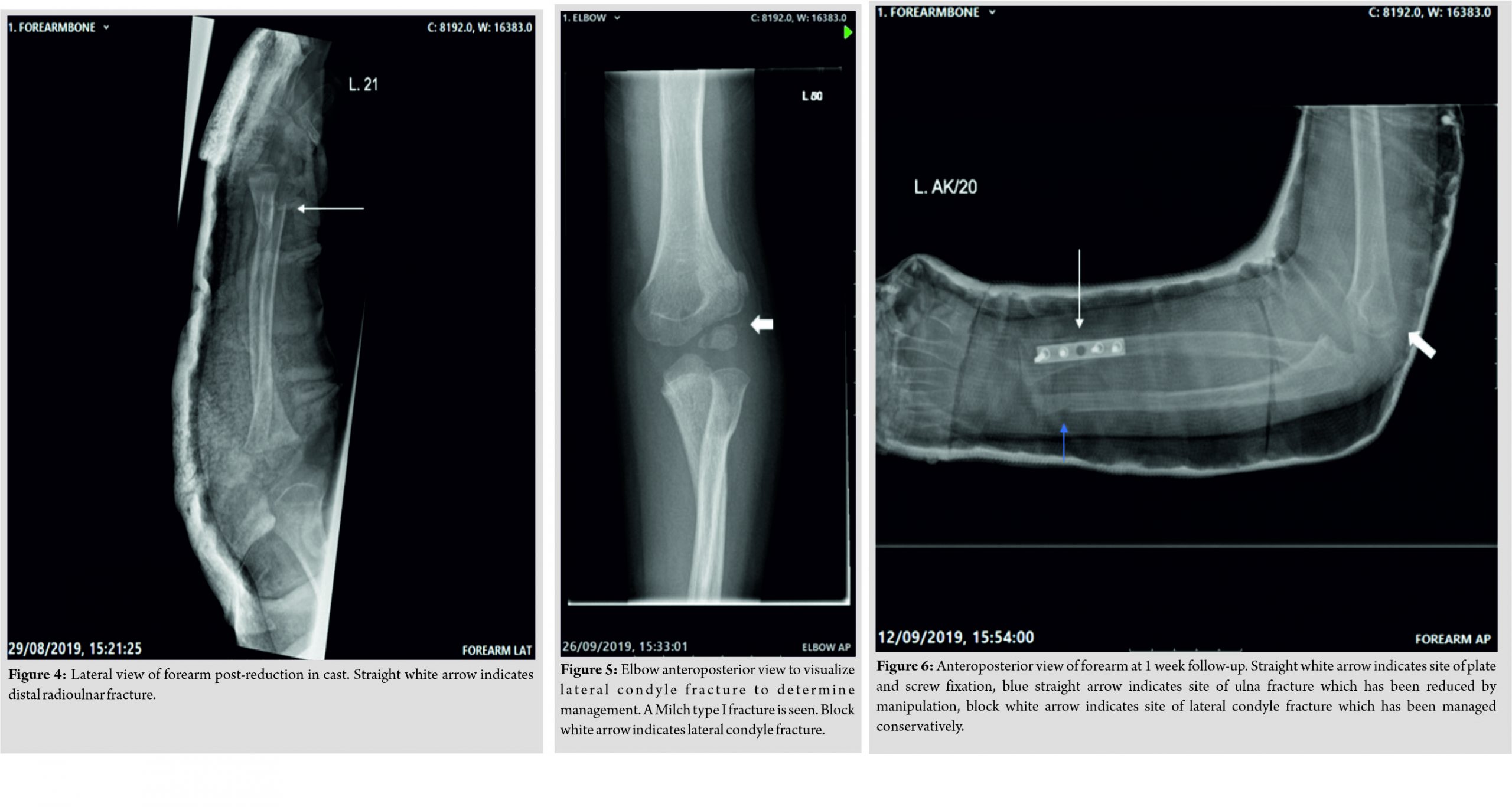
A 5-year-old boy was admitted through the emergency department at our district general hospital having fallen in a playground from a ladder approximately 1.5 m high. The limb was significantly deformed, with no evidence of an open injury, and remained neurovascularly intact throughout. Radiographs demonstrated a minimally displaced lateral condyle fracture of the left elbow, a midshaft ulna fracture, and a displaced off-ended distal third radius and ulna fracture of the left wrist (Fig. 1, 2). 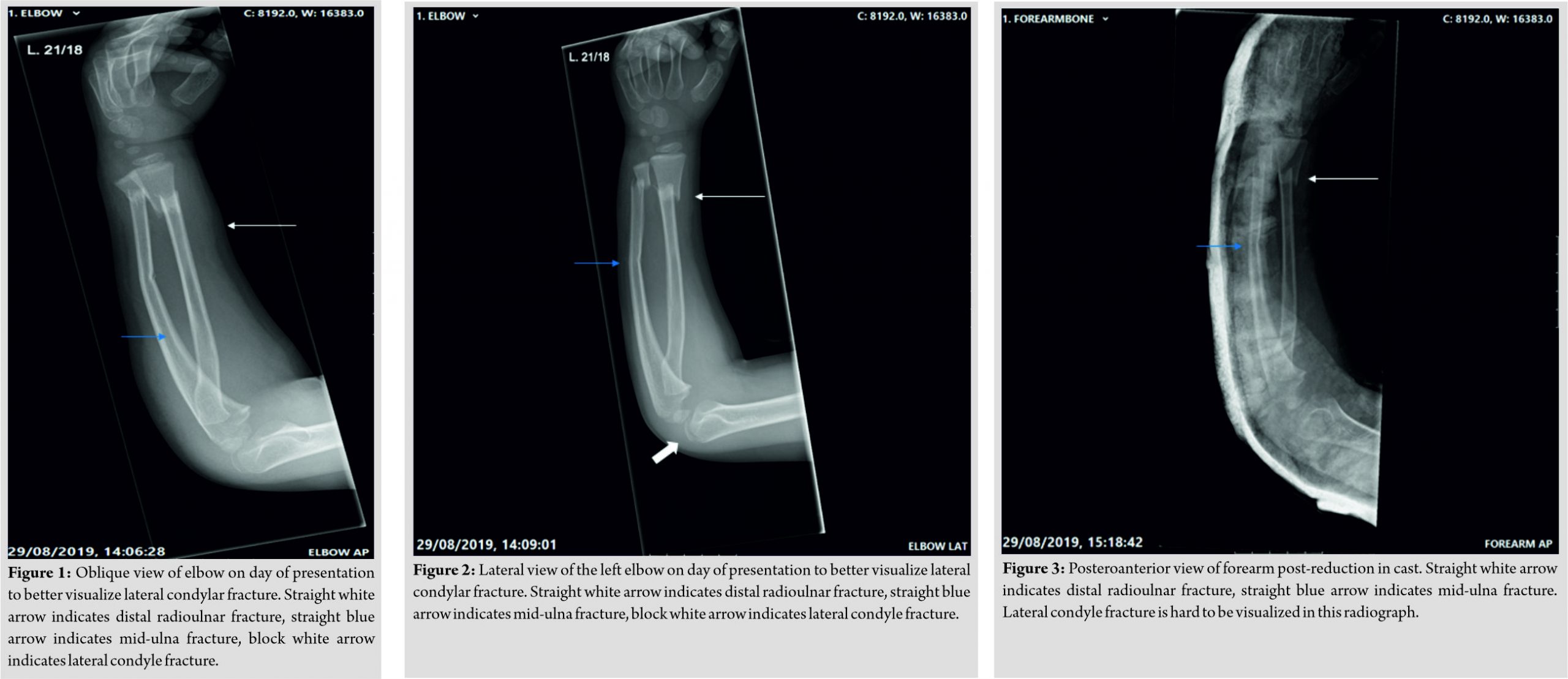
The child remained in an above elbow plaster cast for 4 weeks. On immediate removal of the plaster, elbow range of movement (ROM) was from 40 to 100°. A 80° of pronation was retained, but supination was restricted to 20°. No neurovascular deficit was identified and X-rays demonstrated good fracture union (Fig. 6, 7). At the 8 weeks post-operative follow-up, elbow ROM further improved, with almost full extension, 120° flexion, 70° of pronation and supination passively but achieving 90° actively on pronation and supination. By 12 weeks after surgery, there was a full ROM of the elbow, wrist, and forearm with complete radiological union (Fig. 8, 9). At 13 weeks post-injury, the plate was removed uneventfully and at 2 weeks after the procedure, his wound was well healed, and limb was neurovascularly intact with a full ROM of his elbow, wrist, and forearm at which point he was discharged from our care.
Discussion
To the best of our knowledge, this combination of fractures in the upper limb has not been described in the literature. Multiple studies have been done for both bone fractures in children, describing methods such as hybrid fixation, elastic stable intramedullary nail (ESIN), K-wire fixation, and plate-and-screw constructs [10, 11, 12, 13]. Evidence in literature is conflicting, with studies stating ESIN as a superior fixation method, whereas other studies found no significant difference between ESIN and plating constructs [8, 13, 14, 15, 16]. In our case, there was significant instability demonstrated on initial image intensifier screening perioperatively and the fracture was not amenable to fixation with flexible nails, due to the metaphyseal-diaphyseal junction location of the fracture. In addition, the angulated ulna shaft fracture was able to be completely anatomically reduced; therefore, we did not proceed to performing an ESIN. An ESIN would have allowed for potential quicker recovery time and earlier removal of the plaster, but due to the presence of the ipsilateral lateral condyle fracture, immobilization in an above elbow plaster would still have been required. Even though studies have shown single-bone fixation to be more unstable, we decided to plate only the radius, as the ulna achieved stable reduction after fixation of the distal radius [17, 18]. Evidently, fixation of the radius alone in this case has proven satisfactory, as follow-up demonstrated normal ROMs of all joints in the left arm. This correlates with findings from Yong et al., which showed that single-bone fixation does not compromise on functional outcomes compared to both bone fixations in children [19]. Tan et al. found that lateral condyle fractures should be treated conservatively unless there is a displacement of >2 mm [9]. As such, we opted for conservative treatment. The fracture has healed without any complications as shown in our follow-up X-rays.
Conclusion
This case emphasizes the importance of a secondary survey in the context of even minor trauma to rule out concurrent injuries – in our case, multiple fractures affecting a unilateral upper limb in the pediatric setting. Through this case, we found that minimally displaced lateral condyle fractures can be managed conservatively with good outcome. Single-bone fixation in both bone forearm fractures can lead to very satisfactory outcome, and plate and screw fixation is preferable over ESIN when fractures are within the metaphyseal/diaphyseal junction and unstable.
Clinical Message
The importance of a secondary survey in the context of even minor trauma to rule out concurrent injuries, minimally displaced lateral condyle fractures can be managed conservatively, and single-bone fixation in both bone forearm fractures can lead to good outcome.
References
1. Iyer RS, Thapa MM, Khanna PC, Chew FS. Pediatric bone imaging: Imaging elbow trauma in children-a review of acute and chronic injuries. AJR Am J Roentgenol 2012;198:1053-68.
2. Vopat ML, Kane PM, Christino MA, Truntzer J, McClure P, Katarincic J, et al. Treatment of diaphyseal forearm fractures in children. Orthop Rev (Pavia) 2014;6:5325.
3. Sinikumpu JJ, Lautamo A, Pokka T, Serlo W. The increasing incidence of paediatric diaphyseal both-bone forearm fractures and their internal fixation during the last decade. Injury 2012;43:362-6.
4. Catterall A. Rockwood and Wilkins’ fractures in children. J Bone Joint Surg Br 2002;84:465-6.
5. Kocher MS, Waters PM, Micheli LJ. Upper extremity injuries in the paediatric athlete. Sports Med 2000;30:117-35.
6. Rodríguez-Merchán EC. Pediatric fractures of the forearm. Clin Orthop Relat Res 2005;432:65-72.
7. Shaerf DA, Vanhegan IS, Dattani R. Diagnosis, management and complications of distal humerus lateral condyle fractures in children. Shoulder Elbow 2018;10:114-20.
8. Patel A, Li L, Anand A. Systematic review: Functional outcomes and complications of intramedullary nailing versus plate fixation for both-bone diaphyseal forearm fractures in children. Injury 2014;45:1135-43.
9. Tan SH, Dartnell J, Lim AK, Hui JH. Paediatric lateral condyle fractures: A systematic review. Arch Orthop Trauma Surg 2018;138:809-17.
10. Du Z, Wang H. Commentary on: A novel hybrid fixation versus dual plating for both-bone forearm fractures in older children: A prospective comparative study. Int J Surg 2019;70:105.
11. Kruppa C, Bunge P, Schildhauer TA, Dudda M. Low complication rate of elastic stable intramedullary nailing (ESIN) of pediatric forearm fractures. Medicine (Baltimore) 2017;96:e6669.
12. Şahin N, Akalın Y, Türker O, Özkaya G. ESIN and K-wire fixation have similar results in pediatric both-bone diaphyseal forearm fractures. Ulus Travma Acil Cerrahi Derg 2017;23:415-20.
13. Zhao L, Wang B, Bai X, Liu Z, Gao H, Li Y. Plate fixation versus intramedullary nailing for both-bone forearm fractures: A meta-analysis of randomized controlled trials and cohort studies. World J Surg 2017;41:722-33.
14. Shah AS, Lesniak BP, Wolter TD, Caird MS, Farley FA, Have KL. Stabilization of adolescent both-bone forearm fractures: A comparison of intramedullary nailing versus open reduction and internal fixation. J Orthop Trauma 2010;24:440-7.
15. Baldwin K, Morrison MJ, Tomlinson LA, Ramirez R, Flynn JM. Both bone forearm fractures in children and adolescents, which fixation strategy is superior-plates or nails? A systematic review and meta-analysis of observational studies. J Orthop Trauma 2014;28:e8-14.
16. Westacott DJ, Jordan RW, Cooke SJ. Functional outcome following intramedullary nailing or plate and screw fixation of paediatric diaphyseal forearm fractures: A systematic review. J Child Orthop 2012;6:75-80.
17. Crighton EA, Huntley JS. Single versus double intramedullary fixation of paediatric both bone forearm fractures: Radiological outcomes. Cureus 2018;10:e2544.
18. Colaris J, Reijman M, Allema JH, Kraan G, Van Winterswijk P, De Vries M, et al. Single-bone intramedullary fixation of unstable both-bone diaphyseal forearm fractures in children leads to increased re-displacement: A multicentre randomised controlled trial. Arch Orthop Trauma Surg 2013;133:1079-87.
19. Yong B, Yuan Z, Li J, Li Y, Southern E, Canavese F, et al. Single bone fixation versus both bone fixation for pediatric unstable forearm fractures: A systematic review and meta-analysis. Indian J Orthop 2018;52:529-35.
| How to Cite This Article: Ang WW, Overton A, MA Ahmad. Multiple Unilateral Upper Limb Fractures in the Paediatric Setting – A Case Report. Journal of Orthopaedic Case Reports 2020 September;10(6):64.67. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com