Homocystinuria is a rare disease that needs early identification and effective management to avoid skeletal complications such as genu valgum, pes cavus, chest wall deformities, kyphosis, and scoliosis.
Dr. Sathish Muthu,
Orthopaedic Research Group, Coimbatore, Tamil Nadu, India.
Email: sathishmuthu@orthopaedicresearchgroup.com
Introduction: Homocystinuria has a wide range of clinical presentations ranging from near normal intelligence and appearance with just lens dislocation and minimal skeletal deformities to severe mental retardation with gross skeletal deformities. In this background, we describe one such case with skeletal deformity managed comprehensively.
Case Report: A 17-year-old boy presented with complaints of deformity of the left lower limb since childhood more evident for the past 5 years along with a history of blurring of vision. On examination the pubis-heal length > crown-pubis length along with genu valgum of left lower-limb with 16 cm intermalleolar distance. He also had a superolateral subluxation of the lens in both eyes. Valgus angle was 16° on the left leg compared to 6° on the right. The diagnosis of homocystinuria was confirmed by biochemical investigations. The left side genu valgum was addressed with medial closing wedge osteotomy and fixed with distal femur locking compression plating. Lens subluxation was treated with posterior chamber intra-ocular lens surgery. He was also given medical treatment and on regular monitoring of his homocysteine levels. The patient had good functional outcome at 2-year follow-up.
Conclusion: Homocystinuria is a rare disease that needs early identification and effective management to avoid complications. Skeletal complications are common and include genu valgum, pes cavus, chest wall deformities, and skeletal deformities such as kyphosis and scoliosis. Skeletal deformities can be avoided when identified early and associated osteoporosis which is managed effectively. A holistic approach is needed in the management of such patients with inter-departmental coordination to bring quality to the life of patients with homocystinuria.
Keywords: Homocystinuria, holistic approach, skeletal deformity, deformity correction, ectopia lentis.
Homocystinuria is a rare autosomal recessive inborn error of amino-acid metabolism due to deficiency of the enzyme cystathionine beta-synthase which is needed for the normal metabolism of the homocysteine into cystathionine [1]. The disease has four cardinal clinical features namely, lens dislocation, mental retardation, skeletal abnormalities, and clotting disorder [2]. There is a wide range of clinical presentations ranging from near normal intelligence and appearance with just lens dislocation and minimal skeletal deformities to severe mental retardation with gross skeletal deformities [2, 3]. The most predominant skeletal manifestations of the disease are due to disproportionate skeletal growth resulting in pubis to heel length (PHL) greater than crown to pubis length (CPL), abnormal vertebrae, sternal deformities, genu valgum with large metaphyses, and epiphyses in the involved bones. Due to the similarities in the skeletal presentation, the disease is often confused with Marfan’s syndrome [3]. There is no literature available on the management of skeletal deformities in the case of homocystinuria. In this case report, we present a case of homocystinuria who underwent not only deformity correction but also was managed in a holistic approach to improve the quality of life of the patient addressing the entire spectrum of disease manifestations.
A 17-year-old boy presented with complaints of deformity of the left lower limb since childhood more evident for the past 5 years without any history of trauma. He also had progressive blurring of vision for the past 1 year. The patient had a delay in the development of his motor milestones with near-normal language and social milestones as per his mother.
On general examination, the patient had altered upper to lower segment ratio having the PHL > CPL along with dysmorphic facies as shown in (Fig. 1), microcornea with Bitot’s spots bilaterally, along with superolateral subluxation of both the lens. The patient was subjected to a mini-mental state examination and scored 28/30. Other system examinations were normal. The intermalleolar distance was 16 cm. All the baseline blood investigations such as blood counts, liver, and renal function tests were within normal limits. Special biochemical investigations such as serum Vitamin B12 was <50 pg/ml (Normal: 180-914 pg/ml), serum folic acid was 21.03 ng/ml (Normal: 2.3-24.8 ng/ml), and plasma total homocysteine (tHcy) was >50 μmol/L (Normal: 5.45-16.2 μmol/L). We did a scannogram of the lower limb to analyze the deformity. Valgus angle was 16° on the left compared to 6° on the right as shown in (Fig. 2). We obtained the opinions of specialists from medicine, cardiology, cardiothoracic, and ophthalmology department. DEXA scan was normal.
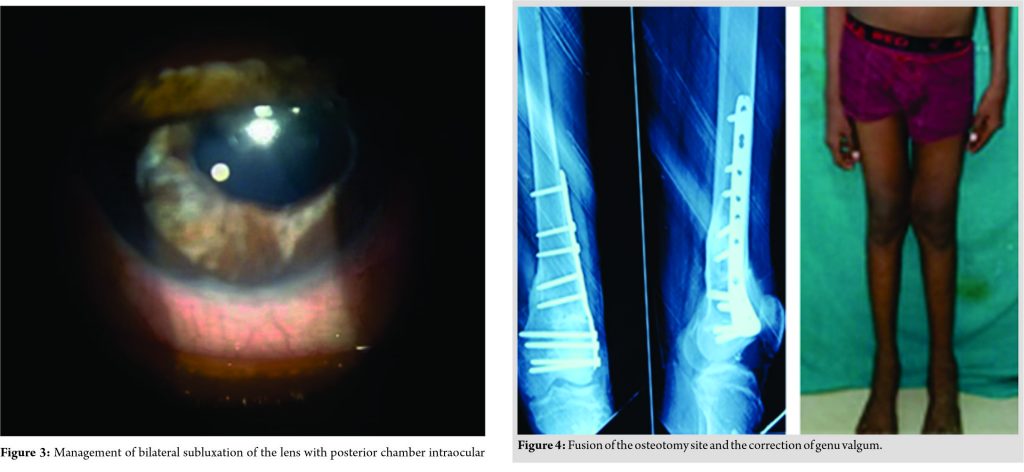
Management of bilateral subluxation of the lens was given priority and treated with posterior chamber intra ocular lens surgery, as shown in (Fig. 3). We treated the genu valgum of the left side with distal femur medial closing wedge osteotomy and fixation with distal femur locking compression plate and screws. The post-operative period was uneventful and the patient was started on non-weight bearing walking from the second post-operative day and not allowed to weight bear until 8 weeks post-operatively. The Valgus angle reduced from 16° to 4° post-operatively, as shown in (Fig. 2) and the intermalleolar distance reduced from 16 cm to 10 cm and an increase in the inter-condylar distance from none to 3 cm.
The patient was also managed medically with folic acid 0.5 mg/day, pyridoxine 50 mg/day, and reduced methionine in diet. He was responsive to pyridoxine therapy and serial monitoring of serum homocysteine was done to monitor the treatment. Additional Vitamin A deficiency management with Vitamin A 25,000 IU/week for 3 months along with Vitamin A rich diet.
The patient was serially followed up until fusion of the osteotomy is confirmed as shown in (Fig. 4) and started on full weight-bearing and the patient achieved a full range of movements and is doing well without any complications until his last follow-up at 2 years post-operatively and advised on a regular follow-up to monitor his tHcy levels periodically and for osteoporosis screening. The patient also underwent routine ophthalmology follow-up.
Homocystinuria being a rare autosomal recessive metabolic disorder has an incidence of 1-9/100,000 people worldwide [4] with the literature yet to be published on the holistic approach toward the management of skeletal deformity in them. Bone deformities occupy a major area in the spectrum of symptomatology in homocystinuria and need appropriate management to prevent expectant complications in them.
Skeletal complications are more common and include overgrowth of long bones and premature osteoporosis [5]. Moreover, this is also a preventable complication with early diagnosis and adequate treatment with good biochemical control [6]. Regular DEXA scans from adolescence for early identification of premature osteoporosis are recommended unless clinically indicated earlier [7]. Skeletal changes are not so common in pyridoxine responsive individuals [8]. Usually, there are no abnormalities at birth [8]. Genu valgum and pes cavus are the first signs of skeletal involvement [9]. Around the age of puberty, the limbs grow out of proportion to the trunk. Sometimes, chest wall deformities such as pectus excavatum or pectus carinatum, along with kyphosis or scoliosis may be present [10]. Altered facial appearance is mostly due to overcrowding of the upper row of teeth and high arched palate [11]. These features give the older patients attain a marfanoid habitus but homocystinuria can be differentiated by the presence of osteoporosis [10]. Osteoporosis is consistent in the spine and the largest review by Mudd [12], 70% of untreated patients developed spinal osteoporosis by 16 years of age. Early identification and effective treatment can reduce the risk of osteoporosis in them [7]. Osteoporosis results in the vertebral collapse and scoliosis; hence, routine DEXA scanning is recommended every 3–5 years from adolescence until warranted earlier for recurrent fractures. It is also important to check the dietary calcium intake and Vitamin D status of the individuals [7]. Operating in a patient with homocystinuria has its additional risks like the risk of venous thromboembolism (VTE) [13]. Hence, biochemical parameters, diet, and nutrition should be optimized before elective procedures can be embarked on them. The use of nitrous oxide is avoided since it increases tHcy concentration [14]. Adequate hydration is achieved with intravenous fluids. Standard VTE prophylaxis measures such as elastic stockings, pneumatic leg compression systems, and early mobilization should be followed during and after surgery. When prolonged immobilization is required low molecular weight heparin is recommended [15]. Failure to address the coronal plane malalignment such as genu valgum as in our case poses an increased risk of development of secondary changes such as early osteoarthritis and rapid deterioration of the general locomotor ability of the individual with increases susceptibility for falls and fractures.
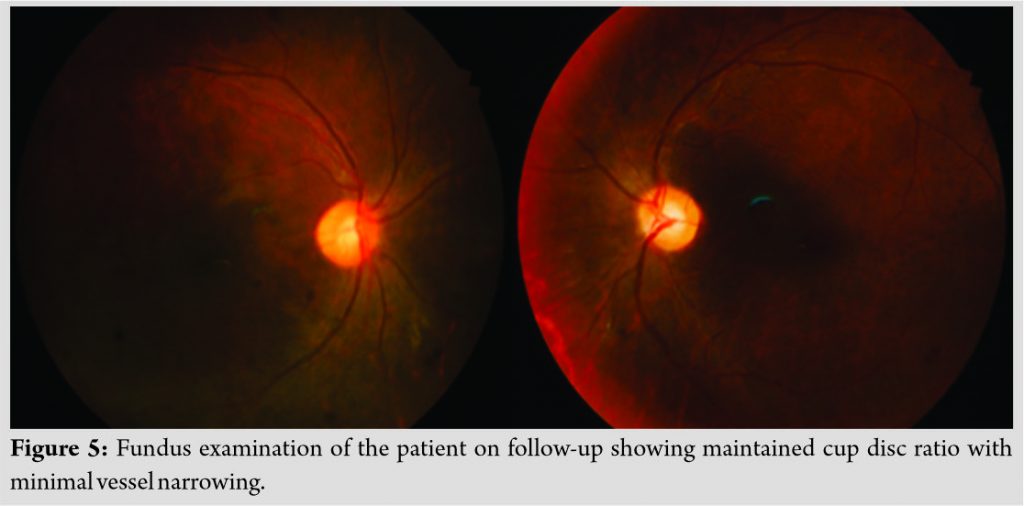
Ophthalmological monitoring needs to look out for myopia, ectopia lentis, and associated complications such as glaucoma and retinal detachment [16]. Fundus examination of the patient during final follow is given by (Fig. 5) showing maintained cup disc ratio with minimal vessel narrowing. At times, ectopia lentis may be the first and only sign of the disease. Whereas, early diagnosis and treatment with good biochemical control can prevent this complication.
Thromboembolic events are more common in untreated or poorly controlled patients [15]. It is also a preventable complication when the condition is diagnosed early and treated appropriately.
As per the guidelines by the European network and registry for homocystinurias and methylation defects (E-HOD), [17] the aim of the medical therapy is plasma tHcy <50 µmol/L in pyridoxine responsive patients and unresponsive cases tHcy <100 µmol/L. Pyridoxine is considered as the first line to achieve target tHcy levels [18] and Betaine can be considered as adjunctive therapy for patients who cannot achieve target levels of tHcy by other means [19].
Dietary treatment is considered for all patients unless target Hcy levels are achieved entirely by pyridoxine supplementation [20, 21]. Diet may be used either as a sole treatment or adjunctive therapy along with pyridoxine therapy.
Homocystinuria is a rare disease that needs early identification and effective management to avoid complications. Skeletal complications are common and include genu valgum, pes cavus, chest wall deformities, and skeletal deformities such as kyphosis and scoliosis. Skeletal deformities can be avoided when identified early and associated osteoporosis are managed effectively. A holistic approach is needed in the management of such patients with inter-departmental coordination to bring quality to the life of patients with homocystinuria.
To improve the quality of life of the patient with homocystinuria, a holistic approach to address all the manifestations of the disease is a necessary prerequisite.
References
- 1.Genetics Home Reference, Homocystinuria; 2020. Available from: https:// www.ghr.nlm.nih.gov/ condition/ homocystinuria. [Last accessed on 2020 Apr 07]. [Google Scholar]
- 2.de Franchis R, Sperandeo MP, Sebastio G, Andria G. Clinical aspects of cystathionine beta-synthase deficiency: How wide is the spectrum? The Italian collaborative study group on homocystinuria. Eur J Pediatr 1998;157 Suppl 2:S67-70. [Google Scholar]
- 3.Beals RK. Homocystinuria. A report of two cases and review of the literature. J Bone Joint Surg Am 1969;51:1564-72. [Google Scholar]
- 4.Asghar A, Ali FM. Anaesthetic management of a young patient with homocystinuria. J Coll Physicians Surg Pak 2012;22:720-2. [Google Scholar]
- 5.Brenton DP. Skeletal abnormalities in homocystinuria. Postgrad Med J 1977;53:488-94. [Google Scholar]
- 6.Cruysberg JR, Boers GH, Trijbels JM, Deutman AF. Delay in diagnosis of homocystinuria: Retrospective study of consecutive patients. BMJ 1996;313:1037-40. [Google Scholar]
- 7.Lim JS, Lee DH. Changes in bone mineral density and body composition of children with well-controlled homocystinuria caused by CBS deficiency. Osteoporos Int 2013;24:2535-8. [Google Scholar]
- 8.Brenton DP, Cusworth DC. The response of patients with cystathionine synthase deficiency to pyridoxine. In: Carson NA, Raine DN, editors. Inherited Disorders of Sulfur Metabolism. Edinburgh: Churchill Livingstone; 1971. p. 264-74. [Google Scholar]
- 9.Boers GH, Polder TW, Cruysberg JR, Schoonderwaldt HC, Peetoom JJ, van Ruyven TW, et al. Homocystinuria versus Marfan’s syndrome: The therapeutic relevance of the differential diagnosis. Neth J Med 1984;27:206-12. [Google Scholar]
- 10.Morreels CL Jr., Fletcher BD, Weilbaecher RG, Dorst JP. The roentgenographic features of homocystinuria. Radiology 1968;90:1150-8. [Google Scholar]
- 11.Brenton DP, Dow CJ, James JI, Hay RL, Wynne-Davies R. Homocystinuria and Marfan’s syndrome. A comparison. J Bone Joint Surg Br 1972;54:277-98. [Google Scholar]
- 12.Mudd SH. Hypermethioninemias of genetic and non-genetic origin: A review. Am J Med Genet C Semin Med Genet 2011;157C:3-32. [Google Scholar]
- 13.Harker LA, Slichter SJ, Scott CR, Ross R. Homocystinemia. Vascular injury and arterial thrombosis. N Engl J Med 1974;291:537-43. [Google Scholar]
- 14.Lowe S, Johnson DA, Tobias JD. Anesthetic implications of the child with homocystinuria. J Clin Anesth 1994;6:142-4. [Google Scholar]
- 15.Lutteri L, Chapelle JP, Gielen J. Homocysteine and cardiovascular risk. Rev Med Liege 1999;54:541-7 [Google Scholar]
- 16.Elkington AR, Freedman SS, Jay B, Wright P. Anterior dislocation of the lens in homocystinuria. Br J Ophthalmol 1973;57:325-9. [Google Scholar]
- 17.Morris AA, Kožich V, Santra S, Andria G, Ben-Omran TI, Chakrapani AB, et al. Guidelines for the diagnosis and management of cystathionine beta-synthase deficiency. J Inherit Metab Dis 2017;40:49-74. [Google Scholar]
- 18.Grobe H. Homocystinuria (cystathionine synthase deficiency). Results of treatment in late-diagnosed patients. Eur J Pediatr 1980;135:199-203. [Google Scholar]
- 19.Benevenga NJ. Betaine in the treatment of homocystinuria. N Engl J Med 1984;310:265-6. [Google Scholar]
- 20.American academy of pediatrics. Committee on nutrition: Special diets for infants with inborn errors of amino acid metabolism. Pediatrics 1976;57:783-92. [Google Scholar]
- 21.Kabra M. Dietary management of inborn errors of metabolism. Indian J Pediatr 2002;69:421-6. [Google Scholar]