[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
When we see patients with scaphoid fracture due to a direct blow injury, it is important to evaluate fracture type using three-dimensional computed tomography to decide the direction of the headless screw.
Case Report | Volume 10 | Issue 9 | JOCR December 2020 | Page 98-101 | Takuya Tada, Kenji Onuma, Koji Sukegawa, Yuya Otake, Tomonori Kenmoku, Masashi Takaso. DOI: 10.13107/jocr.2020.v10.i09.1920
Authors: Takuya Tada[1], Kenji Onuma[1], Koji Sukegawa[1], Yuya Otake[1], Tomonori Kenmoku[1], Masashi Takaso[1]
[1]Department of Orthopaedic Surgery, Kitasato University School of Medicine, Japan.
Address of Correspondence:
Dr. Takuya Tada,
Kenji Onuma, Department of Orthopaedic Surgery, Kitasato University School of Medicine. Japan.
E-mail: onuma@med.kitasato-u.ac.jp
Abstract
Introduction: Two methods using cannulated headless screws can be used for scaphoid fractures: Inserting the screw through the distal fragment and then into the proximal fragment through a palmar approach under direct vision or fluoroscopic guidance and inserting the screw in the proximal-to-distal direction through a dorsal approach with fluoroscopic guidance. These methods are sometimes difficult to use in oblique fractures when trying to achieve screw fixation perpendicular to the fracture plane.
The most common mechanism of injury in the scaphoid fracture is forceful wrist hyperextension and punching something. Less commonly, a direct blow to the wrist also can cause a fracture. The mechanism of fracture by a direct blow to the wrist is not completely clear.
Case Presentation: We experienced two rare cases of scaphoid fracture in goalkeepers sustained when they saved a goal by contacting the soccer ball with the palm of their hand. Both fractures were proximal oblique fractures. We performed through a dorsal approach to insert the screws in the distal-to-proximal direction under direct vision assisted with fluoroscopy. Bone union was noted after surgery in both cases. They returned to their occupations without wrist pain.
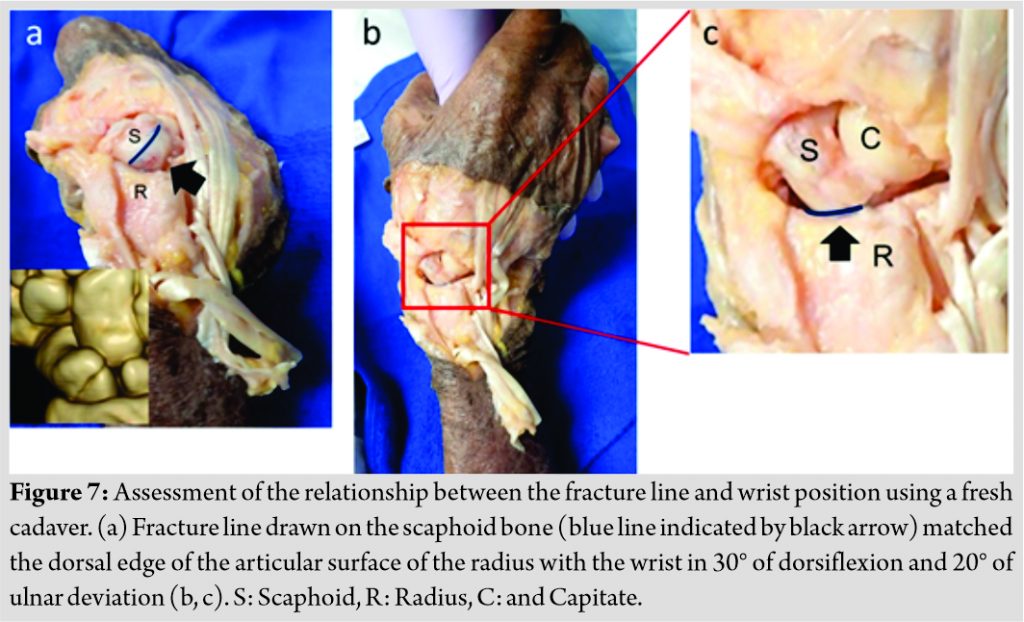
We investigated the relationship between the fracture line and wrist position using a fresh cadaver. The experiment revealed that the fracture line of the scaphoid matched the dorsal edge of the articular surface of the radius with the wrist in 30° of dorsiflexion and 20° of ulnar deviation.
Conclusion: In this report, we reported rare cases of scaphoid fracture due to contact with the soccer ball on the palm. We propose a surgical approach for an oblique fracture of the proximal scaphoid that used guide wires and screws, but was performed through a dorsal, and not palmar, approach to insert the screws in the distal-to-proximal direction.
We presume that coronal shear stress to the scaphoid bone occurred when the palm contacted the ball with the wrist positioned at 30° dorsiflexion and 20° ulnar deviation.
Keywords: Wrist injuries, scaphoid bone, imaging, three-dimensional, fracture fixation, internal.
Introduction
Scaphoid fractures are the most common fractures of the carpal bones. The incidence is highest in males 15–29 years old, usually secondary to a fall from an upright position, and is often seen in contact sports (most commonly football) [1]. The most common mechanism of injury in the scaphoid fracture is forceful wrist hyperextension or punching something [2]. Less commonly, a direct blow to the wrist also can cause a fracture [2]. The mechanism of fracture by a direct blow to the wrist is not completely clear. We experienced two rare cases of scaphoid fracture when goalkeepers saved a goal by contacting the ball with the palm of their hands.
The acute scaphoid fracture is usually treated conservatively with casting or with surgery using headless screws or Kirschner wire [2]. Although headless screw fixation using conventional palmar and dorsal approaches is widely performed, in our cases of a proximal oblique fracture, we used the dorsal approach and performed internal fixation with headless compression screws inserted from the distal to the proximal fragment.
Cases
Case 1
An 18-year-old female professional soccer goalkeeper saved a hard shot with her left hand. She had no prior experience of falling on an outstretched hand (FOOSH) or punching the ball during the game. She presented to our hospital with a history of the left wrist pain 4 weeks after the injury. Physical examination showed tenderness of the anatomical snuffbox. 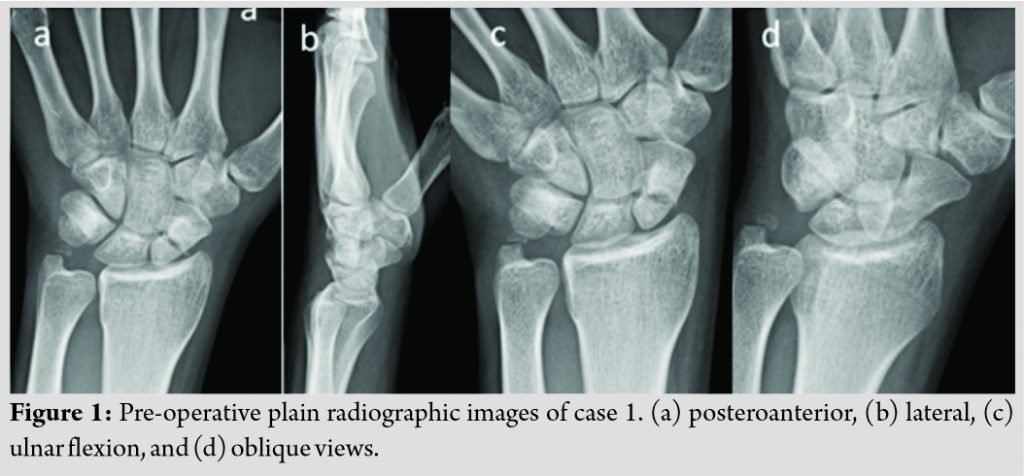
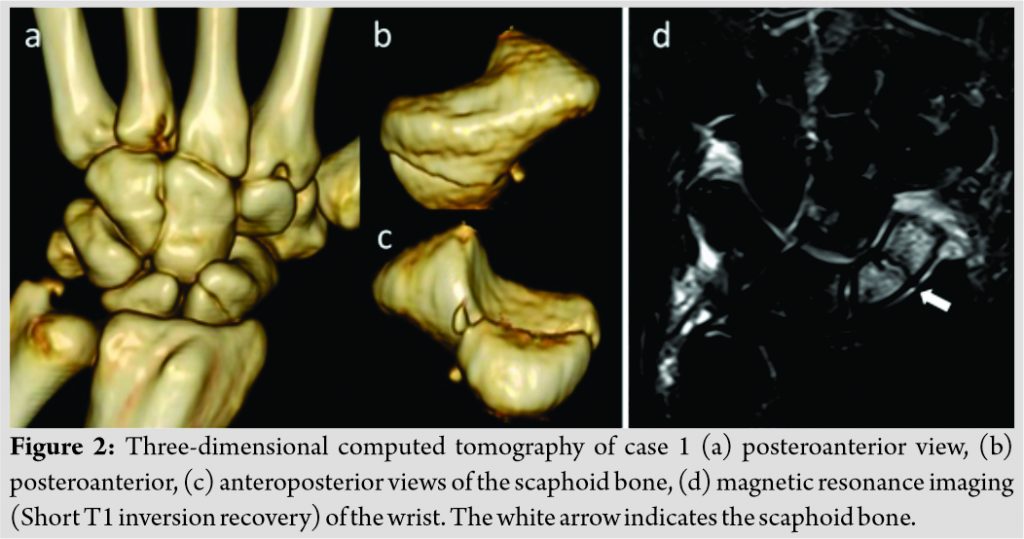
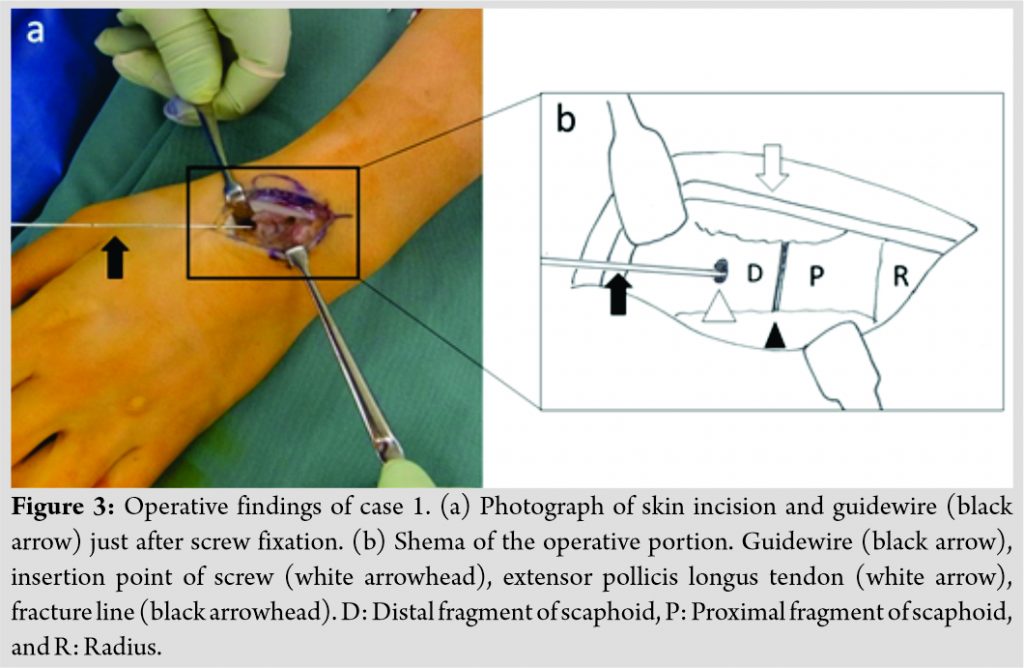
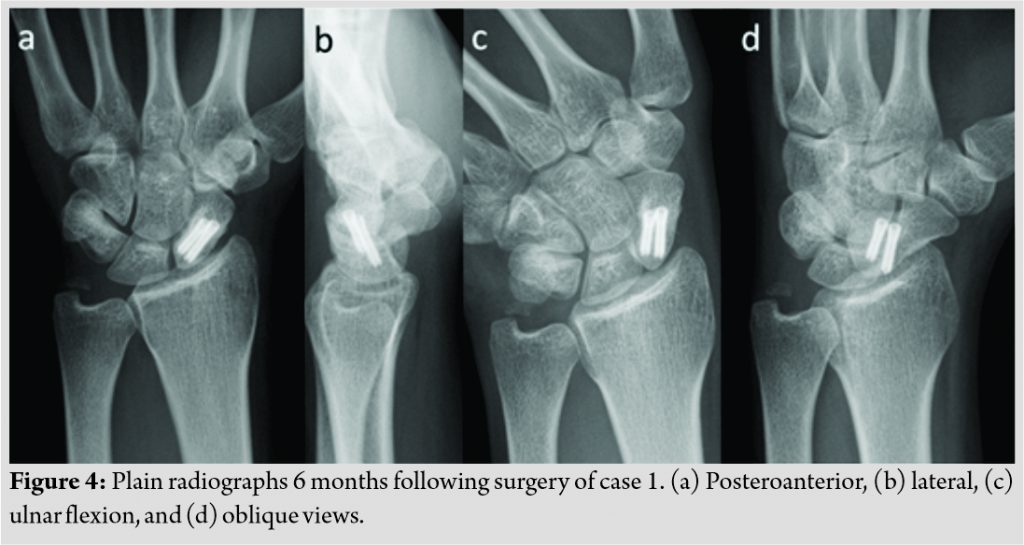
Although we had planned screw fixation with headless compression screws, we thought it would be difficult to insert the screws perpendicular to the fracture plane using conventional methods. The operation was performed using a dorsal approach. An incision into the dorsal capsule was made avoiding the dorsal intercarpal ligament. The scaphoid bone and its fracture line were exposed. Two guide wires were inserted perpendicular to the fracture plane under direct vision assisted by fluoroscopy, followed by two Acutrac® II micro screws (Acumed, Hillsboro, OR, USA) 11 and 13 mm in length in the distal-to-proximal direction (Fig. 3a, b). She was placed in a thumb spica splint after the operation for 3 weeks. Bone union was noted approximately 2 months after surgery (Fig. 4). She returned to soccer without wrist pain.
Case 2
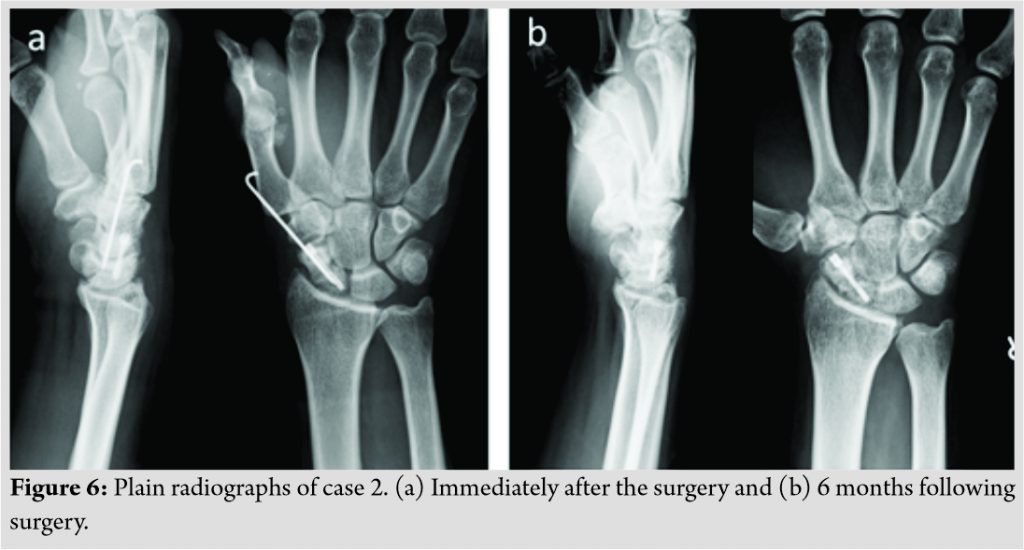
A 25-year-old male amateur soccer goalkeeper saved a hard shot with his right hand. He also had no prior experience of FOOSH or punching the ball during the game. He presented to our hospital with a history of the right wrist pain 10 months after the injury. Physical examination showed reduced range of motion of his wrist and tenderness of the anatomical snuffbox. Plain radiographs suggested a middle third fracture of the scaphoid (Fig. 5a), and 3D CT showed a type 1-B3 fracture by Moritomo’s modified Herbert classification [3] (Fig. 5b-d).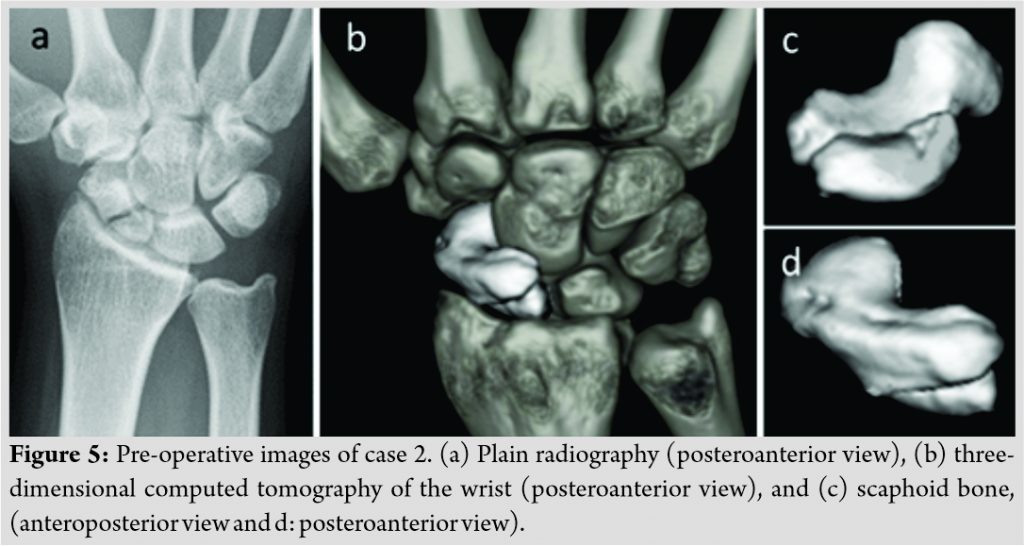
We investigated the relationship between the fracture line and wrist position using a fresh cadaver (Fig. 7). The experiment revealed that the fracture line of the scaphoid matched the dorsal edge of the articular surface of the radius with the wrist in 30° of dorsiflexion and 20° of ulnar deviation.
Discussion
The Herbert classification [4] is widely known as a classification of scaphoid fractures and nonunion based on plain radiography. As the shape of the scaphoid bone is complex, 3D imaging is more useful than plain radiography for classification of fracture type. Oka and Moritomo [5] reported that while 3D images of B1 (distal oblique) and B2 (waist) scaphoid nonunion are different, both fracture lines appear similar on oblique radiographs. In our case, although the PA radiograph suggested a waist fracture, the actual diagnosis was of an oblique fracture on 3D imaging. The fracture type in our case was not typical and not classifiable according to the conventional Herbert classification. According to the modified Herbert classification based on 3D images by Moritomo et al. [3], our case was classified as 1-B3.
The most common mechanism of injury in this fracture is forceful wrist hyperextension, usually from a FOOSH [2]. Middle-third scaphoid fractures are probably caused by extreme wrist extension with compression of the radial side of the palm [2]. Less commonly, a direct blow to the wrist also can cause a fracture [2]. Holii et al. [6] reported that the mechanism of scaphoid waist fractures involves not only wrist hyperextension but also punching. The concentration of external force to the second metacarpal and its transmission to the trapezium and trapezoid produces shear stress at the waist of the scaphoid [6]. In our cases, the patient did not report hyperextension of their wrist or punching as the cause of injury, but saving the ball with their palms.
To the best of our knowledge, non-FOOSH scaphoid fractures in goalkeepers have been reported only once [7]. The fracture type in the two cases in that earlier report was a proximal pole fracture [7]. However, as they did not show 3D images in their report, the actual fracture type is unclear. Although the mechanism of non-FOOSH scaphoid fractures has not been verified, Johnson et al.’s two cases and our two cases were all B3 (proximal pole) fractures [7]. We infer some relationships among the four cases.
We investigated the relationship between the fracture line and wrist position using a fresh cadaver. The experiment using a fresh cadaver revealed that the fracture line of the scaphoid matched the dorsal edge of the articular surface of the radius with the wrist in 30° of dorsiflexion and 20° of ulnar deviation. Although the biomechanical examination is required, we presume that coronal shear stress to the scaphoid bone occurred while contacting the ball on the palm with the wrist positioned at 30° dorsiflexion and 20° ulnar deviation.
Two methods are common for scaphoid fracture fixation using cannulated headless compression screws [2]. The palmar approach, with guidewires and screws inserted from distal to proximal under direct vision or fluoroscopy, has achieved popularity since its development due to the excellent clinical outcome. Recent work, however, has shown that the dorsal approach provides better targeting and more precise screw placement. In our case, we used the dorsal approach, and not the palmar approach, for distal-to-proximal fixation. To the best of our knowledge, this approach to an oblique scaphoid fracture is the first to be reported in the English literature. Our method allows guide wires and screws to be inserted through a non-articular surface of the scaphoid bone perpendicular to the fracture plane, as opposed to the conventional dorsal approach, which is associated with cartilage damage of the proximal fragment, or the palmar approach, which induces cartilage damage to the distal scaphotrapezoidal joint and does not allow vertical insertion to the fracture line for oblique fractures. As our method does not cross articular cartilage, we suggest its use for type 1-B1 and type 1-B3 fractures. Jurkowitsch et al. [8] reported in their biomechanical analysis that fixation with two headless compression screws increases rotational stability compared with single-screw fixation. In our case 1, as the fracture plane was wide and the screw length was short, we used two headless compression screws following two guidewires temporarily inserted to increase rotational stability.
Conclusion
We reported rare cases of scaphoid fracture due to contact with the soccer ball on the palm. We presume that coronal shear stress to the scaphoid occurred while contacting the ball on the palm with the wrist positioned at 30° dorsiflexion and 20° ulnar deviation. We suggest a dorsal approach with distal-to-proximal fixation for scaphoid oblique fractures of type 1-B3. Further, investigation is required to reveal the mechanism of the scaphoid fracture and long-term clinical results.
Clinical Message
When we see patients with scaphoid fracture due to a direct blow injury, it is important to evaluate fracture type using 3D CT to decide the direction of the headless screw. A dorsal approach with distal-to-proximal fixation is a useful procedure for oblique scaphoid fractures to allow the insertion of the screw perpendicular to the fracture plane.
References
1. Duckworth AD, Jenkins PJ, Aitken SA, Clement ND, Court-Brown CM, McQueen MM. Scaphoid fracture epidemiology. J Trauma Acute Care Surg 2012;72:41-5.
2. Dias J, Kantharuban S. Treatment of scaphoid fractures: European approaches. Hand Clin 2017;33:501-9.
3. Moritomo H, Murase T, Oka K, Tanaka H, Yoshikawa H, Sugamoto K. Relationship between the fracture location and the kinematic pattern in scaphoid nonunion. J Hand Surg Am 2008;33:1459-68.
4. Filan SL, Herbert TJ. Herbert screw fixation of scaphoid fractures. J Bone Joint Surg Br 1996;78:519-29.
5. Oka K, Moritomo S. Current management of scaphoid nonunion based on the biomechanical study. J Wrist Surg 2018;7:94-100.
6. Horii E, Nakamura R, Watanabe K, Tsunoda K. Scaphoid fracture as a “puncher’s fracture”. J Orthop Trauma 1994;8:107-10.
7. Johnson MR, Fogarty BT, Alitz C, Gerber JP. Non-FOOSH scaphoid fractures in young athletes: A case series and short clinical review. Sports Health 2013;5:183-5.
8. Jurkowitsch J, Dall’Ara E, Quadlbauer S, Pezzei C, Jung I, Pahr D, et al. Rotational stability in screw-fixed scaphoid fractures compared to plate-fixed scaphoid fractures. Arch Orthop Trauma Surg 2016;136:1623-8.
 |
 |
 |
 |
 |
 |
| Dr. Takuya Tada | Dr. Kenji Onuma | Dr. Koji Sukegawa | Dr. Yuya Otake | Dr. Tomonori Kenmoku | Dr. Masashi Takaso |
| How to Cite This Article: Tada T, Onuma K, Sukegawa K, Otake Y, Kenmoku T, Takaso M. A dorsal approach for the distal-to-proximal internal fixation of oblique scaphoid fractures. Journal of Orthopaedic Case Reports 2020 December;10(9): 98-101 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com