 [box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
In cases of polytrauma and pelvic injuries specially motorbike accidents, testicular dislocation should be ruled out before definitive surgery.
Case Report | Volume 11 | Issue 2 | JOCR February 2021 | Page 90-94 | Varun Chouhan, Manish ladhania, Kiran Chouhan . DOI: 10.13107/jocr.2021.v11.i02.2040
Authors: Varun Chouhan[1], Manish ladhania[1], Kiran Chouhan[1]
[1]Department of Orthopaedic Surgery, Bombay Hospital, Indore, Madhya Pradesh, India.
Address of Correspondence:
Dr. Varun Chouhan,
Department of Orthopaedic Surgery, Bombay Hospital, Indore – 452 010, Madhya Pradesh, India.
E-mail: drvarunchouhan@yahoo.co.in
Abstract
Introduction: Intrapelvic testicular dislocation is rare injury with the possibility of missed or delayed diagnosis. Timely diagnosis of intrapelvic testicular dislocation can prevent iatrogenic testicular injury during surgery and its long-term sequel.
Case Report: A 30-year-old male after motorbike accident presented with a pelvic injury with intrapelvic dislocation of testis. Timely and appropriate diagnosis of injuries, specially intrapelvic dislocation of testis, required early orchidopexy and open reduction and internal fixation of the anterior column, leading to excellent outcome.
Conclusion: In cases of polytrauma and pelvic injuries specially motorbike accidents, testicular dislocation should be ruled out before definitive surgery. Adequate communication and co-ordination between orthopedic surgeon, radiologist, and urologist can lead to excellent outcomes.
Keywords: Testicular dislocation, ectopic testicular dislocation, intrapelvic dislocation of testis.
Introduction
Pelvic injuries are as a result of high energy trauma except in elderly. Motorcycle and motor vehicle accidents are the most common mechanisms. Many patients with pelvic fractures have multisystem injuries. Bladder and urethral injuries occur in 6–15% of pelvic injuries depending on the severity of the pelvic ring fracture. Testicular dislocations with these injuries are rare with few case reports available in the literature, but probably, they are under reported due to lack of awareness. Claubry, in 1818, described the first case of bilateral traumatic dislocation of the testes, which occurred in a 20-year-old soldier who was run over by a wagon wheel [1]. This case report presents a case of pelvic fracture associated with intrapelvic dislocation of the testis. The main purpose of this report is to increase awareness of these injuries in orthopedic fraternity which can prevent iatrogenic injury to testis and its surrounding structure during surgery, even missing the diagnosis of the dislocated testis can lead to disastrous sequel in the long-term.
Case Report
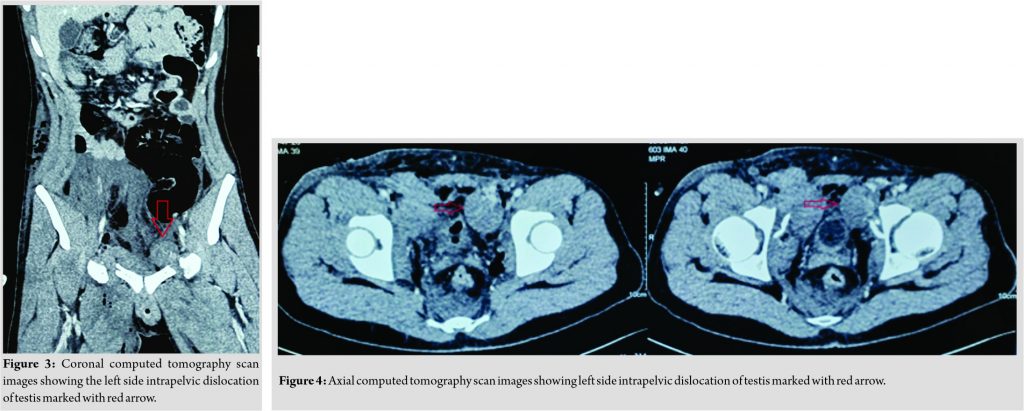
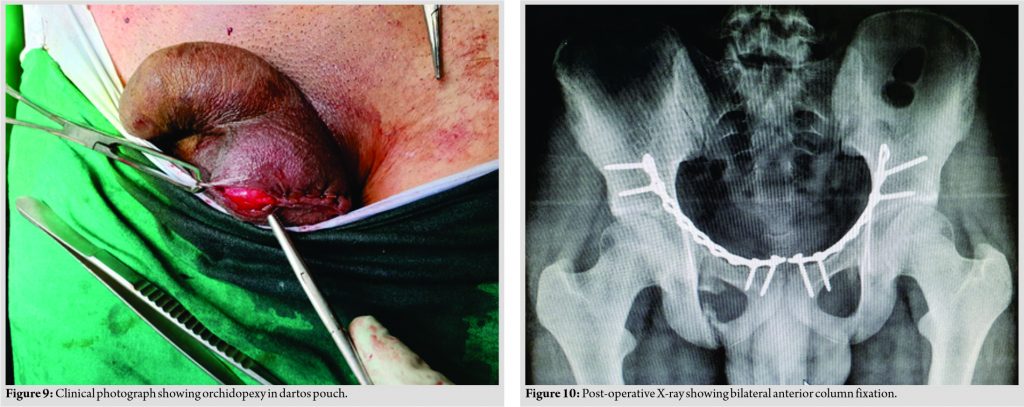
A 30-year-old male patient had road traffic accident while driving a motorbike leading to bilateral pelvis injury with the left side distal end radius fracture. The patient presented in emergency, where primary examination showed severe pain in the left wrist and pelvis. The patient was hemodynamically stable. X-ray showed bilateral superior and inferior pubic rami fractures (Fig. 1) with intra-articular fracture distal end radius. Computed tomography (CT) scan (Fig. 2, 3, 4) revealed that the patient had superior and inferior pubic rami fracture with intrapelvic dislocation of the left testis.


Discussion
Testicular dislocation is rare injuries but may be associated with many traumatic injuries, most frequently due to a motorcycle collision, and it can easily be overlooked due to the severity of other injuries [2]. In cases associated with motorcycle collisions, the force to the scrotum is likely caused by the gasoline tank striking the rider’s perineum and scrotal region due to rapid deceleration of the vehicle [3]. The dislocation may be superficial (the testis is forced into the superficial inguinal pouch) or internal (the testis is forced through the external ring into the inguinal canal or even into the abdominal cavity). Superficial inguinal pouch is the commonest reported location for a dislocated testis, and it occurs in 40–50% of the cases [4]. The possible sites with a relative frequency are as follows: Superficial inguinal – 50%, truly abdominal – 6%, pubic – 18%, penile – 8%, canalicular – 8%, acetabular – 8%, perineal – 4%, and crural – 2% [5]. The dislocation of the testis is commonly unilateral, but it can be bilateral, too, as it has been seen in about 30% of the cases [5, 6]. It is very important to distinguish between traumatic dislocation of testis and cryptorchidism. The scrotal sac is well developed in the traumatic dislocation of the testis as compared to cryptorchidism, where it is underdeveloped (Broakman’s sign) [7]. Dislocation of testis has been reported to impair spermatogenesis in post-pubertal men. The histologic changes usually appear after 4 months of dislocation. They include hyalinization and atrophy of seminiferous tubules, absence of sperm or spermatid formation, presence of germ cells, and an increase in alternative germ cells. Sakamoto et al. reported a case of recovering spermatogenesis in a patient with bilateral testicular dislocation and azoospermia after 15 years [8]. Factors that lead to the dislocation of testis are identified as a spasm of the cremasteric muscle, a wide external inguinal ring, presence of an indirect inguinal hernia, and atrophic testis [6]. “Compound dislocation” of the testis is a special category in which traumatic extrusion of the testis occurs through the skin of the scrotum. It is an extremely rare occurrence and was first described by Alyea in 1929 [9]. Diagnosis of testicular dislocation in cases of polytrauma, specially in case of pelvic injuries, can be missed due to lack of awareness of these injuries, so clinical examination of scrotum and asking complete history regarding complete decent of the testis is very important. In case of suspicion, ultrasonography can be done. Nowadays, CT scan is usually done for better understanding of pelvi-acetabular injuries, CT scan can show dislocated testis if specially looked for and treating surgeon should discuss with radiologist about the possibility of these injuries. Abdominal ultrasound and CT scan could confirm that the testicle is intact and exclude coexisting problems such as testicular rupture, torsion, or hematoma. After diagnosis urologist should be consulted; if the testis can be imaged adequately to ensure its tunical integrity and appropriate blood flow, then closed reduction is the initial treatment of choice in superficial injuries, but internal dislocation needs an open reduction of testis to anatomical location and orchidopexy with appropriate treatment of associated injuries.
Conclusion
Intrapelvic testicular dislocation in the setting of a polytrauma is rare injury which is commonly associated with motorbike accident. History, clinical examination, ultrasonography and CT scan, and adequate communication with radiologist are valuable tools for the diagnosis of testicular dislocation. Timely diagnosis of intrapelvic testicular dislocation before definitive surgery can avoid iatrogenic injury to testis and its associated structures.
Clinical Message
Intrapelvic testicular dislocations can be missed due lack of awareness of them, moreover, in association with pelvi-acetabular injuries, undiagnosed intrapelvic testicular dislocation can lead to possibility of iatrogenic injuries to testis and its associated structures during surgery. Early diagnosis, adequate planning and involving urologist during decision-making, and surgery can lead to excellent functional outcomes.
References
1. Claubry EG. Observations sur une retrocession subite des deux testicules dans I’abdomen, a la suite d’une violente compression de la partie inferieure de la paroi abdominale par une roué de charrette. J Gen Med Chir Pharm 1818;64:325-30.
2. Smith CS, Rosenbaum CS, Harris AM. Traumatic bilateral testicular dislocation associated with an anterior posterior compression fracture of the pelvis: A case report. J Surg Orthop Adv 2012;21:162-4.
3. Perera E, Bhatt S, Dogra VS. Traumatic ectopic dislocation of testis. J Clin Imaging Sci 2011;1:17.
4. Bromberg W, Wong C, Kurek S. Traumatic bilateral testicular dislocation. J Trauma 2003;54:1009-11.
5. Schwartz SL, Faerber GJ. Dislocation of the testis as a delayed presentation of scrotal trauma. Urology 1994;43:743-5.
6. Kilian CA, Paz DA, Patel SA, Austin MJ, Richman KM, Pretorius DH. False diagnosis of ruptured testes in a case of traumatic dislocation. JUM 2009;28:549-53.
7. Ihama Y, Fuke C, Miyazaki T. A two-rider motorcycle accident involving injuries around the groin area in both the driver and the passenger. Legal Med 2007;9:274-7.
8. Sakamoto H, Iwasaki S, Kushima M, Shichijo T, Ogawa Y. Traumatic bilateral testicular dislocation: A recovery of spermatogenesis by orchiopexy 15 years after the onset. Fertil Steril 2008;90:e9-11.
9. Alyea EP. Dislocation of testis. Surg Gynecol Obstet 1929;49:600.
 |
 |
 |
| Dr. Varun Chouhan | Dr. Manish ladhania | Dr. Kiran Chouhan |
| How to Cite This Article: Chouhan V, ladhania M, Chouhan K. Pelvic Fracture Associated with Intrapelvic Dislocation of Testis. Journal of Orthopaedic Case Reports 2021 February;11(2): 90-94. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com





