[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
The key learning objective from this article is that rhabdomyolysis induced acute kidney injury must always be ruled out in geriatric patients of trivial trauma with extensive soft tissue bruising, as the condition has a very favorable prognosis, if promptly detected and treated.
Case Report | Volume 11 | Issue 1 | JOCR January 2021 | Page 16-19 | Sumit Banerjee, Akshat Gupta, Jeshwanth N. DOI: 10.13107/jocr.2021.v11.i01.1946
Authors: Sumit Banerjee[1], Akshat Gupta[1], Jeshwanth N[1]
[1]Department of Orthopaedic Surgery, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
Address of Correspondence:
Dr. Akshat Gupta,
Department of Orthopaedic Surgery, All India Institute of Medical Sciences, Jodhpur, Rajasthan. India.
E-mail: mirage1.akshat@gmail.com
Abstract
Introduction: Crush syndrome refers to the systemic manifestation of muscle cell injury following release of myocyte contents into the blood circulation. It is seen most commonly in patients sustaining high-energy trauma. Acute kidney injury is one of the most serious complications of crush syndrome and is an important cause of mortality in these patients. In contrast, the occurrence of rhabdomyolysis in patients sustaining low-energy trauma is sparsely reported in the literature. The authors report one such rare case.
Case Report: The patient was a 77-year-old hypertensive male who presented to the emergency following an episode of slip and fall at home. After prompt resuscitation, he was sent for radiological evaluation which revealed fractures of the left inter-trochanteric femur and left proximal humerus. Meanwhile, laboratory investigations showed grossly deranged renal parameters, along with elevated serum creatinine phosphokinase levels (more than 5 times the baseline). A diagnosis of acute kidney injury secondary to traumatic rhabdomyolysis was made. Medical management included adequate intravenous fluid administration combined with strict input-output monitoring. Subsequently, the patient underwent closed reduction and internal fixation of the inter-trochanteric femur fracture with a proximal femoral nail. However, fracture of the proximal humerus was managed non-operatively with sling immobilization as patient refused to give consent for a second surgery.
Conclusion: Although rare, acute kidney injury secondary to rhabdomyolysis can occur in patients with low-energy trauma. It is important not to confuse it with chronic renal insufficiency, especially in geriatrics many of whom are long-standing hypertensives.
Keywords: Acute kidney injury, crush syndrome, low-energy trauma, rhabdomyolysis.
Introduction
Crush injury refers to injury resulting from direct physical trauma to the muscles secondary to a crushing force [1, 2]. Crush syndrome, on the other hand, is the systemic manifestation of traumatic rhabdomyolysis due to breakdown of myocytes and subsequent release of their contents into blood circulation [1, 2]. The condition was first described by Eric Bywaters during World War II, and therefore, it is also sometimes referred to as Bywater’s syndrome [3]. Although traditionally associated with wartime injuries, crush syndrome is also seen in civilian life, especially, in incidences involving high-energy trauma-collapse of heavy structures during earthquakes/landslides, road-traffic accidents, assaults, etc. [2, 4, 5]. On an average, the incidence of crush syndrome in trauma patients ranges from 2 to 15% [1, 6]. It can go as high as 30% in earthquake victims [6]. Rarely, crush syndrome and rhabdomyolysis can also be seen in certain low-energy traumatic injuries which result in prolonged immobilization of the body, for example, positioning during surgery, loss of consciousness, and compression of a body part due to stroke/intoxication [2, 4, 5]. However, such cases have been sparsely reported in the literature. In this study, we present one such case of acute kidney injury (AKI) secondary to rhabdomyolysis in a patient who sustained a minor slip and fall at home.
Case Description
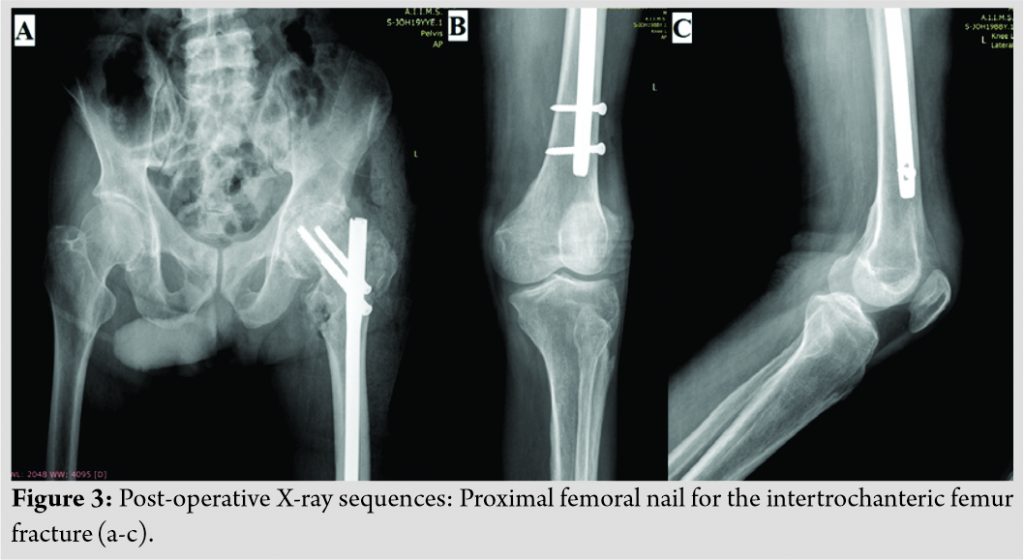
The patient was a 77-year-old male who presented to the emergency with the chief complaints of sudden onset pain in his left hip and shoulder following an episode of slip and fall at home 2 days ago. He was a known case of hypertension, for which he had been taking treatment for the past 15 years. Clinical examination revealed extensive bruising over the chest, left arm, forearm, as well as the medial aspect of the entire left thigh (Fig. 1). Movements of involved hip and shoulder joints were extremely painful and restricted. There was no distal neurovascular deficit in any of the involved limbs. Laboratory investigations revealed anemia (Hb 8.5 g/dl), deranged renal parameters (blood urea was 266 mg/dl and serum creatinine 3.46 mg/dl), elevated serum potassium (5.73 mmol/L), and uric acid (10.4 mg/dl). Coagulation profile was within normal limits. This was initially attributed to the patient’s long-standing hypertension, and hence, adequate fluid resuscitation was undertaken with a strict input-output monitoring. Serial blood gas analysis was also done. Thereafter, the patient was sent for radiological evaluation. The latter revealed fracture of the left inter-trochanteric femur with associated fracture of the left proximal humerus (Fig. 2). Contrary to the extent of contusions, X-rays did not reveal any bony injury to the chest/thigh and forearm.
The patient was closely monitored for any signs of deteriorating renal function. However, due to prompt and adequate administration of intravenous fluids (normal saline), his renal profile showed significant improvement (blood urea came down to 79 mg/dl and serum creatinine to 0.68 mg/dl). This led us to suspect that the derangement in kidney function was probably due to rhabdomyolysis-related AKI and not chronic kidney disease (CKD) secondary to hypertension. Raised levels of creatinine phosphokinase (CPK) (865 U/L; normal in adult males is <171 U/L) confirmed the same. A positive test for serum myoglobin/myoglobin degradation products further validated the diagnosis.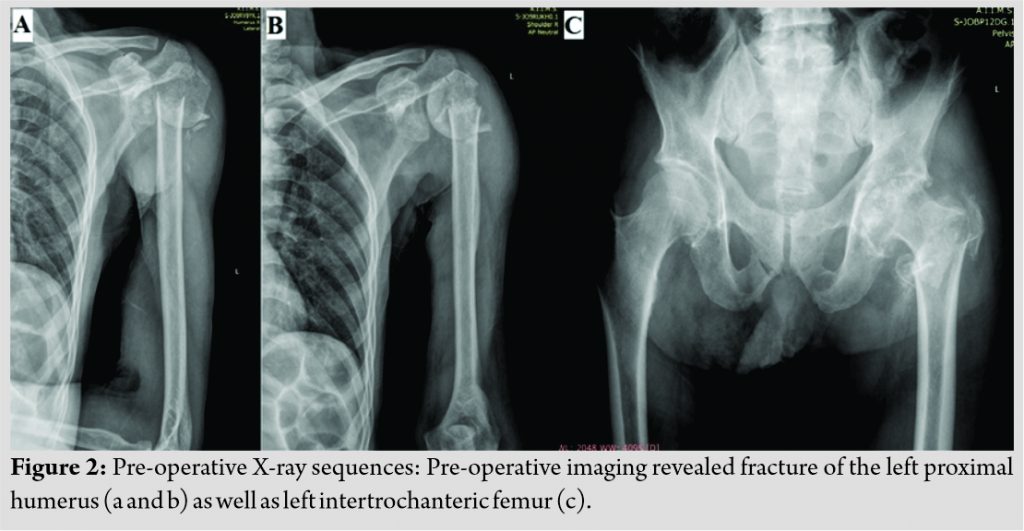
Discussion
Crush syndrome was first described in the British Medical Journal in 1941 by Eric Bywaters and is therefore also known as Bywaters syndrome [1, 3, 5, 7]. Crush injuries – war injuries, earthquakes, tsunamis, landslides, mining accidents, etc., have one thing in common – they usually result from high or extremely high-energy trauma.

Conclusion
The deceptive nature of the disease, especially in geriatric patients who suffer from a multitude of comorbidities, requires a high index of suspicion when dealing with such cases. If not promptly diagnosed and treated, it can cause significant patient morbidity as well as mortality.
Clinical Message
Acute kidney injury secondary to rhabdomyolysis in patients sustaining low-energy trauma is a rare but life-threatening condition. It should not be confused with chronic renal insufficiency in geriatric patients many of whom are long-standing hypertensives. In such cases, a detailed history, strong clinical suspicion, and close monitoring of the patient’s renal parameters are of paramount importance.
References
1. Rajagopalan S. Crush injuries and the crush syndrome. Med J Armed Forces India 2010;66:317-20.
2. Genthon A, Wilcox SR. Crush syndrome: A case report and review of the literature. J Emerg Med 2014;46:313-9.
3. Peiris D. A historical perspective on crush syndrome: The clinical application of its pathogenesis, established by the study of wartime crush injuries. J Clin Pathol 2017;70:277-81.
4. Jagodzinski NA, Weerasinghe C, Porter K. Crush injuries and crush syndrome-a review. Part 1: The systemic injury. Trauma 2010;12:69-88.
5. Chavez LO, Leon M, Einav S, Varon J. Beyond muscle destruction: A systematic review of rhabdomyolysis for clinical practice. Crit Care 2016;20:135.
6. Li W, Qian J, Liu X, Zhang Q, Wang L, Chen D, et al. Management of severe crush injury in a front-line tent ICU after 2008 Wenchuan earthquake in China: An experience with 32 cases. Crit Care 2009;13:R178.
7. Smith J, Greaves I. Crush injury and crush syndrome: A review. J Trauma 2003;54 Suppl 5:S226-30.
8. Devitt BM, Baker JF, Ahmed M, Menzies D, Synnott KA. Saturday night palsy or Sunday morning hangover? A case report of alcohol-induced crush syndrome. Arch Orthop Trauma Surg 2011;131:39-43.
9. Daher ED, Silva GB, Brunetta DM, Pontes LB, Bezerra GP. Rhabdomyolysis and acute renal failure after strenuous exercise and alcohol abuse: Case report and literature review. Sao Paulo Med J 2005;123:33-7.
10. Dickmann JR, Dickmann LM. An uncommonly recognized cause of rhabdomyolysis after quetiapine intoxication. Am J Emerg Med 2010;28:1060e1-2.
11. Tsuji T, Inoue S, Yamagiwa T, Morita S, Inokuchi S. A case of crush syndrome induced by the kneeling seiza position. Tokai J Exp Clin Med 2014;39:166-8.
12. Vijay MK, Vijay P, Kundu AK. Rhabdomyolysis and myogloginuric acute renal failure in the lithotomy/exaggerated lithotomy position of urogenital surgeries. Urol Ann 2011;3:147-50.
13. Dhar D, Varghese T. Crush syndrome case report and literature review. Maced J Med Sci 2010;3:319-23.
14. Gibney RTN, Sever MS, Vanholder RC. Disaster nephrology: Crush injury and beyond. Kidney Int 2014;85:1049-57.
15. Sever MS, Vanholder RC, RDRTF of ISN Work Group on Recommendations for the Management of Crush Victims in Mass Disasters. Recommendation for the management of crush victims in mass disasters. Nephrol Dial Transplant 2012;27 Suppl 1:i1-67.
 |
 |
 |
| Dr. Sumit Banerjee | Dr. Akshat Gupta | Dr. Jeshwanth N |
| How to Cite This Article: Banerjee S, Gupta A, Jeshwanth N. Acute Kidney Injury Secondary to Rhabdomyolysis: A Rare Complication of Low-Energy Trauma. Journal of Orthopaedic Case Reports 2021 January;11(1): 16-19. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com

 [box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]