[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Masquelet technique has been well described in upper limb but it can be used judiciously in lower limb, especially foot to reconstruct the defect, restore the length, minimize implant left in situ, and achieve complete functional recovery for the patient.
Case Report | Volume 10 | Issue 9 | JOCR December 2020 | Page 118-120 | Abhinav D Jogani, Vinayak Garje, Prakash K George, Tushar Rathod, Shubhanshu M Bhaladhare . DOI: 10.13107/jocr.2020.v10.i09.1930
Authors: Abhinav D Jogani[1], Vinayak Garje[1], Prakash K George[1], Tushar Rathod[1], Shubhanshu M Bhaladhare[1]
[1]Department of Orthopaedics, Seth G.S. Medical College and KEM Hospital, Parel, Mumbai. Maharashtra. India.
Address of Correspondence:
Dr. Prakash K George,
Room 305, RMO Hostel, KEM Hospital, Parel, Mumbai – 400 012. Maharashtra. India.
E-mail: drprakashkgeorge@gmail.com
Abstract
Introduction: The literature regarding reconstruction of foot bone defects is limited. The reconstruction of diaphyseal bone defects is technically challenging and is often associated with poor outcomes. Associated osteomyelitis adversely affects the healing rates following a reconstruction procedure.
Case Report: We report a case of a 62-year-old male with lytic lesion involving the head of first metatarsal and proximal part of proximal phalanx following osteomyelitis treated with a two-stage reconstruction utilizing a modification of Masquelet’s-induced membrane technique. A follow-up at 24 months post-surgery revealed a fully incorporated fibular graft with satisfactory functional outcomes.
Conclusion: This two-stage modification of Masquelet technique provided an effective method to reconstruct the defect and restoration of the metatarsal length using minimal hardware to achieve a good functional recovery of the patient.
Keywords: Masquelet technique, first metatarsal reconstruction, fibula strut graft.
Introduction
The reconstruction of diaphyseal bone defects is a technically demanding procedure which is often associated with complications. Defects <2 cm and up to 4 cm can be treated with autogenous bone grafting [1]. For defects greater than 5 cm, a vascularized fibula autograft and the Ilizarov bone transfer techniques are commonly used, but they are associated with several disadvantages. When the distraction osteogenesis method is used, complications such as pin-tract infection, malunion, non-union, and problems with the docking site have been reported, while the need for long-term application of the external fixator lowers the patient compliance. The treatment involves surgical debridement of bone and soft tissue leaving behind a bone defect. When implants are associated with infection, microorganisms typically grow into biofilms, which protect bacteria from antimicrobial treatment and the host immune response [2]. Osteomyelitis further increases the chances of post-operative infection, thus adversely affecting the incorporation of the bone graft used for the reconstruction. The literature regarding reconstruction of foot bone defects is limited. The purpose of this study is to present a case report with an extensive bone defect of the first metatarsal bone following osteomyelitis which was treated with a two-stage reconstruction utilizing a modification of Masquelet’s-induced membrane technique.
Case Report
We report a case of a 62-year-old male who presented with pain in the left foot for 5 months. There was no history of trauma. He had an unremarkable medical and family history. Clinical examination revealed mild diffuse swelling of the region with tenderness on deep palpation and restricted movement of the metatarsophalangeal joint. Skin overlying was normal without any redness or dilated veins.
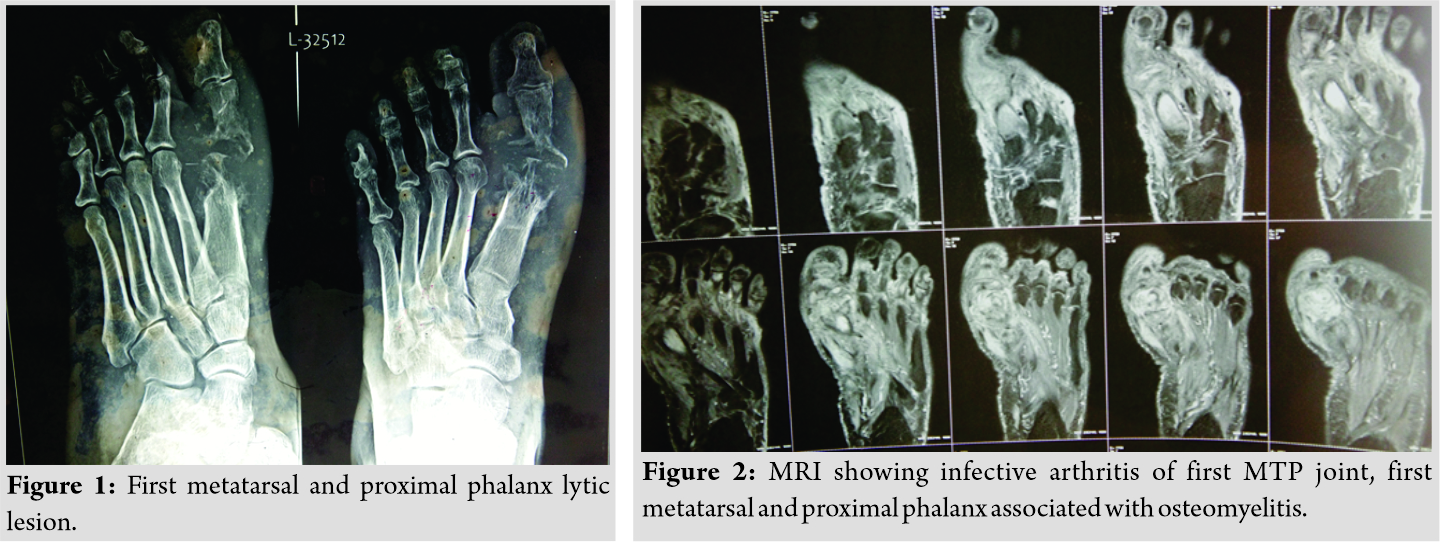
The patient was investigated and radiographs revealed a geographic lytic lesion involving the head of first metatarsal and proximal part of proximal phalanx (Fig. 1). Magnetic resonance imaging also indicated presence of Infective arthritis of first metatarsophalangeal joint with associated osteomyelitis (Fig. 2). Open debridement was carried out till bleeding bone was visible leaving behind a bone defect of 4 cm. Antibiotic cement spacer was placed which was fixed with an intramedullary K-wire (Fig. 3).
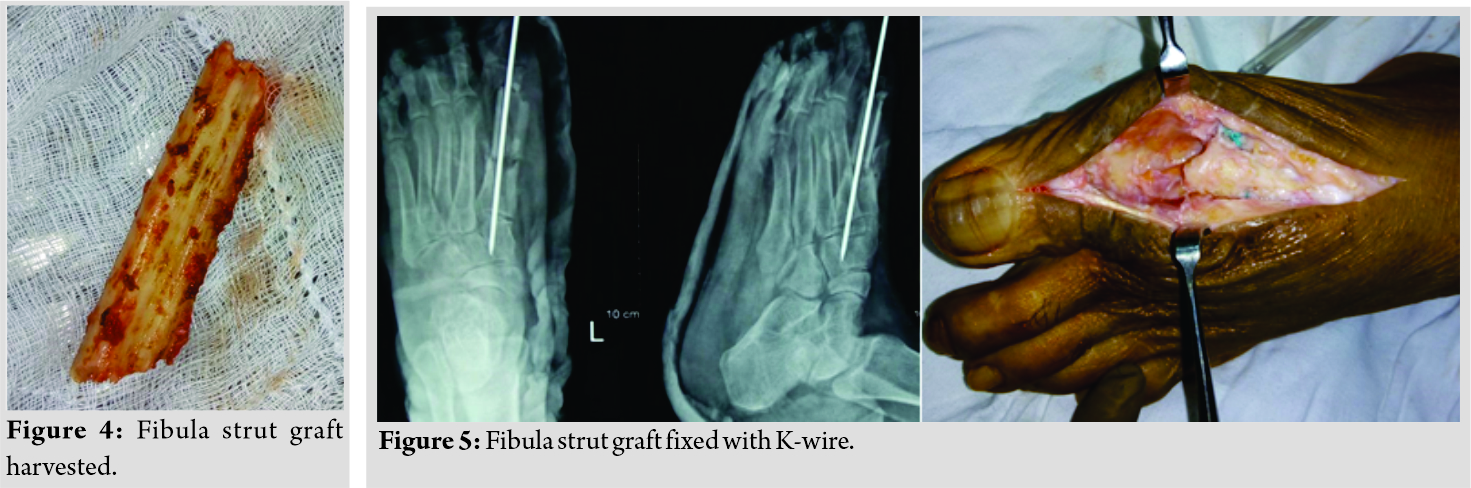
Intraoperative culture revealed the organism to be Methicillin-resistant Staphylococcus aureus and antibiotics were given as per culture sensitivity report. The second stage of reconstruction was done after 6 weeks. The antibiotic cement spacer was removed taking care to preserve the induced membrane and non-vascularized fibula strut graft of 4 cm (Fig. 4) was put in its place within the induced membrane.
The graft was fixed with a single intramedullary K-wire (Fig. 5). Finally, the membrane was sutured for the creation of a local biological chamber, which promotes bone regeneration and graft uptake [3]. The patient was on non-weight-bearing rehabilitation protocol for 3 months postoperatively until the bone graft had incorporated radiologically. Partial weight-bearing was started at 3-month post-surgery and full weight-bearing at 5 months was allowed. Follow-up at 24 months post-surgery revealed a fully incorporated fibular graft and patient walking full weight-bearing (Fig. 6).
Discussion
The free vascularized fibular autograft and distraction osteogenesis still remain the most common long bone defect reconstruction methods. Despite its reported advantages, distraction osteogenesis has been associated with several drawbacks such as technical difficulties, stiffness of adjacent joints, prolonged distraction time, and pin site infections [4, 5, 6, 7, 8]. We performed a modification of Masquelet’s-induced membrane technique using a fibular strut graft that provided better structural support. This limited the implant requirement to a single K-wire, which was, removed later on thus decreasing chances of recurrent infection. The advantages of this technique are that the complications of external fixators are minimized and restoration of normal length of metatarsal bone can be achieved. Although several studies exist on the Masquelet technique, there are only limited studies regarding restoration of complex injuries of the foot [9, 10, 11]. Pelissier et al. had reported a case of the dorsal aspect of the foot injury where the induced membrane and spongy autograft technique were used to reconstruct the metatarsal arch. Bone healing occurred and the results were satisfactory [10]. Largey et al. have reported another case of a patient presenting with a defect of the medioplantar region of the foot. The induced membrane technique was used to reconstruct the complete medial cuneiform loss and the saphenous cross-leg flap was used to manage the soft-tissue deficit. The authors stated an acceptable functional outcome [9]. The induced membrane technique used in this study for reconstruction of first metatarsal has many advantages. At the first stage, the use of cement spacer acts like as an additional support, it promotes the formation of the pseudosynovial membrane and provides high concentration of local antibiotics at the site of injury. Furthermore, an ideal environment for bone graft is created, thereby increasing the chances of union.
Conclusion
Reconstruction of bone defects is an extremely challenging process, especially when complicated by osteomyelitis. The two-stage modification of Masquelet technique is an effective method to reconstruct the defect and restoration of the metatarsal length using minimal hardware to achieve a good functional recovery of the patient.
Clinical Message
Two-stage modification of Masquelet technique provided an effective method to reconstruct the defect, restore the length, minimize implant left in situ, and achieve complete functional recovery for reconstruction of metatarsal bone defects, especially following osteomyelitis.
References
1. Stafford PR, Norris BL. Reamer-irrigator-aspirator bone graft and bi Masquelet technique for segmental bone defect nonunions: A review of 25 cases. Injury 2010;41:S72-7.
2. Patzakis MJ, Zalavras CG. Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: Current management concepts. J Am Acad Orthop Surg 2005;13:417-27.
3. Calori GM, Giannoudis PV. Enhancement of fracture healing with the diamond concept: The role of the biological chamber. Injury 2011;42:1191-3.
4. Masada K, Fujita S, Fuji T, Ohno H. Complications following metatarsal lengthening by callus distraction for brachymetatarsia. J Pediatr Orthop 1999;19:394-7.
5. Arata J, Morimoto N, Soeda H, Kometani A, Abe S, Suzuki S. Nonincisional osteotomy for gradual lengthening by callus distraction in the hand and foot. Ann Plast Surg 2011;67:232-4.
6. Lee DY, Choi IH, Yoo WJ, Lee SJ, Cho TJ. Application of the Ilizarov technique to the correction of neurologic equinocavovarus foot deformity. Clin Orthop Relat Res 2011;469:860-7.
7. Lee KB, Park HW, Chung JY, Moon ES, Jung ST, Seon JK. Comparison of the outcomes of distraction osteogenesis for first and fourth brachymetatarsia. J Bone Joint Surg Am 2010;92:2709-18.
8. Wilusz PM, Van P, Pupp GR. Complications associated with distraction osteogenesis for the correction of brachymetatarsia: A review of five procedures. J Am Podiatr Med Assoc 2007;97:189-94.
9. Largey A, Faline A, Hebrard W, Hamoui M, Canovas F. Management of massive traumatic compound defects of the foot. Orthop Traumatol Surg Res 2009;95:301-4.
10. Pelissier P, Bollecker V, Martin D, Baudet J. Foot reconstruction with the “bi-Masquelet” procedure. Ann Chir Plast Esthet 2002;47:304-7.
11. Huffman LK, Harris JG, Suk M. Using the bi-Masquelet technique and reamer-irrigator-aspirator for post-traumatic foot reconstruction. Foot Ankle Int 2009;30:895-9.
 |
 |
 |
 |
 |
| Dr. Abhinav D Jogani | Dr. Vinayak Garje | Dr. Prakash K George | Dr. Tushar Rathod |
Dr. Shubhanshu M Bhaladhare |
| How to Cite This Article: Jogani AD, Garje V, George PK, Rathod T, Bhaladhare SM. Reconstruction of First Metatarsal Bone Loss Following Osteomyelitis by a modified Masquelet Technique: A Case Report. Journal of Orthopaedic Case Reports 2020 December;10(9): 118-120 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com