[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Sustained local concentration of anti-microbial substance can potentially mitigate deep infections in open fractures of tibia and a careful selection of appropriate anti-microbial may not endanger bone union.
Case Report | Volume 10 | Issue 9 | JOCR December 2020 | Page 65-70 | S Vignesh, Amresh Ghai. DOI: 10.13107/jocr.2020.v10.i09.1906
Authors: S Vignesh[1], Amresh Ghai[2]
[1]Department of Orthopaedics, Base Hospital Barrackpore, Kolkata. West Bengal – 700 120. India.
[2]Department of Orthopaedics, Base Hospital, Delhi Cantt, New Delhi – 110010. India.
Address of Correspondence:
Dr. Vignesh S,
Department of Orthopaedics, Base Hospital Barrackpore, Kolkata. West Bengal – 700 120. India.
E-mail: viccuindia@gmail.com
Abstract
Introduction: The incidence and outcome of infection in open tibial fractures is adequately recorded in literature. The aim of this study is to find out the deep infection rate, union rate, and functional outcome of open tibial fractures managed by prophylactic antibiotic eluting interlocking nail.
Methodology: A total of 18 patients with 20 open tibial fractures who met the study criteria were included and followed up for a minimum of 1 year after surgical intervention. Reamed intramedullary interlocking nailing with antibiotic eluting nail was done followed by adequate skin cover.
Results: The outcomes were assessed using lower extremity functional scale and radiological union scale in tibial fractures both of which showed maximum improvement in initial 3 months followed by a steady improvement till 1 year with a good degree of correlation between the two scales. The total incidence of deep infection in this study was 5% (n = 1). All cases achieved union and independent ambulation by 1 year.
Conclusion: Our study shows good radiological and functional outcomes with prophylactic antibiotic-coated nailing of open tibial fractures of Grades II and IIIA. The rate of deep infection is 5% and union rate is 100% in our study. Further comparative studies are required for drawing more conclusions on application of the results in clinical practice.
Keywords: Local antibiotic prophylaxis, open tibia fracture, antibiotic eluting implant, antibiotic-coated nail, tibia fracture, deep infection, interlocking nail, gentamycin coating, level of evidence: IV.
Introduction
Incidence of open fractures of long bones varies around 11.5 per lakh population per year. The incidence of open fractures of tibia is around 23.5% of all tibial fractures per year and comprises 0.2% of all injuries per year [1]. The risk of infection in an open fracture increases with increasing severity of injury on the Gustilo and Anderson grading system from <2% in Grade I to almost 50% in Grade III open fractures [2]. It was always thought to be mandatory to do a thorough surgical wound debridement within 6 h of injury [3]. However, a few recent studies have proven that there is no statistically significant difference in the incidence of infection in open fractures debrided surgically before or after 6 h [4]. A systematic review of multiple earlier studies concluded that antibiotic treatment reduces the incidence of infections in open fractures [5, 6]. The current recommendations for the management of open tibial fractures up to Grade III A are based on performing a thorough surgical debridement in stages as required, primary intramedullary nailing and immediate soft-tissue repair [7]. In a large study, study to prospectively evaluate reamed intramedullary nails in tibial shaft fractures, which included 1226 participants, they observed that there is no significant difference in infection rate between reamed and unreamed nails in the open fracture group [8]. To mitigate the morbidity due to deep infection, newer generation of biofilm-resistant implants is being investigated. Implants coated with broad-spectrum antimicrobials against potential colonizers appear to be one logical solution [9, 10, 11]. The antimicrobial eluting implants are recently becoming popular in research [12, 13]. A few studies that investigated the use of antibiotic-coated nails in open tibial fractures reported initial positive results [14, 15, 16]. A recent study published in 2017 [17] on the resource and cost consequences of using antibiotic-coated intramedullary nails compared to non-coated nails in open tibia fractures across four European centers concluded that using the antibiotic-coated implant in patients with high risk of infection (GAIII) was cost saving. The aim of this longitudinal follow-up study is to assess the clinical, radiological, and functional outcome in patients of open tibial diaphyseal fractures treated by antibiotic eluting intramedullary interlocking nail. For the purpose of this article, the words “antibiotic coated” and “antibiotic eluting” have been used interchangeably.
Methodology
A prospective longitudinal follow-up study was conducted on 18 consecutive patients with 20 tibial fractures attending this tertiary care orthopedic center between October 2016 and December 2018. All the patients were followed up for a minimum of 1 year after surgical intervention. Clearance was taken from the Institutional Ethical Committee before the conduct of the study.
Inclusion criteria
Patients aged between 18 and 65 years with open diaphyseal tibial shaft fractures of GA Grades II and IIIa and presenting within 72 h of injury.
Exclusion criteria
All non-consenting patients and those with other fracture grades than those mentioned above and patterns such as metaphyseal fractures involving proximal and distal 5 cm of tibia, pathological fractures, those with pre-existing deformities precluding nailing, and those with associated severe chest injury and severe polytrauma patients were excluded from the study.
Sample size calculation
The sample size was is calculated with an assumed deep infection rate of 5% in open tibial fractures Grades II and IIIA based on earlier studies and an expected margin of error (d) of ± 10% and confidence interval of 95%.
Eighteen consecutive and consenting patients with 20 tibial fractures visiting this trauma center after applying the inclusion and exclusion criteria were taken up for the study. Once the general condition is stabilized, the patients were planned to be taken up for surgery as early as possible. All participants were started on systemic intravenous antibiotics with a first-generation cephalosporin and an aminoglycoside at the time of initial presentation.
All participants were managed by thorough wound debridement done either as a one step or as a staged procedure. All fractures were fixed by antibiotic eluting intramedullary interlocking nail at index surgery (Ossipro Gentamicin Eluting Nails manufactured by Matrix Meditec Pvt. Ltd., India).
Adequate skin cover was achieved in all cases either by primary closure or by one of the various methods of skin grafting as decided by a specialist in reconstructive surgery. All other factors including period of immobilization, weight-bearing, and period and type of adjunctive physiotherapy and other therapies were kept similar in all participants. Patients were followed up at 6 weeks, 12 weeks, 6 months, and 12 months from the date of surgery.
Outcome measure
1. Functional outcome was measured using lower extremity functional scale (LEFS). It is a widely used validated scale for lower extremity musculoskeletal function. The LEFS is reliable, and construct validity was supported by existing literature. The sensitivity to change of the LEFS in the study by Binkley and Stratford was superior to that of the SF-36 which is a more elaborate assessment tool. The minimal clinically important difference (MCID) is 9 scale points (90% CI) [18]. Pre-injury scoring was done retrospectively before surgery. Follow-up scoring was done at 6 weeks, 3 months, 6 months, and 1 year after surgery 2. Radiological outcome was measured using radiological union scale in tibial fractures (RUST). The RUST scale is a validated tool for the assessment of union of tibial fractures with an intraclass correlation (ICC) of 0.75 (95% CI) in a study by Leow et al. It is a simple and powerful tool for scoring tibial fracture union objectively [19]. A study conducted by Fernando et al. shows that there was a significant interobserver agreement with ICC of 0.87 (95% CI 0.81–0.91) and intraobserver agreement with ICC of 0.88 (95% CI 0.85–0.91) [20]. Radiographic union was defined as union of at least 3 out of 4 cortices on plain X-ray which corresponds to a RUST score of more than 9. The same criteria were applied to define radiographic union in this study 3. For the purpose of this study, discharge from the wound/surgical site at any point after surgery was considered positive for surgical site infection. Development of infection in deeper layers such as fascia and bone requiring intervention such as removal of implant was considered positive for deep infection/implant related infection. The data were analyzed by paired Student’s t-test. Functional and radiological outcome at different time points was compared. Pearson correlation coefficient was calculated between functional and radiological outcomes at different time points. P < 0.05 was considered statistically significant. SPSS, version 24.0 software was used for analysis.
Results
Demographic profile
The mean age of patients included in this study was 40.3 years and median age of 35.5 years (range 20–60 years). About 72% of the study population (n = 13) were male and 28% (n = 5) were female.
Injury characteristics
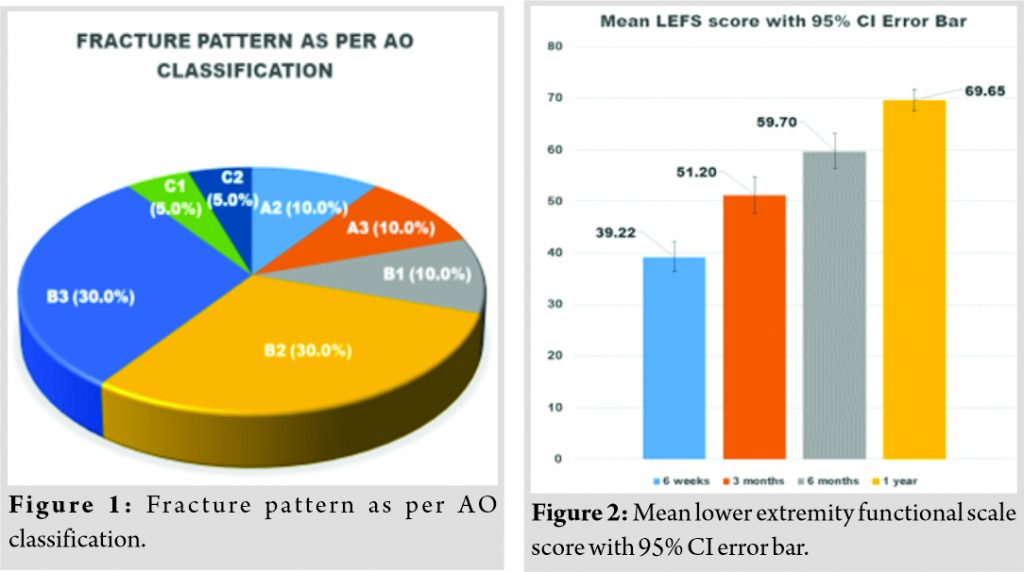
The mode of injury was road traffic accident in 65% of fractures (n = 13). The most common fracture classification was AO-42B2 (30% or n = 6) and AO-42B3 (30% or n = 6) on the AO/OTA classification system, as shown in (Fig. 1). There were 15 cases (75%) of Gustilo and Anderson Grade II fractures and 5 cases (25%) of Grade IIIA fractures included in this study. None of the associated injuries precluded the surgical management.
Management
Definitive fixation was done in all cases at the index surgery. About 85% of the cases (n = 17) had to undergo a single debridement at the index surgery. Three cases (15%) had to undergo two serial debridements spaced at 48–72 h before final skin closure. Primary closure of open wound was achieved in 80% of the cases (n = 16), whereas a delayed primary closure was obtained for skin in one case (5%). One case (5%) with a small defect was left to heal by secondary intention. Two cases (10%) had to undergo split skin grafting to cover the skin defect. All the cases were reamed before nailing and the maximum diameter of the intramedullary nail was used. All the cases were given a minimum of 72 h of prophylactic antibiotics. Except the two bilateral fracture cases (n = 4 or 20%), the remaining 80% of the cases (n = 16) were ambulated with help of support before discharge from hospital.
Outcome measurements
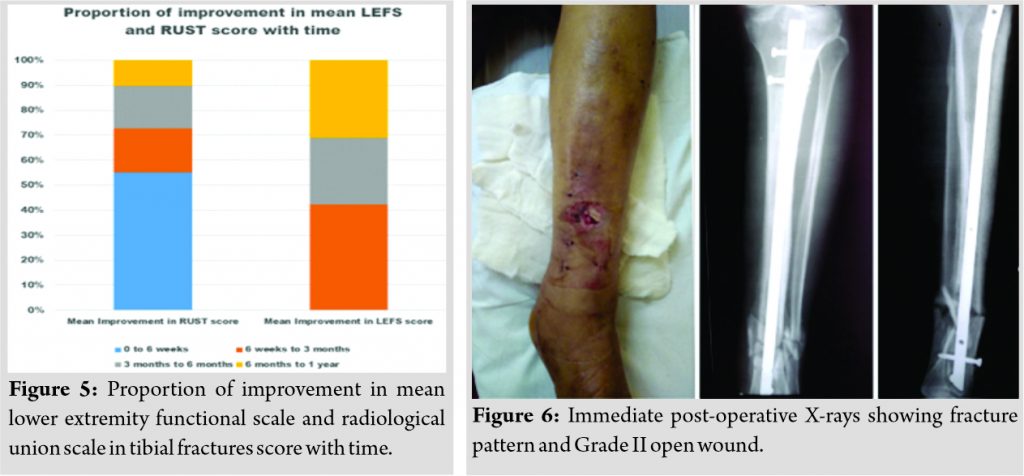
The pre-injury mean LEFS score was 74.20. There was a statistically significant improvement in the LEFS score at each point of the review. The mean LEFS score was 39.22 at 6 weeks which improved to 51.20 at 3 months and 69.65 at 1 year, as shown in (Fig. 2). Most of the average improvement in LEFS score occurred in the first 3 months, as shown in (Fig. 3), followed by a steady and statistically significant improvement at all points of review (P < 0.0001). On translation to clinical importance, significant improvement in score by more than MCID of 9 points (as per Binkley and Stratford study [18]) occurred from 6 weeks to 3 months and from 6 months to 1 year (mean difference > MCID of scale). However, the clinical improvement from 3 months to 6 months may not be clinically significant (mean difference < MCID of scale). Overall improvement in the scale was clinically significant (mean difference from 6 weeks to 1 year is 30.43 score points). The final LEFS mean score at 1 year did not reach the level of pre-injury mean score. All cases were independent ambulators at the end of 1 year. However, a majority (55%, n = 10) of them were not able to participate in recreational sports activities by the end of 1 year. Similarly, considering a RUST score of 0 at the time of acute fracture, the mean score improved to 5.95 by 6 weeks, to 7.85 at 3 months, and to 10.80 at 1 year, as shown in (Fig. 4). Most of the average improvement in RUST score occurred in the first 6 weeks, as shown in (Fig. 3), followed by a steady and statistically significant improvement at all points of review (P < 0.001). Clinically, all the fractures were united by 1 year and all the patients were independent ambulators by this time. The correlation factor between the LEFS and RUST scores was 0.497 at 6 months and 0.711 at 1 year, as shown in (Fig. 5). There were 2 cases (10%) of superficial surgical site infection, one of which was Grade II open injury and other was Grade IIIA open injury. Both cases had mild serous discharge in the initial weeks after surgery. They were managed by local wound wash without opening the deeper layers or exposing the implant. Both cases had no discharge at subsequent review points. There was one case of deep infection in a case of Grade II open fracture whose immediate post-operative photograph and radiograph is shown in (Fig. 6). The patient had persistent discharge from the wounds over interlocking bolts at 6 weeks after surgery. The original open wound had healed. Initially, the wound culture was negative and the patient was managed by local wound lavage at 6 weeks. However, the discharging sinus persisted which tested positive for Staphylococcus spp. sensitive to aminoglycosides. At 3 months, the patient was managed by debridement and removal of locking bolts. The intraoperative image, as shown in (Fig. 7), shows healed primary wound and incision and drainage of locking bolt sites along with bolt removal. The case went on to further improvement. No discharge was noted at 4 months and progressive union of fracture was noted in subsequent visits, as shown in (Fig. 8), which shows status of union at 6 months. The fracture was clinically and radiologically united (RUST score of 11) at 1 year, as shown in (Fig. 9) (radiographs) and (Fig. 10) (clinical photographs). Thus, in this study, the incidence of implant related/deep infection is 5% (n = 1).
Discussion
Infection in orthopedics has always been a difficult domain to manage. It may not be possible to completely eliminate infection in open fractures at this time. However, research is in progress on mitigating the incidence and severity of infections. The concept of biofilms, as such, is not new. It has been seen since the times of Anton Von Leeuwenhoek from the 17th century. The implication of biofilm was widely accepted after the name was coined and described by Donlan and Costerton [21]. Despite the revolution in design biomechanics and metallurgy, infection resistant implant is still an enigma. Earlier studies point out that coating the implant surface with a layer of antimicrobial which elutes locally for an initial period of time might reduce formation of biofilm and hence the infection rates [13]. In our study, the standard design interlocking tibial nail coated with gentamycin by dip-coating method of manufacturing was used. It is manufactured by Matrix Meditec Pvt. Ltd., India. An aminoglycoside is a preferred antibiotic for local prophylaxis because of wide spectrum of activity, low incidence of antimicrobial resistance, and cost-effectiveness. The implants are coated completely with a layer of gentamycin over a carrier made of biodegradable poly(D, L-)lactide. The concentration of drug is 1 mg/cm2 surface area of nail. The process of dip coating ensures that both the outer and inner surfaces of the hollow nail are coated uniformly. The locking bolts are also treated in a similar manner. The initial antibiotic burst action is about 30–40% elution within 3–4 days followed by uniform release for next 4–6 weeks maintaining the local drug concentration above therapeutic level. In this study, all the fractures reached union status by the end of 1 year. There was no significant difference in Grade II injuries when compared with Grade IIIA injuries in RUST score (10.91 vs. 10.73) and LEFS score (69.51 vs. 70.07) at the end of 1 year. There was one case of deep infection that required removal of all locking bolts. Although the surgical team was initially inclined to exchange the complete implant, it was finally decided to do it in stages if required. The rationale was that the initial open wound had healed well and fracture is already showing evidence of progressive healing (RUST score at 6 weeks was 5 and at 3 months was 7). The sinus discharge was from the locking bolt sites. Although the manufacturer claims antibiotic coating of the locking bolts also, the removal of the locking bolts led to uneventful subsidence of infection. There may be multiple factors leading to loss of antibiotic elution from the locking bolts. One such could be the friction during insertion with radial preload. Further studies are needed in this aspect to elaborate whether the procedure of instrumentation and handling has any effect on antibiotic elution. The point to note is that although there was a presumed medullary spread of infection initially, the nail was probably not colonized by the microbes. To comment that it is because of the antibiotic coating and elution is not possible with this limited evidence. Further larger studies are required for such conclusion to be made. (Table 1) shows the comparison of outcomes from our study with other similar studies in the literature.
Conclusion and Recommendations
There was no attrition of the participants. Although the contemporary literature has shown no deep implant-related infections, our study shows 5% rate of deep infection in our setting. Although it is reasonably arguable that there was no colonization of the nail despite presence of medullary spread of infection in the lone case of deep infection which healed uneventfully after locking bolt removal, it is immature to draw any conclusion at this point. The strength of this study lies in the fact that all the fractures had completely united by the end of 1 year. Thus, the rate of union in this study is 100%. Nevertheless, this being an observational study with single intervention has its own limitations in inference. In future, larger comparative studies are needed to draw bold conclusions to reflect on clinical practice. This study recommends more research be done on the development of reliable technology for coating of antimicrobial substance on the implants which will have a predictable and favorable elution pattern. Furthermore, the right choice of antimicrobial substance to be coated needs to be addressed. Large-scale comparative studies and randomized controlled trials are needed to be done to recommend routine use of antibiotic-coated nails in open tibial fractures at this time.
Clinical Message
Very few studies are available in existing literature on the use of antibiotic eluting implants in primary fixation of fractures. The concept of antimicrobial coating of implants is novel and is yet to find its place in the clinical practice. There are various aspects of this study that deserve mention. First, the incidence of deep infection is 5%, which is comparable to the other few available studies and it may be acceptable in open fractures considering higher potential for deep infection. Second and more importantly, all the fractures were united within expected time frame. Hence, one can infer that addition of a carefully chosen antimicrobial is probably not detrimental to bone healing. Third and finally, in the one case highlighted in this report, it could be inferred that the nail was probably not colonized. Such biofilm resistance can be explained by initial local concentration of drug achieved by reliable elution. However, this conjecture should be carefully interpreted at this time. The results can be considered preliminary and this study intends to trigger more clinical as well as basic science research in this domain.
References
1. Court-Brown CM, McBirnie J. The epidemiology of tibial fractures. J Bone Joint Surg Br 1995;77:417-21.
2. Gustillo RB, Mendoza RM, Williams DN. Problems in the management of Type III (severe) open fractures: A new classification of Type III open fractures. J Trauma 1984;24:742-6.
3. Giannoudis PV, Papakostidis C, Roberts C. A review of the management of open fractures of the tibia and femur. J Bone Joint Surg Br 2006;88:281-9.
4. Fernandes MC, Peres LR, de Queiroz AC Jr., Lima JQ Jr., Turíbio FM, Matsumoto MH. Open fractures and the incidence of infection in the surgical debridement 6 hours after trauma. Acta Ortop Bras 2015;23:38-42.
5. Patzakis MJ, Wilkins J, Moore TM. Use of antibiotics in open tibial fractures. Clin Orthop Relat Res 1983;178:31-5.
6. Gosselin RA, Roberts I, Gillespie WJ. Antibiotics for preventing infection in open limb fractures. Cochrane Database Syst Rev 2004;1:CD003764.
7. Patil NV, Padmananda GA. Intramedullary interlocking nailing in Type II and Type III open fractures of tibia-a clinical study. IOSR J Dent Med Sci 2015;14:1-3.
8. SPRINT Investigators, Bhandari M, Guyatt G, Tornetta P 3rd, Schemitsch E, Swiontkowski M, et al. Study to prospectively evaluate reamed intramedually nails in patients with tibial fractures (S.P.R.I.N.T.): Study rationale and design. BMC Musculoskelet Disord 2008;9:91.
9. McConoughey SJ, Howlin R, Granger JF, Manring MM, Calhoun JH, Shirtliff M, et al. Biofilms in periprosthetic orthopedic infections. Future Microbiol 2014;9:987-1007.
10. Geoffrey DH, Nicholas P, Elizabeth AG, Mehta S. Current concepts and ongoing research in the prevention and treatment of open fracture infections. Adv Wound Care (New Rochelle) 2015;4:59-74.
11. Vergidis P, Patel R. Novel approaches to the diagnosis, prevention, and treatment of medical device-associated infections. Infect Dis Clin North Am 2012;26:173-86.
12. Micheal JR, Steffen BR, Fuchs TF. Gentamycin coated tibia nails: Can we afford not to use them? Tech Orthop 2014;29:62-8.
13. Shiels SM, Bouchard M, Wang H, Wenke JC. Chlorhexidine-releasing implant coating on intramedullary nail reduces infection in a rat model. Eur Cell Mater 2018;35:178-94.
14. Metsemakers WJ, Reul M, Nijs S. The use of gentamicin-coated nails in complex open tibia fracture and revision cases: A retrospective analysis of a single centre case series and review of the literature. Injury 2015;46:2433-7.
15. Fassbender M, Minkwitz S, Kronbach Z, Strobel C, Kadow-Romacker A, Schmidmaier G, et al. Local gentamicin application does not interfere with bone healing in a rat model. Bone 2013;55:298-304.
16. Fuchs T, Stange R, Schmidmaier G, Raschke MJ. The use of gentamicin-coated nails in the tibia: Preliminary results of a prospective study. Arch Orthop Trauma Surg 2011;131:1419-25.
17. Taylor H, Wolf S, Paparouni K. The resource and cost consequences of using antibiotic coated intramedullary nails compared to non-coated nails in open tibia fractures across four European Centres. Value Health 2017;20:A399-811.
18. Binkley JM, Stratford PW. The lower extremity functional scale (LEFS): Scale development, measurement properties, and clinical application. North American orthopaedic rehabilitation research network. Phys Ther 1999;79:371-83.
19. Leow JM, Clement ND, Tawonsawatruk T, Simpson CJ, Simpson AH. The radiographic union scale in tibial (RUST) fractures: Reliability of the outcome measure at an independent centre. Bone Joint Res 2016;5:116-21.
20. Fernando AS, Ricardo BC, Matheus LA, Armando A. Reliability of the radiographic union scale in tibial fractures (RUST). Rev Bras Ortop 2017;52:35-9.
21. Donlan RM, Costerton JW. Biofilms: Survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev 2002;15:167-93.
 |
 |
| Dr. S Vignesh | Dr. Amresh Ghai |
| How to Cite This Article: Vignesh S, Ghai A. A Study on the Outcome of Antibiotic Eluting Intramedullary Interlocking Nails in the Primary Fixation of Gustilo and Anderson Grades II and IIIA Open Fractures of Tibia. Journal of Orthopaedic Case Reports 2020 December;10(9): 65-70. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com