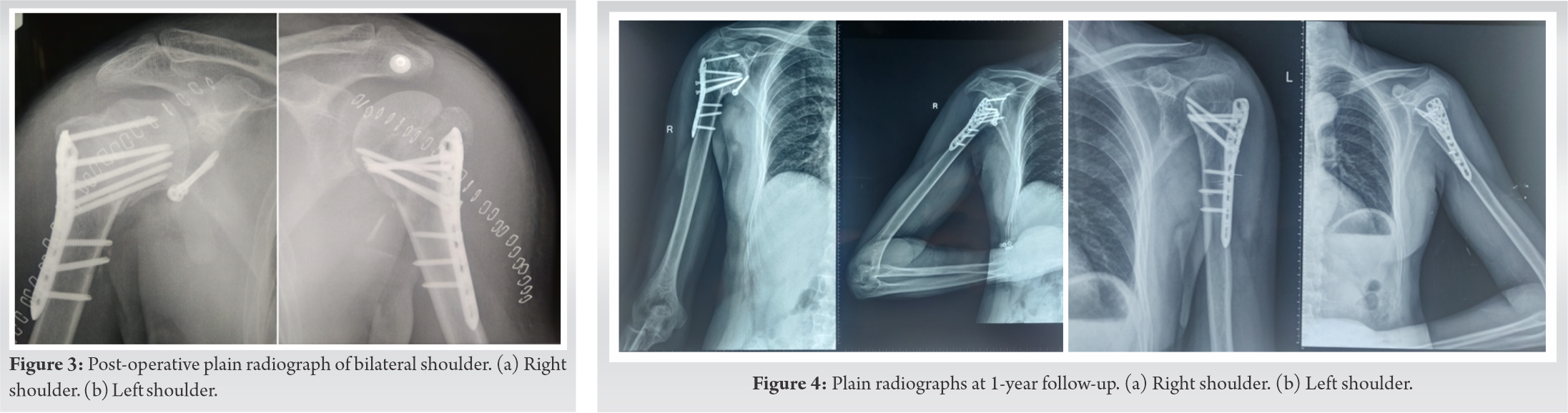
This article provides an insight on how to proceed in cases of bilateral proximal humerus fractures. Use of NCCT before operative intervention in such cases is must to rule out any prior existing lesions in the glenoid or humeral head.
Dr. Pradeep Kumar Meena,
Department of Orthopaedics, All India Institute of Medical Sciences, Rishikesh, India.
E-mail: dr.pradsms@gmail.com
Introduction: Anterior shoulder dislocation is a common presentation in orthopedic emergency but a bilateral fracture dislocation is a rare entity. Only a few cases have been reported in the literature and their management is still not clear. We present a bilateral four part fracture dislocation with Bankart lesion on right side in a 48 years old.
Case Report: A 48-year-old male presented with bilateral proximal humerus fracture with anterior shoulder dislocation following a seizure. He was managed with bilateral PHILOS and Latarjet procedure on right side for a chronic bony Bankart lesion. Superficial infection on left side was managed with debridement. After 1 year period patient had a satisfactory outcome with DASH score of 19.2.
Conclusion: Bilateral four part proximal humerus fracture with shoulder dislocation is encountered rarely. Recurrent dislocations results in chronic glenoid bones loss which needs fixation along with fracture. Addressing both sides subsequently or in a single sitting is still debatable.
Keywords: Bilateral humerus fracture, anterior dislocation, Bankart repair.
Although shoulder is the most common joint to get dislocated, bilateral fracture dislocations are less commonly seen. Most of the bilateral shoulder dislocations documented in the literature are posterior making bilateral anterior dislocation an even rarer entity [1]. Only a few cases of the same have been reported in the literature [1, 2, 3]. Even after an extensive literature search, we were unable to find even a single case of bilateral proximal humerus fracture dislocation with a bony Bankart lesion. We present an uncommon case of bilateral proximal humerus fracture with anterior shoulder dislocation with right sided bony Bankart lesion secondary to an epileptic episode.
A 48-year-old male, working as a shopkeeper, presented to our emergency department with complaints of pain and loss of movement in bilateral shoulder, following fall from the standing height. This incident was associated with an epileptic episode while he was doing routine work in his shop. On detailed history, we discovered that he was a diagnosed case of generalized tonic clonic seizure for 9 years with the past episode 3 years back and was off medication for 2 years. There was no history of diabetes, hypertension, alcohol, and smoking. A history of oral tobacco intake for the past 20 years was present. He had suffered 4 episodes of right shoulder dislocation, the most recent episode being 2 months ago.
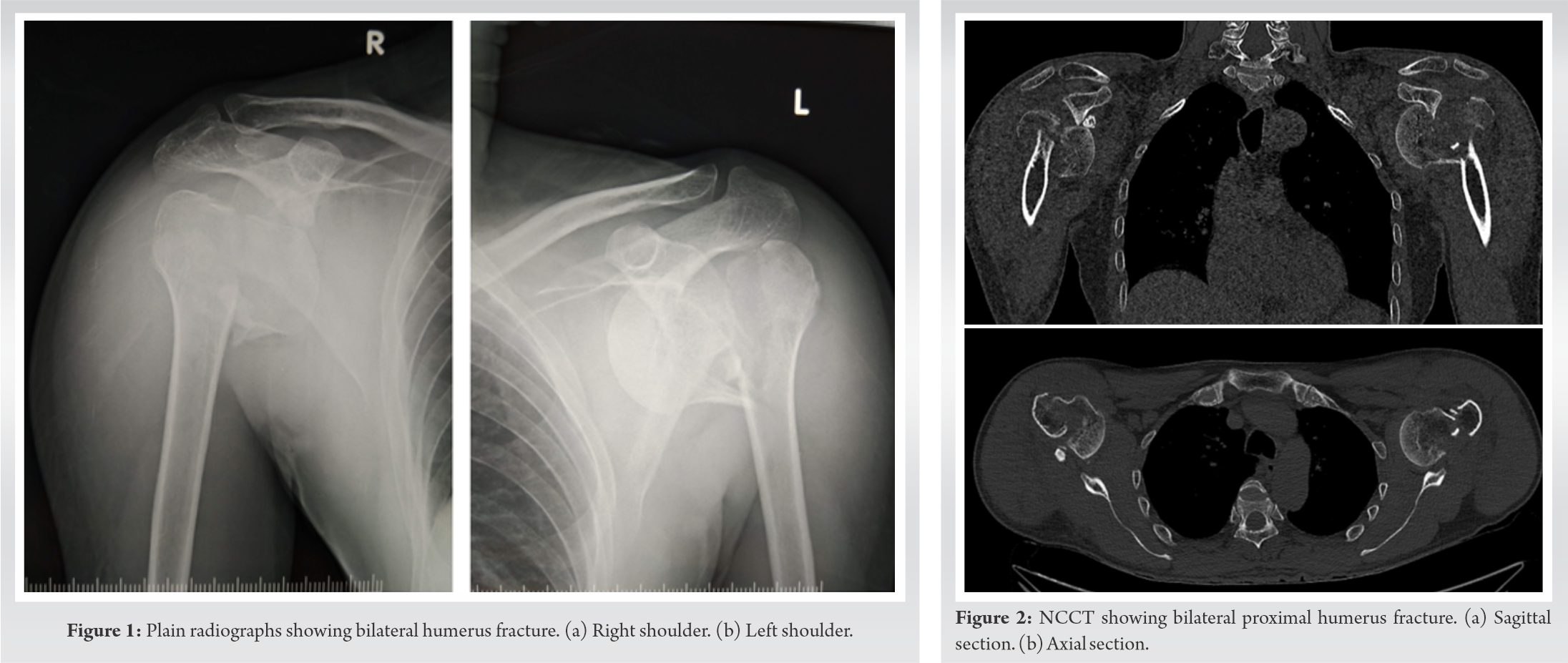
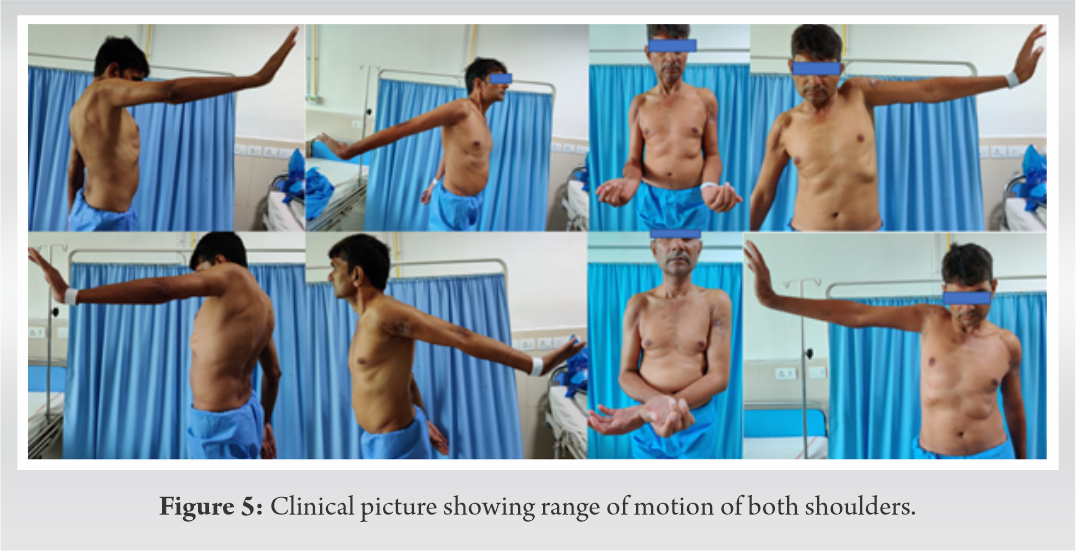
On examination, diffuse tenderness and swelling were present over bilateral shoulder with bony crepitus. No distal neurovascular deficit was noted. No other injuries were noted during the examination. Immobilization and analgesics were given in an emergency. Plain radiographs followed by computed tomography scans revealed bilateral Neer [4] IV part fracture with anterior shoulder dislocation (Figs. 1, 2). The patient was prepared for operative intervention and necessary investigations were done. Both the shoulders were operated in a single sitting. The same deltopectoral approach was used bilaterally and open reduction with Proximal Humerus Interlocking Osteosynthesis (PHILOS) plating was done (Fig. 3). The right side was operated first for no particular reason, taking approximately 3 h followed by the left side in the next 2 h. Re-draping was done and a shot of an intravenous antibiotic was given before starting the left side. Intraoperatively, a bony Bankart lesion in the right shoulder was noticed which led to persistent instability even after fixation of the proximal humerus. Henceforth, a Latarjet procedure was done for the same.
Postoperatively, the right shoulder was immobilized for 2 weeks. Pendular exercises were started on the 1st post-operative day on the left side and after 2 weeks on the right side. It was followed by a range of motion and strengthening exercises subsequently.
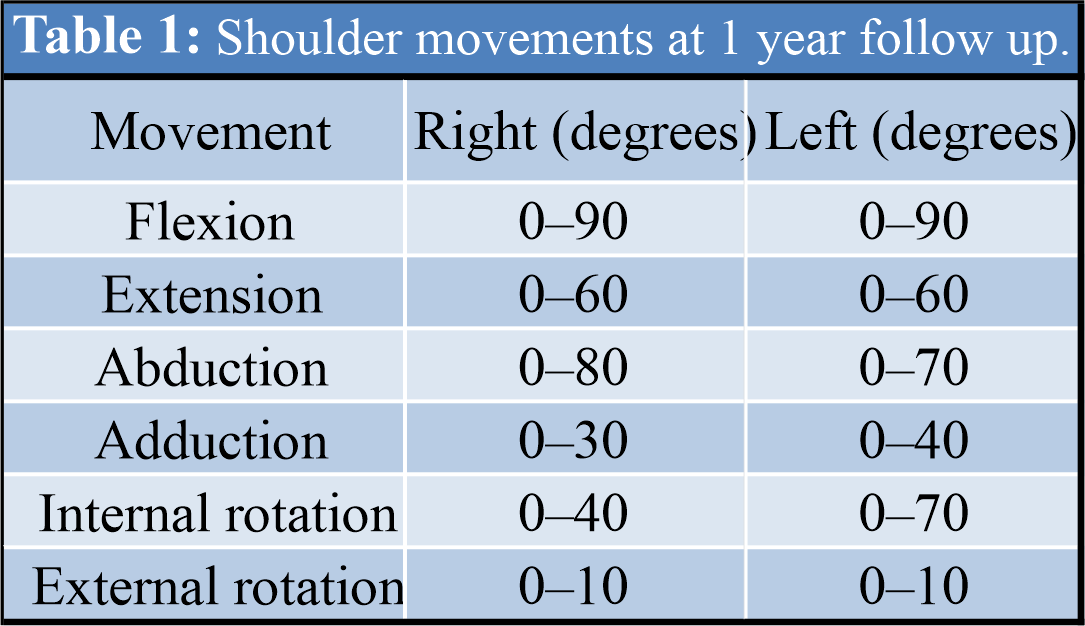
The patient developed a superficial infection on the left side resulting in serous discharge and nonhealing of the suture line. He was diagnosed with surgical site infection and underwent irrigation and debridement for the same. He was followed up at 2 weeks, 4 weeks, and then monthly thereafter. After 1 year of follow-up, the fracture has healed completely (Fig. 4) and had a satisfactory range of motion (Fig. 5) (Table 1).
He was able to carry out his activities of daily living comfortably and his Disability of the Arm, Shoulder, and Humerus of the (DASH) [5] score was calculated to be 19.2 after 1 year.
A proximal humerus fracture is seldom seen in patients younger than 50 years [6]. Bilateral proximal humerus fracture in young is an even rarer entity. Osteosynthesis with PHILOS is currently the recommended treatment of displaced two, three, and four part proximal humerus fractures in younger adults [7]. Proximal humerus fracture with associated glenoid rim fractures and labrum disruption leading to persistent instability and their management has been discussed in the literature [8] but no one has yet described the simultaneous management of bilateral proximal humerus fracture and chronic bony Bankart lesion. Glenoid bone loss, especially from the peripheral region, is common in epileptic patients. Repetitive bone to bone trauma in tonic clonic seizures and recurrent dislocations are considered to be the most significant predisposing factors [9]. Anterior dislocation being more common in epilepsy often leads to anteroinferior bone loss [9]. In case of proximal humerus fracture in such patients, these glenoid bony defects can easily be overlooked which in turn can result in intra-operative problems and post-operative instability. A detailed history must be obtained and various radiographic techniques can be applied to quantify such defects and better plan the surgery. The prolonged duration of surgery has been shown to increase the risk of surgery [10]. In our case, it took roughly 6 h to operate both sides subsequently in a single sitting. Although standard sterile precautions were taken and the antibiotic dose was repeated intraoperatively, we encountered surgical site infection on one side. However, the cause of postoperative surgical site infection is known to be multifactorial, and a single factor cannot be solely held responsible [11]. Risks of prolonged surgery might be weighed against the advantages like early mobilization and physiotherapy while deciding to fix bilateral proximal humerus fracture in a single sitting. A DASH score of <30 is considered by some as the point where the upper limb disorder does not cause problems in daily living [5]. Our patient was able to return to his job, had no sense of instability, and carry out activities of daily living without much difficulty after 3 months measuring 34.2 on the DASH evaluation scale. At the end of 1 year, he was pain free and demonstrated a score of 19.2 DASH outcome measure.
Bilateral proximal humerus fracture with shoulder dislocation is rarely encountered in clinical practice. Managing such fractures with standard osteosynthesis can produce satisfactory results. One must be wary of associated glenoid bone loss in such cases and plan patient management accordingly. Addressing both fractures in single or multiple sittings is another important issue to ponder upon before surgery.
Bilateral proximal humerus fracture dislocation is a rare emergency case presentation for orthopedic surgeons. Diagnosing and managing such cases should be after a complete and thorough investigation including NCCT of humeral head to look for the bony defects. Managing both the sides simultaneously or staged approach should be discussed further.
References
- 1.Kumar YC, Nalini KB, Maini L, Nagaraj P. Bilateral traumatic anterior dislocation of shoulder-a rare entity. J Orthop Case Rep 2013;3:23-5. [Google Scholar]
- 2.Sunku N, Kalaiah K, Marulasidappa G, Gopinath P. Bilateral anterior fracture-dislocation of shoulder joint- a rare case with delayed presentation. J Orthop Case Rep 2012;2:7-9. [Google Scholar]
- 3.Turhan E, Demirel M. Bilateral anterior glenohumeral dislocation in a horse rider: A case report and a review of the literature. Arch Orthop Trauma Surg 2008;128:79-82. [Google Scholar]
- 4.Charles S Neer I. Displaced proximal humeral fractures: Part II. treatment of three-part and four-part displacement. J Bone Joint Surg Am 1970;52:1090-103. [Google Scholar]
- 5.Williams N. Dash. Occup Med 2014;64:67-8. [Google Scholar]
- 6.Court CM Brown, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand 2001;72:365-71. [Google Scholar]
- 7.Canale S Terry JH. Campbell’s Operative Orthopaedics. 12th ed. Philapdelphia, PA: Elsevier, Mosby; 2012. p. 2484-5. [Google Scholar]
- 8.Lahav A, Rogachefsky R, Toledano B, Meinhard BP. The management of anterior dislocation of the shoulder with proximal humerus fracture, Bony Bankart lesion and associated glenoid labrum avulsion: A report of 2 cases. Am J Orthop (Belle Mead NJ) 2003;32:349-52. [Google Scholar]
- 9.Thangarajah T, Lambert S. The management of recurrent shoulder instability in patients with epilepsy: A 15-year experience. J Shoulder Elbow Surg 2015;24:1723-7. [Google Scholar]
- 10.Cheng H, Chen BP, Soleas IM, Ferko NC, Cameron CG, Hinoul P. Prolonged operative duration increases risk of surgical site infections: A systematic review. Surg Infect 2017;18:722-35. [Google Scholar]
- 11.Cheadle WG. Risk factors for surgical site infection. Surg Infect 2006;7:7-11. [Google Scholar]