[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Paraparesis or paralysis may not be always due to the spinal cause; it can be due to non-spinal medical cause such as hypokalemia, which can be kept in mind while treating such patient.
Case Report | Volume 10 | Issue 9 | JOCR December 2020 | Page 47-51 | Hitesh N Modi, Utsab Shreshtha, Om Lakhani. DOI: 10.13107/jocr.2020.v10.i09.1898
Authors: Hitesh N Modi[1], Utsab Shreshtha[1], Om Lakhani[2]
[1]Department of Spine Surgery, Zydus Hospitals and Healthcare Research Private Limited, Ahmedabad. Gujarat. India.
[2]Department of Endocrinology, Zydus Hospitals and Healthcare Research Private Limited, Ahmedabad. Gujarat. India.
Address of Correspondence:
Dr. Hitesh N Modi,
Department of Spine Surgery, Zydus Hospitals and Healthcare Research Pvt. Ltd., Ahmedabad – 380 054. Gujarat. India.
E-mail: drmodihitesh@gmail.com
Abstract
Introduction: This study aims to present a case of spinal intradural tumor with paraparesis referred for surgery, which later progressed to quadriparesis and subsequently found to have hypokalemia due to primary hyperaldosteronism causing a clinical dilemma.
Case Report: A 46-year-old male was referred for surgery from peripheral center with a diagnosis of an intradural tumor at L1. The patient presented to us with paraparesis, which progressed to quadriparesis. On evaluation, the patient was found to have low serum potassium levels of 1.6 mmol/L with hypertension. The plasma aldosterone-renin was elevated which was suggestive of primary hyperaldosteronism. Further, investigations in the form of CT abdomen suggested the presence of a right adrenal adenoma. The patient was diagnosed with hypokalemia-induced quadriparesis and treated conservatively with potassium supplementation and later spironolactone. The patient recovered completely in 72 h and was able to walk independently before discharge.
Conclusion: Spinal tumor may not always be the cause for patient’s paraparesis; non-spinal factors such as hypokalemia should be kept in mind. The presence of intradural spinal tumor with hypokalemia may cause decision dilemma regarding treatment and interdisciplinary approach is recommended to facilitate the treatment.
Keyword: Intradural spine tumor, paraparesis or quadriparesis, hypokalemia, primary hyperaldosteronism/Conn’s syndrome, management dilemma.
Introduction
Weakness in extremities is often a presenting symptom in cases of spinal intradural or extradural tumors [1]. However, it may not be always seen that patients who have intradural tumors often present with neurological complication [2]. Usually, it requires surgical excision if it involves neurology. Severe hypokalemia can sometimes present as muscular weakness mimicking neurological deficit [3]. Hypokalemic paralysis in extremities is also relatively rare but potentially life-threatening clinical condition [4]. If recognized and treated appropriately, patients recover without any clinical sequel [5]. Morbidity and mortality associated with unrecognized disease include respiratory failure leading to death. Hence, it is imperative for physicians to be knowledgeable about the causes of hypokalemic paralysis and consider them diagnostically.
Can intradural tumor present with weakness in extremities and simultaneously having hypokalemic paraparesis that presents with similar kind of symptoms that often mislead to the treatment of intradural tumor? This presentation when coexisted in patient of spinal cord pathology always leads to diagnostic dilemma [6]. There is no case report present in the literature having such condition present simultaneously that might mislead to decision dilemma for the treatment. We present a case of a 46-year-old male who was diagnosed as having an intradural extramedullary tumor on magnetic resonance imaging (MRI) having paraparesis and referred for surgery. He was later found to have concomitant potassium deficiency due to progression of weakness proximally. The potassium deficit was due to primary hyperaldosteronism (Conn’s syndrome) [7].
Case Report
A 46-year-old male was referred for surgery from the peripheral center with diagnosis of spine tumor. The patient presented with complaint of sudden onset of asymmetrical weakness on both lower extremities over a period of 3 days. He has associated mild back pain around dorsolumbar region for more than 3 months duration. There was no history of trauma or any injury over the back. Treatment in the previous facility was mainly in the form of diagnostic in the form of MRI and symptomatic in the form of oral gabapentin and nonsteroidal anti-inflammatory medications. He had history of hypertension for 2 years and was on antihypertensive medications in the form of combination of losartan and hydrochlorothiazide. There was no family history with similar weakness. There was no significant history with similar illness. Physical examination revealed heart rate of 102 beats/min, blood pressure of 150/102 mmHg, oxygen saturation (SpO2) of 96%, temperature of 98 degree F, and respiratory rate of 26/min. There were no pallor, icterus, lymphadenopathy, cyanosis, clubbing, edema, and dehydration noted. No jugular venous distension or swelling around neck (goiter) was appreciated. Cardiac examination revealed regular rhythm with normal heart sounds. Respiratory examination revealed tachypnea with decreased breath sounds in bilateral basal areas. Abdominal examination was normal. On neurological examination, cranial nerve functions were grossly intact, however, power in all muscle groups in the right lower extremity was 2/5 and in left lower extremity was 3/5. The sensations of all four limbs were normal; however, the deep tendon reflexes were absent with bilateral flexor plantar response. There was no tenderness or swelling over back noticed. The patient did not have any problem with bowel and bladder movement.
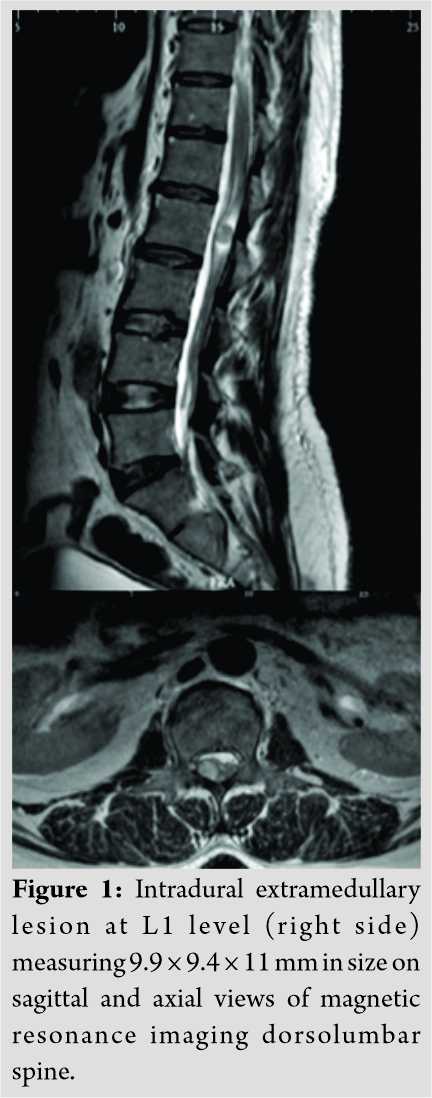
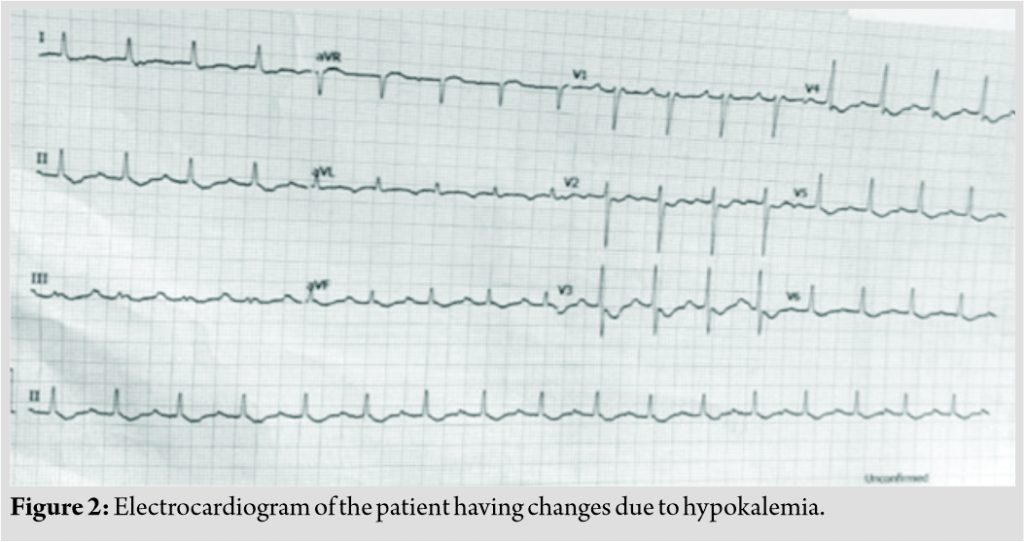
MRI of dorsolumbar spine showed evidence of intradural extramedullary lesion at L1 level (right-sided prominent) measuring 9.9 × 9.4 × 11 mm in size (Fig. 1). MRI of brain with cervical screening was normal. Primary blood investigations including complete blood count and random blood sugar were within normal range. Considering his neurological deterioration and MRI imaging, he was primarily admitted in ward for further work-up with possibility of surgical option. In intensive care unit (ICU), further hematological work-up suggested normal renal, liver, and thyroid functions. However, his serum potassium level (K+) was significantly low with the value of 1.6 mmol/L (normal: 3.5–4.5). His serum sodium, ionized calcium, and magnesium level were 146 mmol/L (normal: 135–145), 3.79 mg/dl (normal: 4.49–5.29), and 2.86 mg/dl (normal: 1.6–2.3), respectively. Twelve standard leads electrocardiogram revealed changes of severe hypokalemia such as flattening of T wave, ST segment depression, prolongation of PR interval (228 ms), prolonged QT corrected interval (593 ms), and presence of U waves (Fig. 2). ABG (arterial blood gas) analysis showed mixed respiratory alkalosis with K+ of <1.5 mmol/L. The patient also started developing mild weakness in his both upper extremities within next 8 h, and power in his both upper extremities was around 4/5 while power in both lower extremities was further deteriorated to 1/5. Reflexes in all extremities were sluggish with preserved sensations.
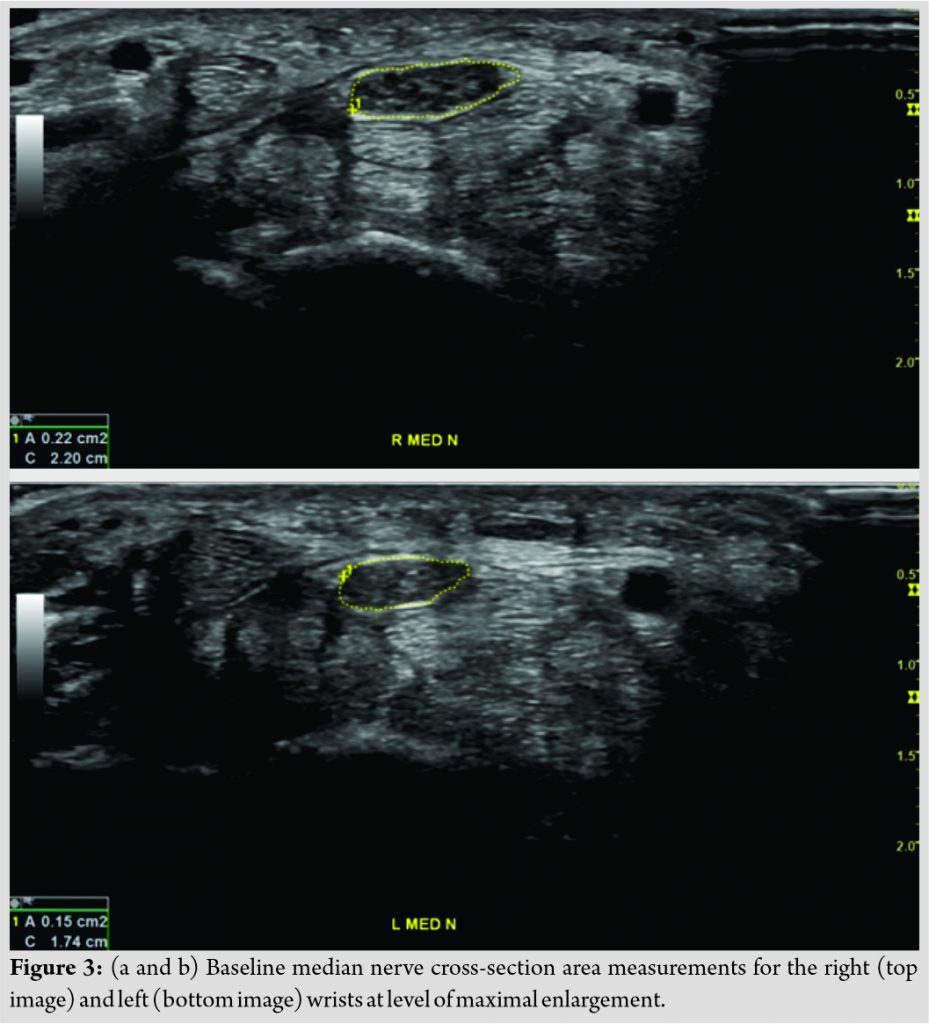
Endocrinologist and cardiologist were consulted immediately. The patient was shifted to ICU and simultaneously treated with intravenous potassium, calcium, and other supportive measurements. Consecutively, appropriate tests were requested. Since the patient had hypokalemia, metabolic alkalosis with hypertension, primary hyperaldosteronism was primarily suspected. The plasma aldosterone-renin ratio was ordered after correction of the potassium levels and keeping all the pre-test conditions in mind. The plasma aldosterone-renin ratio was significantly elevated. A saline loading test was performed which showed failure of adequate suppression of aldosterone, confirming the diagnosis of primary hyperaldosteronism (Conn’s syndrome). Other laboratory investigations such as transtubular potassium gradient (TTKG), Vitamin D3, and parathyroid hormone serum cortisol were 5.55 (normal <3), 44.05 (normal: 13.1–35), 14 ng/ml (normal: 30–100), 74.5 pg/ml (normal: 7.5–53.5), and 3.77 mcg/dl (afternoon level: 3–10), respectively. The thyroid function test was normal. Creatine phosphokinase (CPK) was 5391 U/L (normal: 55–170) increasing up to 21,000 U/L, which returned to normal level with adequate hydration. Nerve conduction velocity was normal. Ultrasound of whole abdomen was not significant. Contrast-enhanced computed tomography (CECT) of whole abdomen showed a well-defined peripherally enhancing nodular lesion suggestive of a right adrenal adenoma. There was also hyperplasia of the left adrenal gland (Fig. 3).
Therefore, the diagnosis was kept as primary hyperaldosteronism primarily in a case of spinal intradural tumor. The patient was treated conservatively in spite of intradural tumor, which was decided to observe closely for further decision later on. On the 2nd day of admission, potassium level was increased up to 1.9–3.2 mmol/L, which again increased to 2.4–3 mmol/L and 4.3 mmol/L on the 3rd and 4th day, respectively. Meanwhile, the patient’s power in both upper extremities became 5/5 and in both lower extremities became 4/5. Therefore, potassium infusion was stopped and oral spironolactone was added [7]. The patient was able walk after 72 h with assistance and after 96 h independently. He was discharged after 5 days along with antihypertensive and potassium sparing diuretic (spironolactone).
The patient is maintained on regular visit with endocrinology and spine department till his last follow-up at 6 months. Since the patient had a right adenoma and a hyperplasia of the left adrenal gland, the patient would require adrenal venous sampling if surgical management for primary hyperaldosteronism is to be considered. However, the patient had normal blood pressure and normal potassium levels with adequate dose of spironolactone and adrenal venous sampling followed by surgical resection was deferred. There is no recurrence of such symptoms and intradural tumor remains of same size without further sequel.
Discussion
Acute onset of non-traumatic paraparesis or quadriparesis can be caused by vascular as well as inflammatory disorders of spinal cord (transverse myelitis), non-inflammatory spinal space occupying lesions (spine tumors), and non-spinal disorders. Hypo- or hyperkalemia is one of the causes of non-spinal disorders causing acute onset weakness in extremities [3]. Search for causative factor for paraparesis is obvious when intradural tumor is seen on MRI; however, it can be confusing in the presence of other coexisting diseases [6]. In addition, progressive neurological deficit from paraparesis to quadriparesis raises alarm in surgeon’s mind dealing with intradural pathology at dorsolumbar spine [8-10]. The patient of intradural tumor often presents with various different types of progression of disease, acute, subacute, or chronic. Therefore, the signs also vary, such as, hyperreflexia, hyporeflexia, or areflexia. It often confuses surgeon for management guideline. However, during pre-operative laboratory examinations, hypokalemia was found which was significantly low. Thus, the patient was diagnosed as hypokalemic paraparesis and later quadriparesis. The syndrome of hypokalemic paralysis includes a heterogeneous group of disorders characterized clinically by hypokalemia and acute systemic weakness. Most cases are due to familial or primary hypokalemic periodic paralysis; sporadic cases are associated with numerous other conditions including barium poisoning, hyperthyroidism, renal disorders, certain endocrinopathies, gastrointestinal potassium losses, Sjogren’s syndrome, and infectious pathologies such as dengue fever and Yersinia enterocolitica infection [4, 11-15]. In our case, the patient presented to us in progressive condition, and therefore, initially, it appears to have paraparesis which confuses physician as symptoms were correlating with the lesion. It is important to consider electrolytes and thyroid function tests before we decide for surgical option in spine case.
Acute onset rapidly progressive paraparesis to quadriparesis with normal sensations, reflexes, and bowel/bladder functions but having hypotonia precludes the obvious diagnosis of spinal tumor at L1 level [16]. Vascular lesions were ruled out by normal ultrasound and CECT abdomen. Neurologic disorders were ruled out clinically and by nerve conduction test. Routine pre-operative investigations revealed significant hypokalemia, and on correction of which the patient improved regaining full muscle strength. Simultaneously, we tried to find the cause of hypokalemia as well. A well-defined peripherally enhancing nodular lesion with absolute percentage washout 81% and relative percentage of washout 87 involving body of the right suprarenal gland suggestive of adrenal adenoma was seen (Fig. 3) [17]. Our patient had significant hypokalemia and mixed alkalosis with high normal sodium that coincides with the features of hyperaldosteronism (hypernatremia, hypokalemia, and metabolic alkalosis) [18], though the TTKG was 5.55 (should be <3 to label hypokalemia). The plasma aldosterone to renin ratio of 44.05 (normal: 13.1–35) suggested the presence of primary hyperaldosteronism [7]. We also noted ongoing rhabdomyolysis in this patient with CPK increasing up to 21,000 U/L, which improved with adequate hydration. This may be attributed due to the failure of synthesis of glycogen and inadequate vasodilation of arterioles and capillaries of exercising muscles in the presence of hypokalemia in an otherwise ambulatory patient before he presented to us [19].
Conclusion
Hypokalemic paraparesis progressing to quadriparesis in a patient of spinal tumor is not reported previously. As paraparesis is usual manifestation of spinal cord tumor, it is obvious for spine surgeon to think of surgical resection of the tumor. It is emphasized that medical causes of such manifestations should not be underestimated. In this case, interdisciplinary approach in coordination with endocrinology, nephrology, and urology department helped us to reach to the correct diagnosis of the quadriparesis. Therefore, spinal tumor may not always be the cause of paraparesis/quadriparesis. Non-spinal disorders should not be overlooked as well before planning for surgical resection of the tumor such as hypokalemia (which is treatable) being prime cause of quadriparesis in our case. We want to emphasize on multidisciplinary approach for such patient and focus on primary cause rather than proceeding straightforward to the surgery.
Clinical Message
Spinal tumor may not always be the cause for a patient’s paraparesis; non-spinal factors such as hypokalemia should be kept in mind. The presence of intradural spinal tumor with hypokalemia may cause a decision dilemma regarding treatment and interdisciplinary approach is recommended to facilitate the treatment.
References
1. Ottenhausen M, Ntoulias G, Bodhinayake I, Ruppert FH, Schreiber S, Förschler A, et al. Intradural spinal tumors in adults-update on management and outcome. Neurosurg Rev 2019;42:371-88.
2. Fachrisal, Setiawan E, Alhuraiby SS. Functional outcome in intradural extramedullary tumor patients: Case series. Ann Med Surg (Lond) 2020;54:71-3.
3. Schwenkreis P, Pennekamp W, Tegenthoff M. Differential diagnosis of acute and subacute non-traumatic paraplegia. Dtsch Arztebl 2006;103:2948-54.
4. Ahlawat SK, Sachdev A. Hypokalaemic paralysis. Postgrad Med J 1999;75:193-7.
5. Haider M, Khan Chachar AZ, Munir A. Thyrotoxic periodic paralysis. J Ayub Med Coll Abbottabad 2019;31:619-21.
6. Mittal MK, Rabinstein AA. Spinal cord meningioma: A treatable cause of paraplegia. J Clin Med Res 2012;4:286-8.
7. Foo R, O’Shaughnessy KM, Brown MJ. Hyperaldosteronism: Recent concepts, diagnosis, and management. Postgrad Med J 2001;77:639-44.
8. Khan FG, Namran S. Coexistence of myasthenia gravis with hypokalemic periodic paralysis: A rare presentation. BMJ Case Rep 2019;12:e231241.
9. Elkins JC. Hypokalemic periodic paralysis secondary to dexamethasone injection. J Emerg Nurs 2019;45:79-81.
10. Aggarwal A, Wadhwa R, Pande A, Sahu M, Kapoor D, Khanna R. Hypokalemic periodic paralysis and spectrum of thyroid disorders: Analysis of 7 cases from Northern India. Indian J Endocrinol Metab 2019;23:168-70.
11. Mishra V, Harbada R, Sharma A, Mishra M. Hypokalemic quadriparesis in dengue. J Fam Med Prim Care 2015;4:278-9.
12. Stedwell RE, Allen KM, Binder LS. Hypokalemic paralyses: A review of the etiologies, pathophysiology, presentation, and therapy. Am J Emerg Med 1992;10:143-8.
13. Phelan DM, Hagley SR, Guerin MD. Is hypokalaemia the cause of paralysis in barium poisoning? Br Med J (Clin Res Ed) 1984;289:882.
14. Soule BR, Simone NL. Hypokalemic periodic paralysis: A case report and review of the literature. Cases J 2008;1:256.
15. Munir I, Mehmood T, Islam K, Soni L, McFarlane SI. Thyrotoxic periodic paralysis with sensory deficits in young African American male: A case report and literature review. Am J Med Case Rep 2019;7:138-42.
16. Sandalcioglu IE, Hunold A, Müller O, Bassiouni H, Stolke D, Asgari S. Spinal meningiomas: Critical review of 131 surgically treated patients. Eur Spine J 2008;17:1035-41.
17. Park JJ, Park BK, Kim CK. Adrenal imaging for adenoma characterization: Imaging features, diagnostic accuracies and differential diagnoses. Br J Radiol 2016;89:20151018.
18. Guyton A, Hall J. Adrenocortical hormones. In: Textbook of Medical Physiology. 11th ed., Ch. 77. Philadelphia, PA: Elsevier Saunders; 2006. p. 948-49.
19. Martínez JJ, Oliveira CL, Meneses AL, Rodríguez SA, Corrales PP, López AH, et al. Rhabdomyolysis due to primary hyperaldosteronism. Endocrinol Nutr 2009;56:431-4.
 |
 |
 |
| Dr. Hitesh N Modi | Dr. Utsab Shreshtha | Dr. Om Lakhani |
| How to Cite This Article: Modi HN, Shreshtha U, Lakhani O. Hypokalemic Paraparesis Progressing to Quadriparesis in a Case of Intradural Spinal Tumor. Journal of Orthopaedic Case Reports 2020 December;10(9): 47-51. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com