[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
This case report emphasizes the importance of TAD, valgus reduction, and positive variance in avoiding implant failures, even with a newer implant like TFNA which was developed to improvise onto the shortcomings of PFNA two nail.
Case Report | Volume 10 | Issue 9 | JOCR December 2020 | Page 61-64 | Sanjay Agarwala, Mayank Vijayvargiya, Tej Shah. DOI: 10.13107/jocr.2020.v10.i09.1904
Authors: Sanjay Agarwala[1], Mayank Vijayvargiya[1], Tej Shah[1]
[1]Department of Orthopedics, PD Hinduja Hospital and Medical Research Centre, Mumbai. Maharashtra. India.
Address of Correspondence:
Dr. Sanjay Agarwala,
Professional Services, P.D. Hinduja National Hospital, Veer Savarkar Marg, Mahim (W), Mumbai – 16. Maharashtra. India.
E-mail: drsa2011@gmail.com
Abstract
Introduction: Trochanteric femoral nail-advanced (TFNA) was introduced in the market with better nail design, better alloy (titanium molybdenum) and both sliding and static locking options of the helical blade. Although, it was devised to overcome the shortcomings of roximal Femoral Nail Anti-rotation (PFNA), it still can have complications, if the principles of fracture management are not met. Here, we report a case of a TFNA implant failure with helical blade cut-out in an elderly osteoporotic patient treated for inter-trochanteric femur fracture. To the best of our knowledge, this is the first report of helical blade cut-out wit TFNA nail in world literature.
Case Report: An 83-year-old female patient was treated with a TFNA nail for inter-trochanteric femur fracture (AO 31A2.1). An acceptable reduction and stable fixation were achieved. The position of the helical blade in the head was in the optimal position with a tip apex distance (TAD) of 29 mm. The patient presented to us 6 weeks later with implant failure with helical blade cut out after a history of fall. Cemented bipolar hemiarthroplasty with calcar reconstruction using a mesh was done. The patient was clinically asymptomatic and was walking full weight-bearing till her last follow-up at 14 months.
Conclusion: We can associate the failure seen in our case with an increased TAD of 29 mm, osteoporotic bone and a neutral to negative variance. Helical blade cut-out was seen as the blade was locked onto the nail with insufficient hold onto the osteoporotic head fragment which collapsed into varus, leading to cut-out. This case report emphasizes the importance of TAD, valgus reduction, and positive variance in avoiding implant failures, even with a newer implant like TFNA which was developed to improvise onto the shortcomings of PFNA nail.
Keywords: Trochanteric femoral nail-advanced, helical blade, cut-out, inter-trochanteric femur fracture.
Introduction
Intramedullary proximal femoral nail (PFN) was developed by AO/ASIF for the treatment of unstable peri-trochanteric femoral fractures. Compared with DHS fixation, intramedullary nail like PFN confers an advantage of early weight-bearing and reduced re-operation rates [1]. However, even PFN has its own share of complications as screw back-out, screw cut-out, hardware prominence, and implant failure [2]. To overcome the complications of PFN, trochanteric femoral nail-advanced (TFNA) was introduced to the global market in 2015. It is made of titanium molybdenum (TiMo) alloy (Ti-15Mo) [3]. The small proximal diameter and the lateral relief cut design of the TFNA Nail were designed to avoid impingement on the lateral cortex while preserving bone in the insertion area, potentially reducing the risk of fracture displacement. Oblique cut on the lateral end of the TFNA Helical Blade and screw was designed to reduce lateral protrusion on the soft tissues when compared with that of a standard cut head element [3]. The TFNA offers both options of blade and screw fixation of the femoral head with sliding and static locking [3]. We report a case of a TFNA implant failure with helical blade cut-out in a patient operated for intertrochanteric femur fracture. To the best of our knowledge, this is the first case report of TFNA implant failure with helical blade cut-out. We have also discussed the probable reasons for its failure and the surgical option taken to manage the case.
Case Report
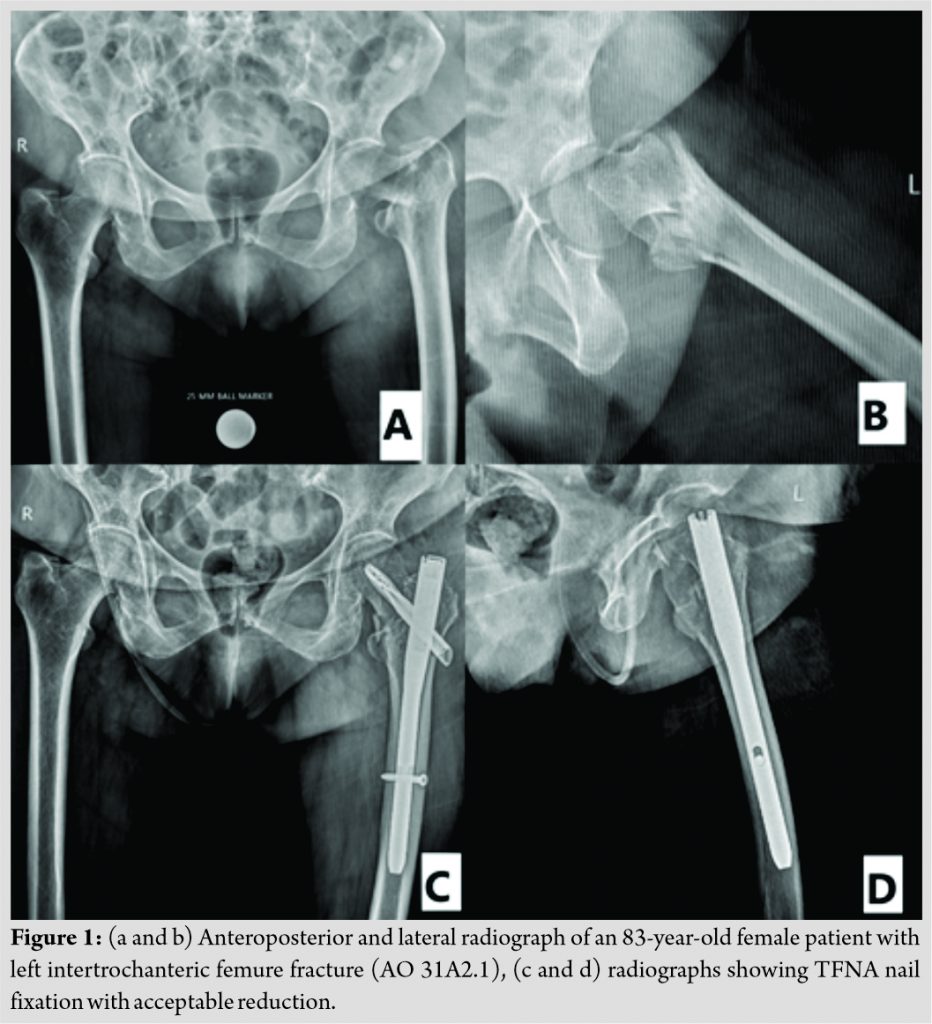
A 83-year-old lady with a BMI of 32 presented to us with a history of fall at home. Radiographs showed left-sided intertrochanteric femur fracture (AO 31A2.1) with marked osteopenia (Singh’s index Grade 3) (Fig. 1). She was operated with TFNA Depuy (Dimension 11 x 200 mm and helical blade of 80 mm). An acceptable reduction of the fracture and stable fixation was achieved intraoperatively (Fig. 1). The position of the helical blade in the head was in the optimal position (center–center) assessed as per Cleveland index (Fig. 2). Tip apex distance (TAD) was found to be 29 mm, assessed in magnification controlled anteroposterior view and lateral view as per the Baumgartner’s method (Fig. 2). Neck-shaft angle measured after fixation was 132.1o and the normal side was 131.4o (Fig. 2). The patient was mobilized partial weight-bearing with the help of walker from the next day of surgery.
She presented to us 6 weeks after the surgery with severe acute onset pain in the left hip, along with inability to bear weight. There was a history of fall at home. Radiographs showed implant failure (cut through of the helical blade) (Fig. 3). Laboratory investigations ruled out infection. The patient was planned for implant removal and bipolar hemiarthroplasty. 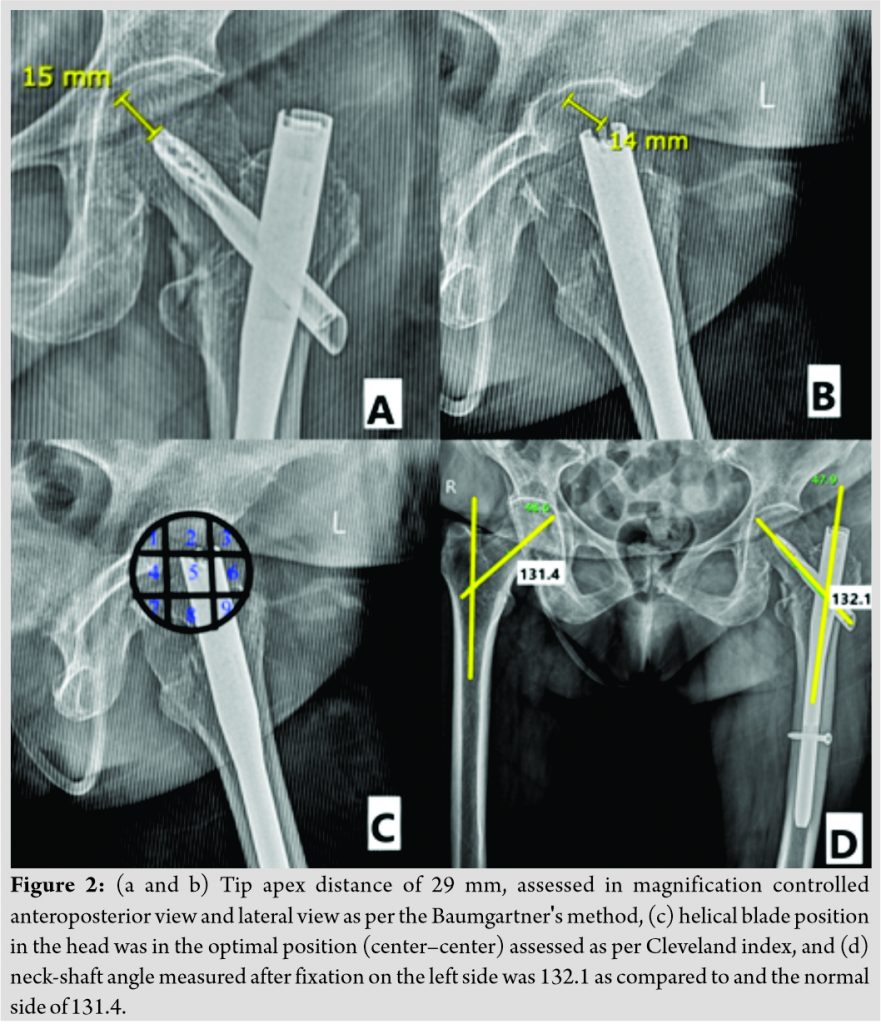
Discussion
Cephalomedullary nails have shown less incidence of implant failure and higher union rate as compared to DHS in unstable IT femur fractures and are the ideal implant of choice in managing such cases [4]. However, they have their own share of complications which include screw cut-out, Z, and reverse-Z effect [5]. TFNA nail was introduced by AO Synthes to overcome the shortcomings of PFNA nail. Here, we are presenting our first case of TFNA implant failure and discussing the possible reasons for its failure. TAD was described by Baumgaertner [6, 7] as a useful intraoperative indicator of deep and central placement of the lag screw in the femoral head, regardless of whether a nail or a plate is chosen to fix the fracture [8]. Nikoloski et al. studied the association of TAD with failure in helical blades and found a bimodal distribution of failure in relation to TAD [9]. Medial migration occurred with TAD <20 mm, whereas cephalad cut-out was seen with TAD >30 mm. They proposed that for helical blades, the optimum TAD is between 20 and 30 mm [9]. TAD, in our case, was 28 mm, although it was lying within the range of optimum value for helical blades in cephalomedulary nails as defined by Nikoloski et al., it was on the higher side. As per the Cleveland index, maintaining an optimal position (center–center, inferior–center) of the screw is necessary for a good outcome. Complications were more when the screw position was in the suboptimal position [10]. In our case, as per Cleveland index, the helical blade was in optimal position. In our case, neck-shaft angle was 132.1 as compared to 131.4 on the normal side. Varus reduction has been shown to be associated with high implant failure rates [11]. Other factors for migration of the implant are an improper entry point, loss of medial support, and a longer superior screw [5]. Fracture reduction with positive medial cortical support allows limited sliding of the head-neck fragment to contact with the femur shaft and thus achieves secondary stability, providing a good mechanical environment for fracture healing [12]. Studies have shown that a positive or neutral variance is associated with good outcomes in intertrochanteric fractures using an intramedullary nail [12]. In our case, the fracture was fixed in neutral or slight negative variance. The other reason of failure of helical blade in this case can be osteoporotic bone. Singh’s index is a reliable method to estimate the degree of osteoporosis [13]. In our case, Singh index of osteoporosis was Grade 3. Biomechanical studies have demonstrated that osteoporotic bones are associated with high chances of implant migration and failure [14]. Lobo-escolar et al. also found Singh’s index to be a significant predictor of cut out [13]. Lamber et al. found that TFNA nail breakage was seen mostly in unstable fracture patterns in their case series [15]. They also hypothesized that the reduced cross-sectional area of the TFNA at the level of the proximal screw aperture, changes in the alloy compared with its predecessors may be of importance in breakage of the TFNA at that site [15]. In our patient, since there was a cut-out of the helical blade from the femoral head, it was not possible to salvage the femoral head; therefore, we opted for bipolar hemiarthroplasty.
Conclusion
We can associate the failure seen in our case with an increased TAD of 29 mm, osteoporotic bone and a neutral to negative variance. Instead of helical blade back-out, we have seen cut-out as the helical blade was locked into the nail. Therefore, failure, in our case, happened with head fragment falling into varus with helical blade cut-out from the femoral head.
Clinical Message
This case report emphasized the importance of TAD, valgus reduction and positive variance in avoiding implant failures, even with a newer implant like TFNA which was developed to improvise onto the shortcomings of PFNA two nail.
References
1. Hoffman MF, Khoriaty JD, Sietsema DL, Jones CB. Outcome of intramedullary nailing treatment for intertrochanteric femoral fractures. J Orthop Surg Res 2019;14:360.
2. Koyuncu S, Altay T, Kayalı C, Ozan F, Yamak K. Mechanical failures after fixation with proximal femoral nail and risk factors. Clin Interv Aging 2015;10:1959-65.
3. DePuy Synthes Companies. TFN-Advanced Proximal Femoral Nailing System: Surgical Technique; 2017. Availabl from: http://www.synthes.vo.llnwd.net/o16/LLNWMB8/US%20Mobile/Synthes%20North%20America/Product%20Support%20Materials/Brochures/3936_DSUSTRM06140109-7_TFNA_Core_rev1.pdf. [Last accessed on 2019 Jan 24].
4. Jonnes C, Sm S, Najimudeen S. Type II intertrochanteric fractures: Proximal Femoral Nailing (PFN) versus Dynamic Hip Screw (DHS). Arch Bone Joint Surg 2016;4:23‐8.
5. Pires RE, Santana EO Jr., Santos LE, Giordano V, Balbachevsky D, Dos Reis FB. Failure of fixation of trochanteric femur fractures: Clinical recommendations for avoiding Z-effect and reverse Z-effect type complications. Patient Saf Surg 2011;5:17.
6. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am 1995;77:1058-64.
7. Baumgaertner MR, Solberg BD. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br 1997;79:969-71.
8. Haidukewych GJ. Intertrochanteric fractures: Ten tips to improve results. J Bone Joint Surg Am 2009;91:712-9.
9. Nikoloski AN, Osbrough AL, Yates PJ. Should the tip-apex distance (TAD) rule be modified for the proximal femoral nail antirotation (PFNA)? A retrospective study. J Orthop Surg Res 2013;8:35.
10. Cleveland M, Bosworth DM, Thompson FR, Wilson HJ Jr., Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am 1959;41-A:1399-408.
11. Hak DJ, Bilat C. Avoiding varus malreduction during cephalomedullary nailing of intertrochanteric hip fractures. Arch Orthop Trauma Surg 2011;131:709-10.
12. Chang SM, Zhang YQ, Ma Z, Li Q, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: A key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg 2015;135:811-8.
13. Pramudito JT, Soegijoko S, Mengko TR, Muchtadi FI, Wachjudi RG. Trabecular pattern analysis of proximal femur radiographs for osteoporosis detection. J Biomed Pharm Eng 2007;1:45-51.
14. Cheema GS, Rastogi A, Singh V, Goel SC. Comparison of cutout resistance of dynamic condylar screw and proximal femoral nail in reverse oblique trochanteric fractures: A biomechanical study. Indian J Orthop 2012;46:259-65.
15. Lambers A, Rieger B, Kop A, D’Alessandro P, Yates P. Implant fracture analysis of the TFNA proximal femoral nail. J Bone Joint Surg Am 2019;101:804‐11.
 |
 |
 |
| Dr. Sanjay Agarwala | Dr. Mayank Vijayvargiya | Dr. Tej Shah |
| How to Cite This Article: Agarwala S, Vijayvargiya M, Shah T. TFNA Implant Failure with Helical Blade Cut-out. Journal of Orthopaedic Case Reports 2020 December;10(9): 61-64. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com