[box type=”bio”] Learning Point of the Article: [/box]
High suspicion of injury and stronger fixation of fracture is needed in patients presenting with shoulder dislocation following seizures to prevent missed diagnoses and failures from pre-existing osteopenia of drug use; a classification is also proposed for these injuries.
Case Report | Volume 10 | Issue 6 | JOCR September 2020 | Page 80-85 | Srinivas B S Kambhampati, Samundeeswari Saseendar, Saseendar Shanmugasundaram. DOI: 10.13107/jocr.2020.v10.i06.1886
Authors: Srinivas B S Kambhampati[1], Samundeeswari Saseendar[2], Saseendar Shanmugasundaram[3]
[1]Department of Orthopaedics, “Sri Dhaatri,” SKDGOC, Vijayawada, Andhra Pradesh, India,
[2]Department of Orthopaedics, CARE Sports Injury, Chennai, India,
[3]Department of Orthopaedics, Apollo Hospital, Muscat, Sultanate of Oman.
Address of Correspondence:
Dr. Saseendar Shanmugasundaram,
Apollo Hospital, Muscat, Sultanate of Oman.
E-mail: ssaseendar@yahoo.co.in
Abstract
Introduction: Bilateral shoulder dislocations are rare and can result from sports injuries, epileptic seizures, electric shock, or electroconvulsive therapy. Divergent shoulder dislocations are even more rare and difficult to treat. We report a case of bilateral divergent shoulder dislocations with bilateral greater tuberosity fractures. We have reviewed the existing literature and have summarized the mechanisms and outcomes of such injuries.
Case Report: A 35-year-old, right-hand dominant male, a known epileptic presented with pain and deformity in both shoulders after an episode of generalized seizures. Radiographs revealed anterior dislocation on the right and posterior dislocation on the left shoulders along with bilateral displaced fractures of the greater tuberosities. The patient was treated with closed reduction of bilateral shoulder dislocations using gentle traction followed by open suture fixation of the greater tuberosity fractures. The greater tuberosity on the posterior dislocation side needed redo fixation with compression screws and sutures for failed fixation. The patient went on to heal well and achieve full function. The case is one of a very rare group of injuries.
Conclusions: Divergent shoulder injuries with greater tuberosity fractures are very rare. They can present a diagnostic and therapeutic challenge. A higher degree of suspicion to diagnose and patient-based approach with strong fixation techniques can lead to good clinical outcomes.
Keywords: Shoulder dislocation, bilateral shoulder dislocation, divergent shoulder dislocation, bilateral greater tuberosity fracture, complex shoulder injury.
Introduction
The shoulder is the most commonly dislocated joint, the most common direction being anterior. Posterior dislocations are less common, representing just 2% of all shoulder dislocations [1]. Bilateral shoulder dislocations are even less common and are considered to result from sports injuries, epileptic seizures, electric shock, or electroconvulsive therapy [2]. We report a case of bilateral divergent shoulder dislocations with bilateral greater tuberosity fractures. Such injuries are rare. The literature has been reviewed and the challenges faced in the treatment of such complex seizure-related injuries are discussed.
Case Report
A 35-year-old, well-built, right-hand dominant gentleman, a temple priest by profession and a known epileptic with a frequency of seizures of once every year, being treated with regular oral phenytoin, presented with pain and deformity in both shoulders since the previous day. He had an episode of generalized seizures the previous day and sustained a fall during the episode. He reported that his left arm got stuck between a wall and a cupboard during the fall while his right arm was free during the fall. However, the patient could not recollect clear details due to seizures. He was otherwise asymptomatic before the incident. There was no history of external injury or other associated injuries or history suggestive of instability.
On examination, both shoulders were swollen with bruising on the medial aspect of both arms. Both shoulders were tender and the arms were held in a neutral position. All attempted movements of the shoulders were painful. There was no distal neurological or vascular deficit in the upper limbs. There was no generalized ligament laxity on clinical examination.
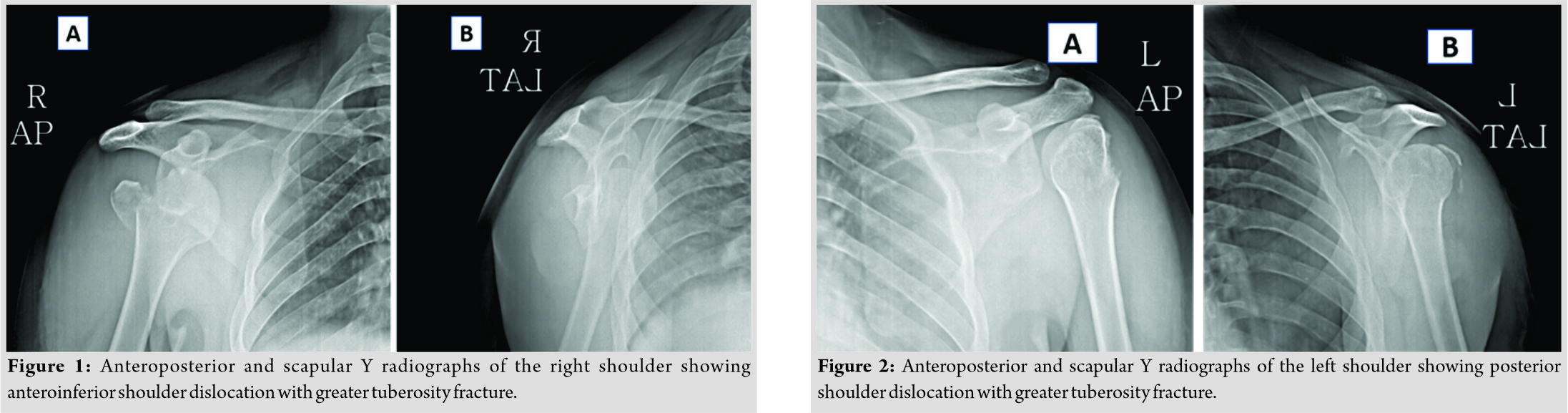
Anteroposterior and scapular Y-view radiographs of the right shoulder (Fig. 1) revealed an anteroinferior dislocation of the shoulder with a displaced fracture of the greater tuberosity and a large Hill–Sachs lesion. Similar views of the left shoulder revealed a light bulb sign (Fig. 2), suggesting posterior dislocation of the shoulder, along with a displaced fracture of the greater tuberosity. Closed reduction of both shoulders was performed with gentle traction under general anesthesia. The greater tuberosities were persistently displaced after the reduction. A lateral transdeltoid approach (deltoid splitting) was used to approach the fracture and transosseous suture fixation of the greater tuberosities with No. 2 Ethibond sutures was done by the technique suggested by Dimakopoulos et al. [3].
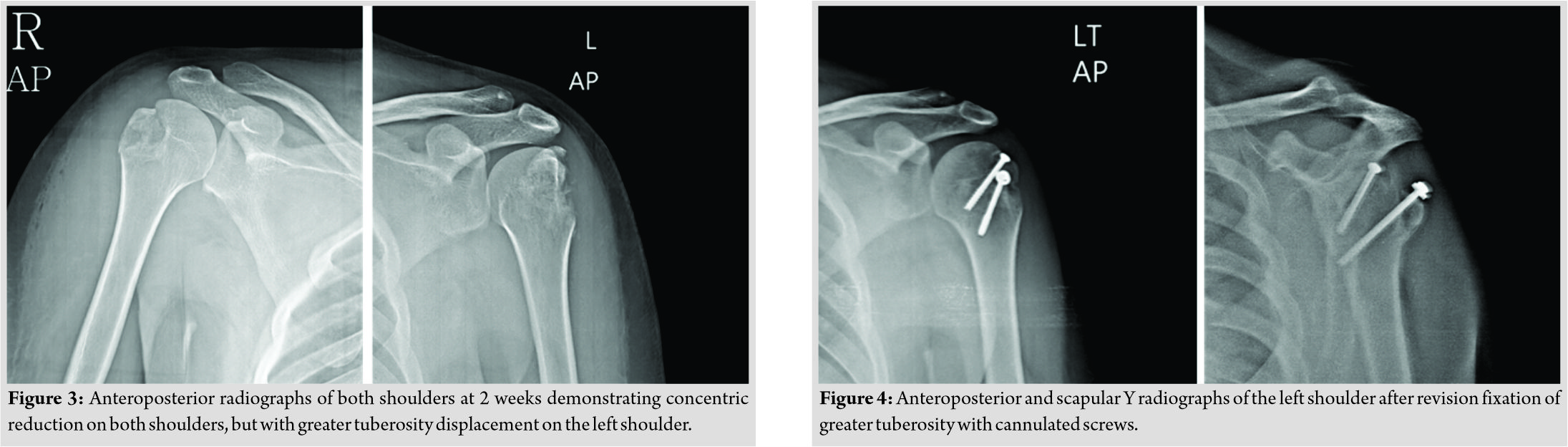
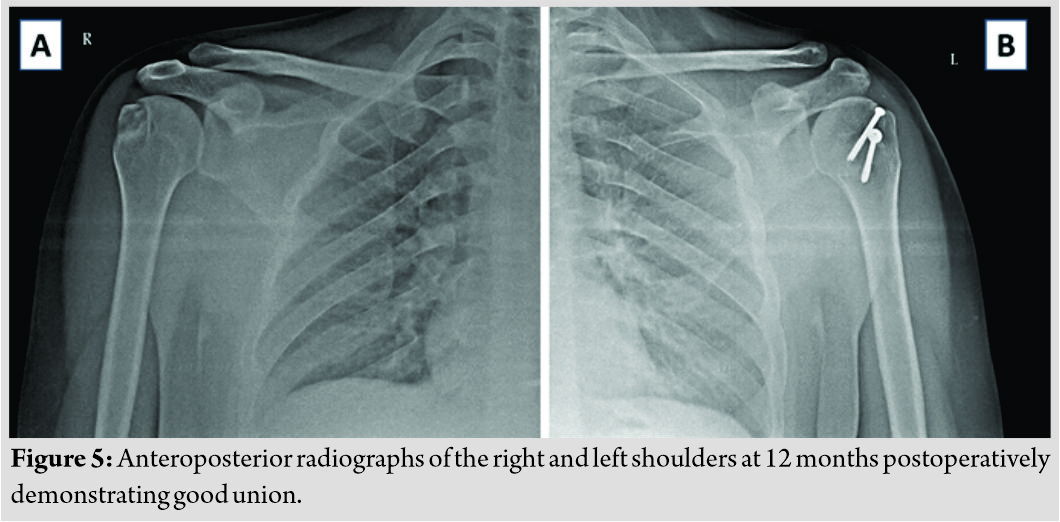
At 2 weeks post-fixation, both shoulders remained congruently reduced. While the right greater tuberosity fracture remained stable, the tuberosity fracture in the left shoulder had displaced (Fig. 3). Resuturing was done under anesthesia and the fixation was reinforced with 4 mm cannulated cancellous screws (Fig. 4). The greater tuberosity fracture had split into two fragments. Fixation was assessed under fluoroscopy and was found to be stable with movements of the shoulder. The patient was advised arm sling for both shoulders for 6 weeks, with an additional small abduction pillow on the left. Internal rotation was delayed for 4 weeks on the left shoulder. Pendulum exercises were started from 2 weeks postoperatively followed by active assisted and active exercises at 4 and 6 weeks, respectively. The patient recovered well. Fractures united at 8 weeks on the right shoulder and at 12 weeks on the left, and at last follow-up at 12 months, the greater tuberosity fractures had healed well and the glenohumeral joints were in situ (Fig. 5). He had achieved full shoulder function by 16 weeks after first surgery (Fig. 6).
Discussion
The shoulder is one of the most unstable joints, accounting for nearly 50% of all dislocations [2]. Of these, 96.5% are anterior, while 3% are posterior [4]. Inferior dislocations and unusual variants of them, though rare, have also been reported [5]. The incidence of bilateral glenohumeral joint dislocation is, however, rare and is mostly considered to be posterior, usually caused by sports injuries, epileptic seizures, electrical shock, or electroconvulsive therapy [2]. Mechanism of shoulder dislocations is unique in seizure disorders. Fracture is an uncommon complication of seizures, the incidence of all fractures being as low as 0.3%, and is extremely rare in the absence of trauma [6]. We would like to classify the mode of injury in bilateral shoulder dislocations into two: “simultaneous” and “sequential.” “Simultaneous” injury is when the index cause (e.g., epileptic convulsions and electrocution) results in violent contractions of the anterior or posterior group of muscles, resulting in anterior or posterior shoulder dislocations, respectively. These dislocations are usually symmetrical. However, asymmetric or divergent dislocations do happen in such injuries when one arm is held in adduction and internal rotation, while the other is held in abduction and external rotation at the time of seizure or electrocution [1, 2, 7, 8]. The injury is “sequential” when the index cause (e.g., seizure, syncope, and electric shock) is followed by an external force (e.g., a fall or traction by a bystander to prevent a fall, etc.). The sequential insults result in anterior or posterior dislocations based on the position of the arm and direction of external force [1, 2, 4, 9, 10, 11]. Sequential insults can also be a part of a sports injury or motor vehicle accident when two different external forces act on the two shoulders [12]. The mechanism of posterior dislocation during seizures is considered to be axial loading with the shoulder in adduction, flexion, and internal rotation, as the internal rotators are more powerful than the external rotators [13]. Fractures are thought to occur due to impingement of the humerus on the glenoid, with persistent seizures causing either fracture of the glenoid rim or proximal humerus. In seizure-related, anterior shoulder dislocation, the mechanism is usually a fall with a flail upper limb in abduction, external rotation, and extension when the greater tuberosity impinges on the acromion and levers out the humeral head from the joint [2]. It may also occur due to the contraction of the pectoralis and latissimus against an unyielding arm, as in a patient restrained in a lateral position while having the seizures [13]. Avulsion fractures and bone defects occur due to violent contraction of the attached muscles coupled with impingement or impact with the glenoid or the acromion. Associated metabolic bone disease, for example, due to antiepileptic drugs contributes to loss of tensile strength of bone [13]. The mechanism of greater tuberosity fractures has been reported to be either from impaction or from avulsion [14]. Impaction can occur against the acromion or superior glenoid, whereas avulsion more commonly occurs with anterior glenohumeral dislocation. It has been found that greater tuberosity fractures occur in 15–30% of dislocations [14]. Unsatisfactory results with conservative management have been reported, if the displacement is more than 5 mm in the general population and more than 3 mm in athletes. The injury in the present report most likely fits into a mechanism of “sequential insults” – the patient had an episode of convulsive seizures that caused a posterior dislocation of the left shoulder, whereas a fall on an outstretched and abducted right arm resulted in anterior dislocation of the right shoulder. Impingement of the osteopenic humeral head on the glenoid rim with persistent violent contractions of the shoulder external rotators resulted in bilateral fractures of the greater tuberosities. It is important to seek a clear history of fall in all patients with a history of seizures, to understand the possible injuries and avoid missed diagnoses [2]. Loss of contour of the shoulder is a classical presentation with dislocated shoulders. However, the typical presentation can be masked in the presence of a fracture [4]. Similarly, in our case, due to time lapse and associated fracture and consequent swelling, this finding was not evident. The most common dislocation of the shoulder reported following epileptic seizures is a posterior dislocation. Bilateral posterior dislocation of shoulders during seizures, although rare, has been reported in literature and association with proximal humerus fracture on both sides is even rarer. As on May 19, 2019, a preliminary search in PubMed for the keywords “divergent fracture dislocation of shoulder” resulted in only one article, by Walla et al. [9]. However, a search for the keywords “bilateral shoulder dislocation” resulted in 403 articles. The titles, abstracts, and when needed, the full text of all these articles were screened to categorize the results. Of the 403 articles, 101 were reports of bilateral anterior shoulder dislocations, 89 about bilateral posterior dislocations, 27 about bilateral inferior dislocations, 8 about divergent anterior and posterior dislocations, and one about divergent anterior and inferior dislocations. Of the remaining, 142 article results were not relevant to the search, while 35 articles or their abstracts were not in English or were not accessible. The references of the reports of divergent dislocations were further searched for similar other reports. In all, there were 10 reports of divergent anterior and posterior shoulder dislocations with or without fracture of the proximal humerus. The details of these reports are summarized in Table 1. There was only one report of such dislocation with bilateral greater tuberosity fractures [4]. The number of reports of bilateral anterior shoulder dislocation was clearly more than such reports of posterior dislocations. This is contradictory to existing reports stating that posterior dislocations are more common than anterior, when bilateral. This can be explained by the fact that most literature search by previous reports were found to be non-extensive or non-representative [1, 4, 9, 15]. Anterior dislocation of one shoulder and posterior dislocation of the other shoulder have been called by different names, including asymmetric dislocation [2, 4] and divergent dislocation [9]. Extensive literature search has revealed only one such report of bilateral greater tuberosity fracture in asymmetric shoulder dislocations [4]. Divergent shoulder dislocations have been reported with a varied spectrum of associated injuries – ranging from no fracture to bilateral comminuted proximal humerus fractures (Table 1). The present case differs from the other reports in being associated with bilateral greater tuberosity fractures. Although Sharma et al. [4] reported on such a similar presentation, their case differs in following a syncope and fall without seizures. The patient sustained two different external injuries to both shoulders. The patient was treated conservatively with a good outcome. However, in the present report, the patient had a more complex sequence of injuries – while seizure could have a role in both the shoulder dislocations, the internal rotation attitude of the left arm predisposed to a posterior dislocation on the left and the following fall on an outstretched right arm led to an anterior dislocation on the right. Strong pull of the shoulder muscles in a pre-existing weak bone could have contributed to the greater tuberosity fractures. The higher displacement in the present case warranted surgical fixation in both shoulders. The presence of seizures and bilateral injury also complicated fixation, necessitating a repeat procedure. We are of the opinion that the direction of dislocation during seizures has more to do with the position of the shoulders than the strength of the posterior and anterior muscle groups. Displaced fractures of the proximal humerus have been advocated fixation, especially in a young patient, for better results. Different methods of fixations have been reported in the literature. These include screw fixation, K-wire fixation, and suture fixation. One disadvantage with metal implant technique (screws or K-wires or plate) is the potential to cause symptoms in the future needing removal of the implant. Suture fixation has been described for greater tuberosity fractures and is not associated with this drawback. Suture fixation may also be beneficial in comminuted fractures or small bone fragments where screw fixation would not be possible. Other techniques used for fixing proximal humerus fractures are using stainless steel (SS) wires, tapes, and sutures [16]. SS wires have the drawback of cutting through osteoporotic bone and fatigue failure requiring removal. We preferred suture fixation of the fractures to avoid the need for later implant removal. However, the fixation on the left shoulder failed and needed a redo fixation in the form of cancellous screws. Failure after fracture fixation has been described even after rigid bone fixation with metal implants [8]. The failure can be attributed to a loss of bone strength from the use of antiepileptics, recurrence of seizures, and/or difficulty in compliance due to bilateral shoulder immobilization. Bone loss as a complication of anti-epileptic drug therapy has been well established and early identification is advised to prevent fractures [17, 18]. The bilateral greater tuberosity fractures in our patient possibly resulted from a combination of bone weakness and muscle pull during seizure, as also the splitting of the greater tuberosity into two fragments noticed during revision surgery.
Conclusions
Understanding the mechanism of bilateral shoulder dislocations is important, with particular emphasis on the position of the shoulder during a seizure episode. More solid fixation is advised in patients with a seizure disorder due to preexisting osteopenia and the risk of further seizures. Careful attention has to be paid in the follow-up period to address any redisplacement of fracture fragments.
Clinical Message
Bilateral shoulder fracture dislocations are difficult to treat. Clinical suspicion should be high and the treatment should be tailored according to characteristics of the fracture–dislocation and the patient’s morbidity to avoid failure or need for revision surgery.
References
1. Tsionos I, Karahalios T, Zibis AH, Malizos KN. Combined anterior and posterior shoulder dislocation as a manifestation of a brain tumour. Acta Orthop Belg 2004;70:612-5.
2. Sharma A, Jindal S, Narula MS, Garg S, Sethi A. Bilateral asymmetrical fracture dislocation of shoulder with rare combination of injuries after epileptic seizure: A case report. Malays Orthop J 2017;11:74-6.
3. Dimakopoulos P, Panagopoulos A, Kasimatis G. Transosseous suture fixation of proximal humeral fractures. J Bone Joint Surg Am 2009;91:8-21.
4. Sharma D, Karthikeyan M, Natraj AR, Poduval M, Patro DK. Asymmetrical fracture dislocation of shoulder-a case report and review of literature. J Orthop Case Rep 2013;3:19-22.
5. Saseendar S, Agarwal DK, Patro DK, Menon J. Unusual inferior dislocation of shoulder: reduction by two-step maneuver: a case report. J Orthop Surg Res 2009;3(4):40.
6. Finelli PF, Cardi JK. Seizure as a cause of fracture. Neurology 1989;39:858-60.
7. Ozer H, Baltaci G, Selek H, Turanli S. Opposite-direction bilateral fracture dislocation of the shoulders after an electric shock. Arch Orthop Trauma Surg 2005;125:499-502.
8. Aufderheide TP, Frascone RJ, Cicero JJ. Simultaneous bilateral anterior and posterior shoulder dislocations. Am J Emerg Med 1985;3:331-3.
9. Walla A, Gnandi-Piou F, Egbohou P, Assogba K, Quacoe M. Bilateral divergent shoulder’s fracture dislocation case in an ischemic stroke patient. J Orthop Case Rep 2017;7:13-6.
10. Cyffka R, Jackisch T, Lein T, Bonnaire F. Simultaneous bilateral ventral and dorsal shoulder dislocation following an epileptic convulsion–a rare combination of injuries. Unfallchirurg 2005;108:327-31.
11. Galois L, Traversari R, Girard D, Mainard D, Delagoutte JP. Asymmetrical bilateral shoulder dislocation. SICOT Online Rep 2003;E024:1-5.
12. Hendriks MM, Frölke JP. Diagnostic image (230). A man with bilateral shoulder dislocation. Ned Tijdschr Geneeskd 2005;149:528.
13. Goudie EB, Murray IR, Robinson CM. Instability of the shoulder following seizures. J Bone Joint Surg Br 2012;94:721-8.
14. Green A, Izzi J. Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elb Surg 2003;12:641-9.
15. Nema S, Pai D, Sinha N, Gupta KK. A unique case of non-traumatic asymmetric shoulder dislocation with four-part fractures of proximal humeri following seizures. J Emerg Trauma Shock 2013;6:231.
16. Hawkins RJ, Bell RH, Gurr K. The three-part fracture of the proximal part of the humerus. Operative treatment. J Bone Joint Surg Am 1986;68:1410-4.
17. Meier C, Kraenzlin ME. Antiepileptics and bone health. Ther Adv Musculoskelet Dis 2011;3:235-43.
18. Pack AM. The association between antiepileptic drugs and bone disease. Epilepsy Curr 2003;3:91-5.
 |
 |
 |
| Dr. Srinivas B S Kambhampati | Dr. Samundeeswari Saseendar | Dr. Saseendar Shanmugasundaram |
| How to Cite This Article: Kambhampati SBS, Samundeeswari S, Saseendar S. Divergent Fracture–dislocation of Shoulders – A Therapeutic Challenge. Journal of Orthopaedic Case Reports 2020 September;10(6): 80-85. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com