[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Injury to both the MCL and proximal tibiofibular joint is rare and requires a heightened suspicion to make the diagnosis, but following the technique outlined in this report can allow for successful concomitant surgical management of this injury pattern.
Case Report | Volume 10 | Issue 9 | JOCR December 2020 | Page 23-27 | Andrew Gudeman, Patrick Siparsky. DOI: 10.13107/jocr.2020.v10.i09.1890
Authors: Andrew Gudeman[1], Patrick Siparsky[1]
[1]Department of Orthopaedic Surgery, Indiana University School of Medicine, Indianapolis, Indiana, United States.
Address of Correspondence:
Dr. Patrick Siparsky,
Department of Orthopaedic Surgery, Indiana University School of Medicine, Indianapolis – 46202, Indiana, United States.
E-mail: psiparsky@iuhealth.org
Abstract
Introduction: Proximal tibiofibular instability is a relatively rare cause of lateral-sided knee pain, and it can be difficult to diagnose. However, medial collateral ligament (MCL) tears are much more common and are much easier to diagnose. Concomitant management of these injuries, however, is uncommon and not well described.
Case Report: We present the case of a 26-year-old female who was struck on the lateral side of the knee by a motor vehicle. She suffered a Grade III MCL tear involving both the superficial and deep bands of the ligament, as well as proximal tibiofibular instability. She failed a course of non-operative management with bracing, and the decision was made to proceed with surgery. The procedure entailed peroneal nerve neurolysis, proximal tibiofibular joint stabilization with Tight Rope™ construct, deep MCL repair, and the superficial MCL reconstruction.
Conclusion: A heightened suspicion for proximal tibiofibular instability must be had in patients with trauma to the knee and lateral-sided pain. In this case, concurrent MCL reconstruction and proximal tibiofibular joint stabilization were necessary to return the knee to normal kinematics.
Keywords: Proximal tibiofibular instability, medial collateral ligament tear, knee.
Introduction
Proximal tibiofibular joint (PTFJ) instability is a rare injury that requires a high index of suspicion for diagnosis with lateral-sided knee pain [1]. These injuries often occur in patients with high-energy mechanisms and can been seen with a concomitant tibial shaft fracture [2, 3, 4] However, cases of isolated proximal tibiofibular dislocations have also been described [5]. Patients often present with lateral-sided knee pain, similar to numerous other pathologies of the knee, making the diagnosis difficult and frequently missed. Both operative and non-operative management with immobilization have been described [3]. Historically, fusion and screw fixation methods were used; however, the PTFJ plays a role in internal and external rotation of the leg, making these stiffer construct less desirable [6]. More recent advancements in the surgical treatment of these injuries include either an anatomic graft reconstruction or suspensory button fixation [5, 7, 8]. Medial collateral ligament (MCL) injuries, on the other hand, are one of the most common injuries in the knee. The superficial MCL provides resistance to valgus stress beyond 30° of flexion, while the deep MCL provides stability in full extension. When found in isolation, Grade I and II MCL injuries are usually treated non-operatively [9, 10]. Rarely, these injuries require surgery in the setting of Grade III damage with persistent valgus laxity in full extension or in combination with other ligamentous injury, or if the distal MCL is torn and retracts over the pes anserine (often termed the “Stener lesion” of the knee) [9]. When surgery is indicated, chronicity and extent of the injury determine whether the MCL is repaired primarily or whether it is reconstructed. Conventionally, acute injuries repaired with 7–10 days of the injury are amenable to primary repair, while others are reconstructed, though treatments do vary [11]. We present a case of a patient who sustained significant trauma to the MCL and injury of the PTFJ. We discuss the clinical presentation, imaging, and unique surgical considerations when addressing these injuries concomitantly. To the best of our knowledge, there have been no described cases in which there were both a Grade III MCL tear and proximal tibiofibular injury requiring surgical intervention.
Case Report
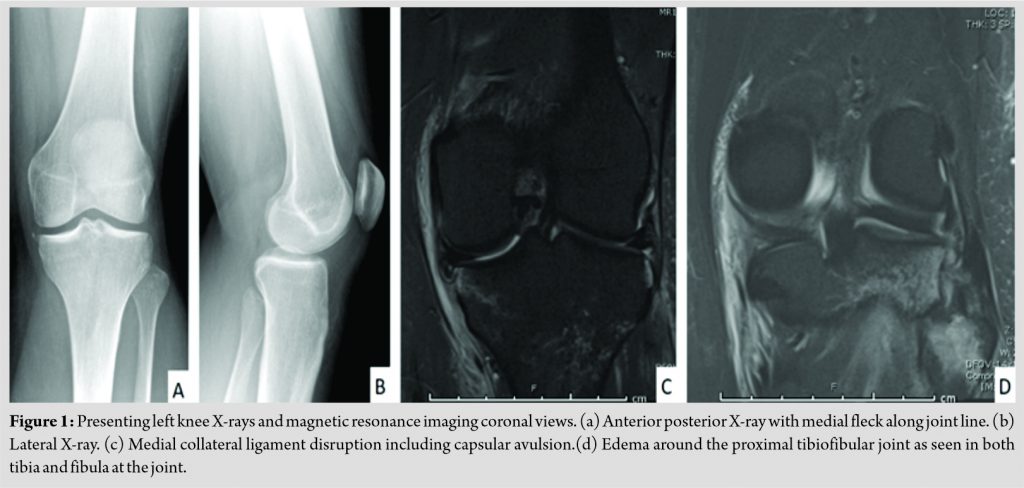
This case presents a 26-year-old female who was struck on the lateral aspect of her knee by a car. She presented to the emergency department where X-rays revealed a small fleck avulsion along the medial joint line. This was a capsular avulsion involving the tissue of the deep MCL (Fig. 1a and b). A magnetic resonance imaging (MRI) was obtained which showed a complete tear of the deep and superficial MCL with no other significant ligamentous injury, as well as edema along the PTFJ (Fig. 1c and d). There was no evidence of meniscal or chondral injury. She was discharged 1 day after the accident with a hinged knee brace locked in extension, with the plan to follow up in the sports medicine clinic.
She presented to clinic approximately 1 week later. At that time, she was found to have decreased sensation on the dorsum of her foot, increased PTFJ motion compared to the contralateral leg, and increased valgus laxity at both 0° and 30° of flexion. With regard to her decreased sensory in the dorsum of the foot, it was significantly worsened with movement of the PTFJ. An additional 3-week trial of non-operative management with bracing was attempted, while she continued to work on non-weight-bearing range of motion and quadriceps reactivation. She returned to clinic at 1 month post-injury with full range of motion, but continued symptoms of opening with valgus load in 0° and 30° of knee flexion, as well as continued dynamically worsening peroneal nerve symptoms with PTFJ movement. The decision was made to proceed with surgery.
Surgical technique
Six weeks after her injury, surgery was performed. Physical examination was repeated under anesthesia and she was found to be ligamentously stable besides significant laxity found with valgus stress in both 30° of flexion and full extension (Fig. 2).
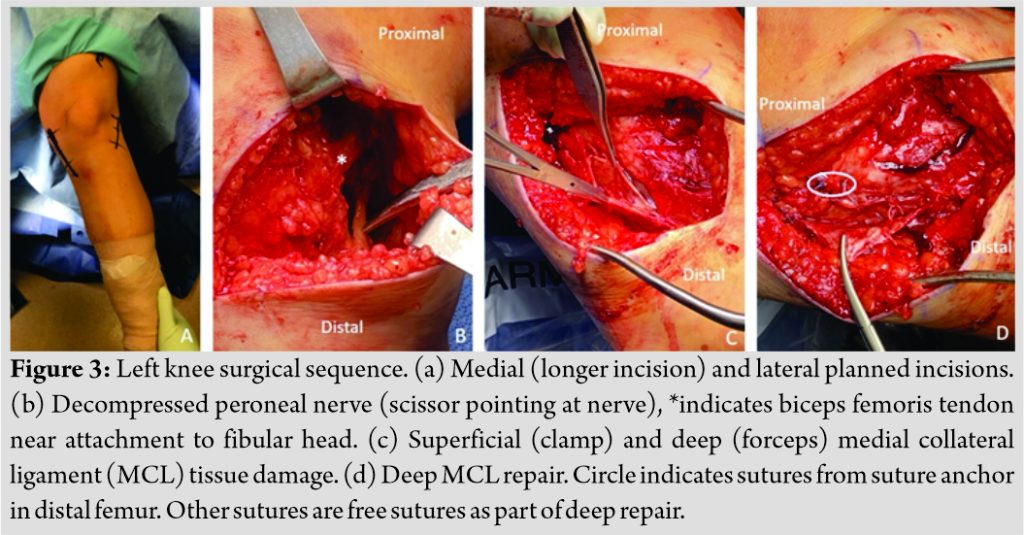
A hockey stick incision (Fig. 3a) was made laterally, and dissection was taken down to the posterior aspects of the biceps femoris just proximal to the attachment to the fibular head. The peroneal nerve was identified, and neurolysis was performed proximally and distally until the nerve was completely free of soft tissue and scar tissue compression (Fig. 3b). The PTFJ was very mobile to movement in open evaluation.
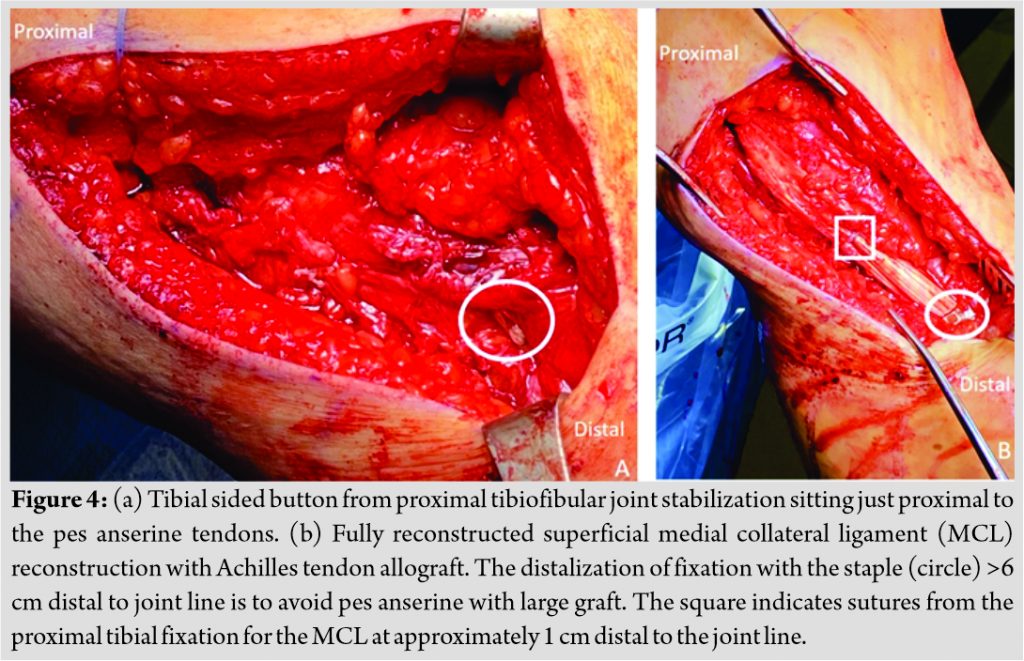
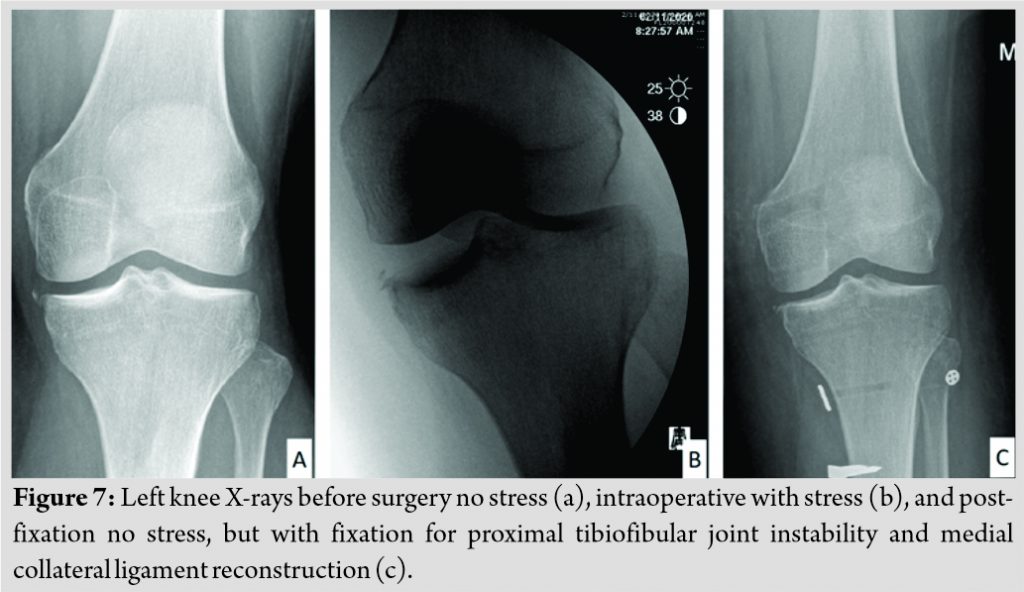
Next, the medial side of the knee was approached through an incision from the medial epicondyle to the pes anserine insertion. The damaged superficial and deep MCL were identified (Fig. 3c). The deep MCL was repaired with the knee in full extension and with varus force using a suture anchor attached to the distal femur, as well as with free sutures the length of the deep MCL tissue (Fig. 3d). Before reconstruction of the superficial MCL, attention was brought back to PTFJ Tight Rope™ (Arthrex, Naples, FL) placement. Under the guide of fluoroscopy, a drill tunnel was placed through the PTFJ from laterally to medially, with posterior to anterior directionality. The Tight Rope™ was placed and locked medially (Fig. 4a). The sutures were tightened until physiologic motion of the PTFJ was achieved.
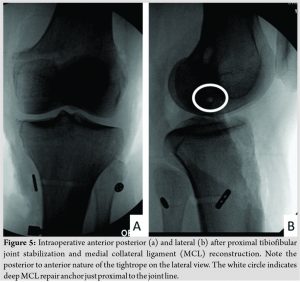
An Achilles tendon allograft was then utilized for the superficial MCL reconstruction. The graft was pulled through a drill hole in the distal femur that was just proximal and posterior to the medial epicondyle and locked in place with an interference screw. The graft was secured in the proximal tibia 1 cm distal to the joint line with a suture anchor, as well as distally with a tibial staple. This was done with the knee in 30° of flexion with a varus force. In this particular case, the tibial staple was placed more distal than the usual 6 cm from the joint line secondary to the PTFJ button being right around 6 cm distal to the joint line based on fibular anatomy (Fig. 4b). Additional free sutures were used to bring some of the more posterior tissue including any remnant of the posterior oblique ligament up to the MCL reconstruction tissue. The knee was felt to be stable to valgus loads at this point. (Fig. 5) shows the intraoperative radiographs for the PTFJ stabilization and the MCL repair/reconstruction.
Follow-up
Postoperatively, the patient remained non-weight-bearing for the first 2 weeks with the leg locked in full extension. The subsequent 2 weeks, she was weight-bearing as tolerated with the leg still locked in extension with crutches. On post-operative day 4, she began working with physical therapy, with a focus on knee range of motion exercises and quadriceps and hip abductor strengthening, initially with body weight and gradually increasing weight as tolerated.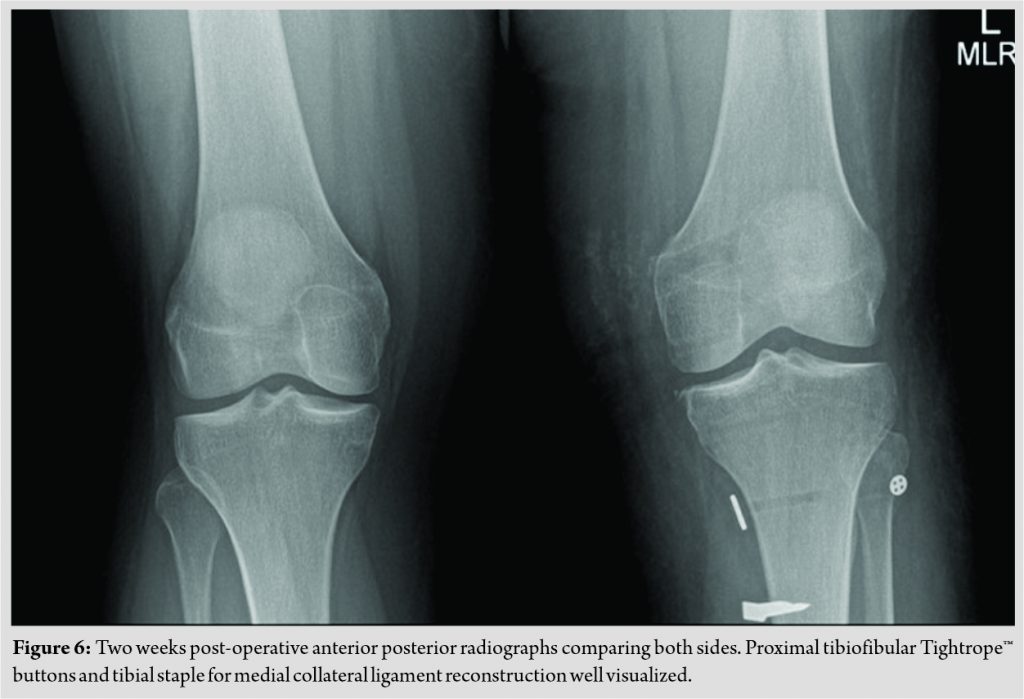
At 6 weeks postoperatively, she was taken out of her hinged knee brace and transitioned to a hinged knee sleeve to provide additional support to the MCL reconstruction. She initiated exercise biking and discontinued crutches.
Discussion
The management of PTFJ instability can be difficult because of the rarity of the injury and the difficulty diagnosing it with an estimated misdiagnosis rate of up to 33% [6]. It commonly presents with lateral-sided knee pain and instability of the joint on examination, although the pain can mimic meniscal, chondral, or ligamentous pathology. It is very important to compare with the contralateral side to avoid misdiagnosis. Typically, the increased mobility of this joint when it is unstable is not subtle and is much more than the contralateral (uninjured) side. The diagnosis becomes even more difficult when concomitant injuries to the knee are present, as was the case in this patient with a Grade III MCL tear. Early identification and intervention can help avoid problems such as static and dynamic peroneal nerve symptoms, as well as chronic instability of the PTFJ [12]. Diagnostic testing has limited utility in its diagnosis because the joint can be relocated at the time of MRI, but grossly unstable clinically. Electromyography can play a role if a palsy of the common peroneal nerve is seen, although it was not obtained in our case because her peroneal nerve symptoms were clearly worsened by simply moving the proximal fibula. The use of stiff fixation constructs, such as arthrodesis and screw fixation, can limit rotation proximally and result in ankle pain secondary to the length of the syndesmosis [6]. The use of a screw for fixation may also necessitate hardware removal. Horst and Laprade [13] discussed anatomic reconstruction of the PTFJ with graft tendon through bone tunnels with acceptable results. Other studies have reported use of a Tight Rope™ or suspension button construct, similar to those that have been popularized for distal tibiofibular syndesmosis [7, 14]. Results of these techniques have been isolated to case reports and small case series but all have shown promising results. To the best of our knowledge, no comparative studies have been performed to show clinical superiority of one method over the others. Management of MCL tears is both common and well documented [9, 10]. The mainstay of treatment for MCL tears is non-surgical treatment and is successful a majority of the time. This includes progressive range of motion and strengthening exercises, with or without a brace depending on the grade of the injury [11]. Surgical indications include valgus instability in full extension, as well as complex multiligamentous knee injuries. Primary repair can be attempted in acute injuries, while reconstruction is typically the best option for more chronic injury or injury patterns without adequate tissue for primary repair [11]. Outcomes following isolated MCL repair or reconstruction are sparse, as they are typically performed concomitantly with other ligamentous reconstruction. However, Varelas et al. performed a systematic review that showed improved patient outcomes after isolated MCL reconstruction and no difference in outcomes comparing isolated MCL reconstruction to MCL reconstruction in conjunction with other surgeries about the knee [15]. Given that surgery for either proximal tibiofibular instability or MCL tear is relatively rare in its own regards, treating them concomitantly has not been described to our knowledge. Concomitant management poses several challenges. Pearls for this procedure can be found in (Table 1). PTFJ instability should be considered for any lateral-sided knee pain after trauma, and suspicion should be high even if there are no findings on X-ray or MRI.
Conclusion
Operative intervention for PTFJ instability and MCL tears is rare in isolation and concomitant surgery to address these has not been described. Having a heightened suspicion for PTFJ instability with lateral knee pain after trauma can help make the diagnosis. When performing these procedures concomitantly, we present several pearls and pitfalls (Table 1) to maximize success.
Clinical Message
Our clinical message is that PTFJ instability can be a difficult diagnosis to make. It should be particularly suspected when a patient has lateral-sided knee pain after trauma with negative imaging and possible peroneal palsy. When operating on the PTFJ and MCL concomitantly, this technique can help avoid common pitfalls and maximize chances of success.
References
1. Aladin A, Lam KS, Szypryt EP. The importance of early diagnosis in the management of proximal tibiofibular dislocation: A 9-and 5-year follow-up of a bilateral case. Knee 2002;9:233-6.
2. Herzog GA, Serrano-Riera R, Sagi HC. Traumatic proximal tibiofibular dislocation: A marker of severely traumatized extremities. J Orthop Trauma 2015;29:456-9.
3. Haupt S, Frima H, Sommer C. Proximal tibiofibular joint dislocation associated with tibial shaft fractures-7 cases. Injury 2016;47:950-3.
4. Johnson BA, Amancharla MR, Merk BR. Dislocation of the proximal tibiofibular joint in association with a tibial shaft fracture: Two case reports and a literature review. Am J Orthop (Belle Mead NJ) 2007;36:439-41.
5. O’Reilly OC, Carruthers KH, Siparsky PN. Bilateral, atraumatic proximal tibiofibular joint instability treated with suspensory button fixation. Orthopedics 2017;40:e1107-11.
6. Ogden JA. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res 1974;101:186-91.
7. Okoroha KR, Mahan MC, Matar R, Khalil LS, Brand JP, Guthrie ST. Proximal tibiofibular dislocation repaired with syndesmotic suture buttons: A case report. J Orthop Case Rep 2018;8:82.
8. Warner BT, Moulton SG, Cram TR, LaPrade RF. Anatomic reconstruction of the proximal tibiofibular joint. Arthrosc Tech 2016;5:e207-10.
9. Encinas-Ullán CA, Rodríguez-Merchán EC. Isolated medial collateral ligament tears: An update on management. EFORT Open Rev 2018;3:398-407.
10. Miyamoto RG, Bosco JA, Sherman OH. Treatment of medial collateral ligament injuries. J Am Acad Orthop Surg 2009;17:152-61.
11. Phisitkul P, James SL, Wolf BR, Amendola A. MCL injuries of the knee: Current concepts review. Iowa Orthop J 2006;26:77-90.
12. Sarma A, Borgohain B, Saikia B. Proximal tibiofibular joint: Rendezvous with a forgotten articulation. Indian J Orthop 2015;49:489-95.
13. Horst PK, LaPrade RF. Anatomic reconstruction of chronic symptomatic anterolateral proximal tibiofibular joint instability. Knee Surg Sport Traumatol Arthrosc 2010;18:1452-5.
14. Lenehan B, McCarthy T, Street J, Gilmore M. Dislocation of the proximal tibiofibular joint: A new method of fixation. Injury Extra 2006;37:385-9.
15. Varelas AN, Erickson BJ, Cvetanovich GL, Bach BR Jr. Medial collateral ligament reconstruction in patients with medial knee instability: A systematic review. Orthop J Sports Med 2017;5:2325967117703920.
 |
 |
| Dr. Andrew Gudeman | Dr. Patrick Siparsky |
| How to Cite This Article: Gudeman A, Siparsky P. Surgical Management of Concomitant Proximal Tibiofibular Instability and Medial Collateral Ligament Tear: A Case Report. Journal of Orthopaedic Case Reports 2020 December;10(9): 23-27. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com