This article provides an insight on how to proceed in cases of bilateral proximal humerus fractures. Use of NCCT before operative intervention in such cases is must to rule out any prior existing lesions in the glenoid or humeral head.
Dr. Sean-Tee J.M Lim,
Department of Orthopaedic Surgery, University Hospital Limerick, Ireland, St Nessan’s Road, Dooradoyle, Co. Limerick, V94 F858.
E-mail: limse@tcd.ie
Introduction: Mallet finger injury is defined by disruption of the terminal extensor tendon distal-to-distal interphalangeal (DIP) joint. While in the fingers, it is a relatively common injury, it is a rarely encountered entity when involving the thumb. Various conservative and operative treatment strategies have been reported for the management of mallet thumb with no consensus by clinicians.
Case Report: We present the case of a 27-year-old right hand dominant man with a left bony mallet thumb injury that occurred while playing hurling. Hurling is traditional Irish sport that is one of the fastest field games in the world, involving the use of a wooden Hurley and ball. Clinically, there was loss of active extension at the DIP joint of the non-dominant thumb with radiographs revealing an avulsion fracture involving more than one-third of the articular surface at the base of the distal phalanx. Closed reduction and percutaneous fixation using a single extension block Kirschner wire was performed without a transfixion wire across the DIP joint. Four months postoperatively, the patient had regained that good functional dexterity was able to return to playing hurling.
Conclusion: A single K-wire technique may be beneficial with theoretical reduction of chance of iatrogenic nail bed, bone fragment rotation, chondral damage, and bone injury. To the best of our knowledge, no previous reports of its application to bony mallet thumb have been described.
Keywords: Mallet fracture, K-wire, hurling, trauma, closed reduction
Mallet finger injuries occur when damage is sustained to the extensor tendon and may cause an avulsion fracture of the distal phalanx or a rupture of the terminal tendon of extensor mechanism. Also known as “baseball finger,” these types of injuries occur commonly during sports activities [1]. However, such injuries to the thumb are a rare entity with no general consensus on how to manage this bony mallet thumb [2]. A reasoning for the rarity of mallet thumb may be due to the thumb being shorter than the fingers and the extensor pollicis longus tendon being thicker than the extensors of the fingers [3]. If left untreated, a mallet finger can be complicated by the development of osteoarthritis at the distal interphalangeal (DIP) joint or possibly hyperextension (swan-neck) deformity at the level of the proximal interphalangeal joint [4]. Management ranges from conservative treatment with periods of immobilization by splinting to operative management with closed reduction with percutaneous pinning (CRPP) or open reduction and rigid fixation depending on the extent of injury [5]. Hurling is a contact sport native to Ireland with international reach being practiced in North America, Europe, Australia, New Zealand, South Africa, and Argentina [6]. It is played with a hurling stick and sliotar (ball) and is associated with significant morbidity, especially in regard to hand injuries due to lack of protective wear [7]. We present a case of bony mallet thumb successfully managed by percutaneous pinning with a single Kirschner (K) wire without a transfixion as not described previously.
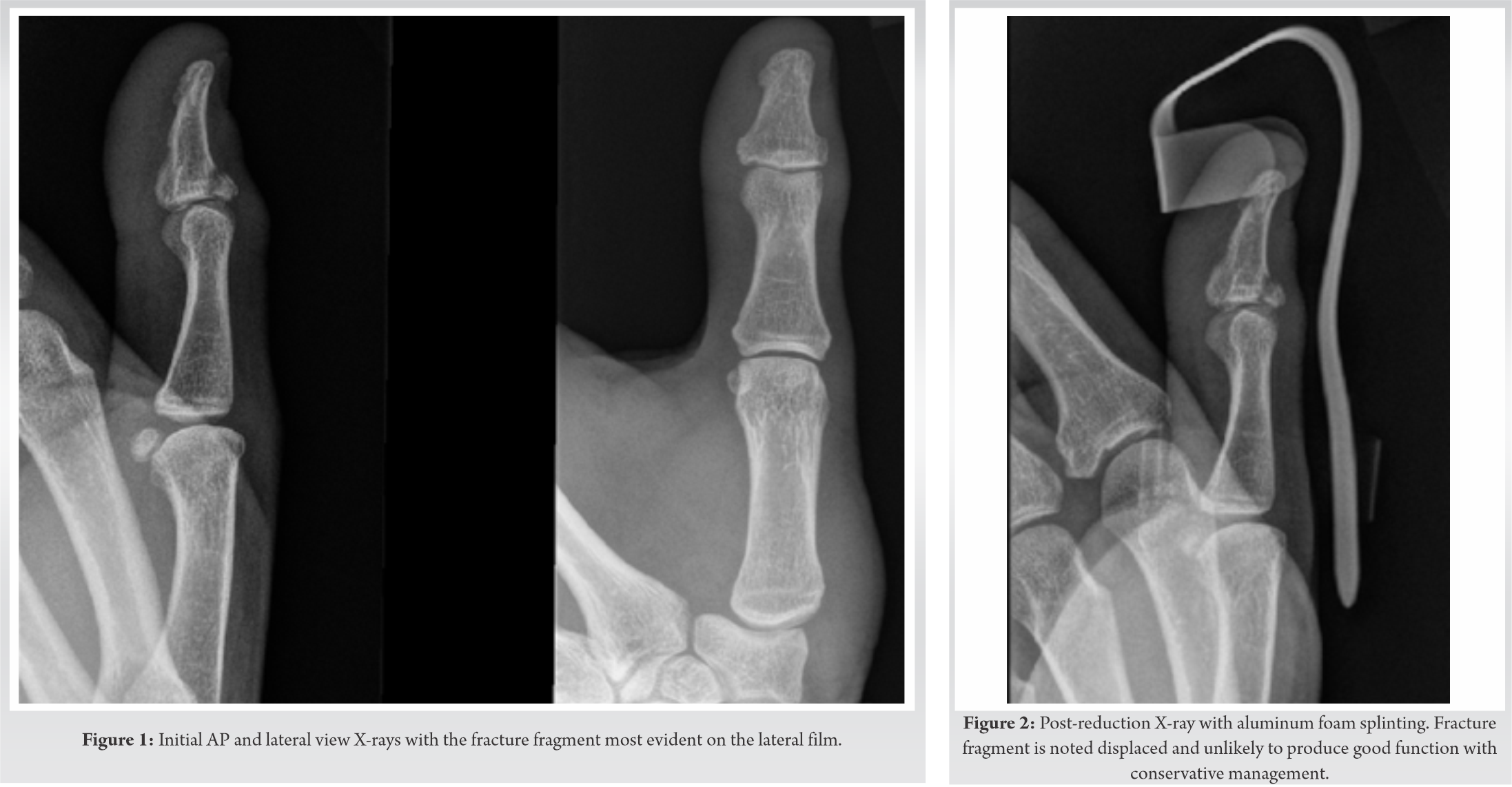
A 27-year-old right hand dominant male presented to the emergency department with a history of closed injury to the left hand. He reported 1 day prior being struck on the left thumb by a hurling stick during a match. On physical examination, the left thumb was swollen and tender at the DIP joint but otherwise neurovascularly intact. He was unable to actively extend at the IP joint but neither passive extension nor active flexion of the joint was disturbed. There was no instability of the IP joint against radial and ulnar stress. Radiographs showed an avulsion fracture at the base of the distal phalanx involving 1/3–2/3 of the articular surface, without DIP joint subluxation (Fig. 1).
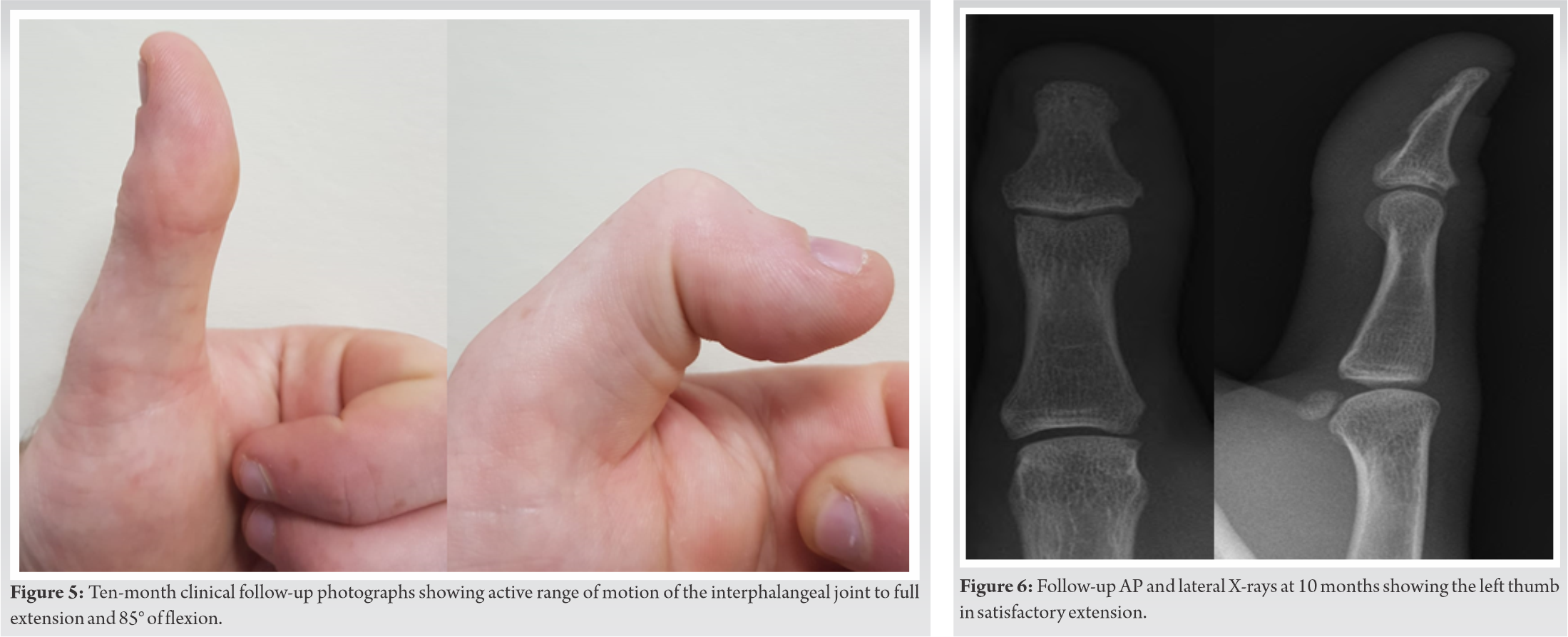
Closed reduction and splinting was undertaken, however, sufficient reduction could not be achieved on X-ray (Fig. 2). Therefore, CRPP was performed under general anesthesia. Ring tourniquet was applied for a total of 15 min. With the thumb flexed at the IP joint, a single 1.6 mm extension blocking K-wire was inserted from the dorsal side of the bony fragment to the proximal phalanx, as close to the bony fragment as possible. Satisfactory positioning was achieved clinically and radiologically with C-arm to confirm position (Fig. 3).
A volar extension splint was applied postoperatively. The follow-up visit was conducted 10 days after the surgery to evaluate the site of the pin with radiographs showing satisfactory fragment placement (Fig. 4). The single Kirschner wire was removed 4 weeks after the operation, after which active flexion of the IP joint was commenced with hand therapy. Under the guidance of experienced hand therapists, active mobilization and increased weight-bearing followed. Ten months after the repair, the patient had an active range of motion at the IP joint of 85° of flexion and 8° of extension (Fig. 5).
The range of motion on the contralateral side was 90° of flexion and 10° of extension. The patient reported no pain in the thumb with movement or at rest. According to Crawford’s evaluation criteria (Table 1), the result was excellent [8]. X-rays at 10 months post-repair showed excellent bone union without extensor lagging (Fig. 6). He reported that he was able to return to playing hurling at a competitive level 4 months after his injury and was overall very satisfied with his functional outcome.
Acute mallet thumb injuries account for small fraction of finger mallet fractures and thus have resulted in a shortage of evidence with still little guidance for the diagnosis and treatment [9]. The classification of mallet finger injuries has been described in both the Wehbe and Schneider classification, and Doyle’s classification. The fracture presented in this case would be type 1B according to the Wehbe and Schneider classification (Table 2), involving no DIP joint subluxation and 1/3–2/3 of articular surface involvement [10]. The Doyle system is based on the mechanism of injury, being categorized by the presence of laceration and the percentage of the involved joint surface (Table 3). As this injury involved 20–50% of the articular surface, it is classified as a type IV B injury according to Doyle’s classification [11]. Non-operative management has been suggested for cases with no associated fracture or no volar subluxation of the distal phalanx and generally involves immobilization of the joint in extension for at least 6–8 weeks [12]. A study by Groebli et al. reported that conservative treatment with splinting is preferred over surgery in cases of delayed presentation (>15 days) [13]. One of the main drawbacks with conservative management that has been noted is poor patient compliance [14]. For mallet finger injuries, surgeons traditionally recommended surgery if there was involvement of more than one-third of the DIP joint articular surface and those with subluxation or displacement [13]. Many different types of operative fixation have been described for mallet type injuries including open reduction, hook plate, screws, pull-through wires, tension band fixation, compression fixation pins, and the extension block technique [3]. A retrospective study by Oflazoglu et al. comparing 24 mallet fractures of the thumb and 392 mallet fractures of other digits concluded that mallet fractures of the thumb presented for medical attention sooner, had smaller fragment displacement and less articular involvement [15]. While the fracture fragments may be smaller and involve less articular surface, they often present early like in the case described, therefore, benefiting from operative management. The most common method of CRPP for mallet injuries is by the use of two wires as described by Ishiguro et al. [16]. In this case, we used a single blocking K-wire without use of trans-DIP fixation to good effect. Additional transfixion K-wires used to fix the DIP joint may cause iatrogenic nail bed injury, bone fragment rotation, chondral damage, or osteoarthritis. Furthermore, the need for prolonged immobilization may cause flexion contracture of the DIP joint [14]. The thumb contributes approximately 40% of overall hand function, therefore, it is paramount to cause as little iatrogenic damage as possible [17]. In our cause, an athletic male presented 1 day post-bony mallet thumb injury over one-third of the articulating surface, therefore, would benefit from minimally invasive surgical fixation. For a larger fracture fragment, a multiple K-wire technique may have been more appropriate for repair.
We encountered a rare case of bony mallet thumb that we repaired using a single extension blocking K-wire without a transfixion wire with an excellent functional outcome. Future prospective and randomized studies are justified to confirm the efficacy of this technique for bony mallet thumb injuries.
Mallet fracture pattern of the thumb remains a rare clinical entity that often benefits from operative fixation. For smaller fracture fragments, a single extension blocking K-wire has the ability to produce excellent clinical outcomes.
References
- 1.Alla SR, Deal ND, Dempsey IJ. Current concepts: Mallet finger. Hand (NY) 2014;9:138-44. [Google Scholar]
- 2.Din KM, Meggitt BF. Mallet thumb. J Bone Joint Surg Br 1983;65:606-7. [Google Scholar]
- 3.Nishimura R, Matsuura S, Miyawaki T, Uchida M. Bony mallet thumb. Hand Surg 2013;18:107-9. [Google Scholar]
- 4.Rockwell WB, Butler PN, Byrne BA. Extensor tendon: Anatomy, injury, and reconstruction. Plast Reconstr Surg 2000;106:1592-603; quiz 1604, 1673. [Google Scholar]
- 5.Lamaris GA, Matthew MK. The diagnosis and management of mallet finger injuries. Hand (NY) 2017;12:223-8. [Google Scholar]
- 6.Falvey E, McCrory P, Crowley B, Kelleher A, Eustace J, Shanahan F, et al. Risk factors for hand injury in hurling: A cross-sectional study. BMJ Open 2013;3:e002634. [Google Scholar]
- 7.Kiely PD, Ashraff M, O’Grady P, Dawson MJ, O’Beirne JG. Hurling-related hand injuries. Injury 2003;34:561-3. [Google Scholar]
- 8.Crawford GP. The molded polythene splint for mallet finger deformities. J Hand Surg 1984;9:231-7. [Google Scholar]
- 9.Arvanitakis M, Calcagni M, Giesen T. Closed mallet thumb injury treated surgically: A case report. Case Reports Plast Surg Hand Surg 2017;4:27-9. [Google Scholar]
- 10.Wehbe MA, Schneider LH. Mallet fractures. J Bone Joint Surg Am 1984;66:658-69. [Google Scholar]
- 11.Vedder NB. Operative hand surgery, 4th edition, Volumes 1 and 2. Ann Surg 1999;230:825-5. [Google Scholar]
- 12.Bloom JM, Khouri JS, Hammert WC. Current concepts in the evaluation and treatment of mallet finger injury. Plast Reconstr Surg 2013;132:560e-6. [Google Scholar]
- 13.Lin JS, Samora JB. Surgical and nonsurgical management of mallet finger: A systematic review. J Hand Surg Am 2018;43:146-63.e2. [Google Scholar]
- 14.Pratt DR, Bunnell S, Howard LD Jr. Mallet finger; classification and methods of treatment. Am J Surg 1957;93:573-8; discussion, 578-9. [Google Scholar]
- 15.Oflazoglu K, Moradi A, Braun Y, Ring D, Chen NC, Eberlin KR. Mallet fractures of the thumb compared with mallet fractures of the fingers. Hand (NY) 2017;12:277-82. [Google Scholar]
- 16.Ishiguro T, Itoh Y, Yabe Y, Hashizume N. Extension block with Kirschner wire for fracture dislocation of the distal interphalangeal joint. Tech Hand Up Extrem Surg 1997;1:95-102. [Google Scholar]
- 17.Emerson ET, Krizek TJ, Greenwald DP. Anatomy, physiology, and functional restoration of the thumb. Ann Plast Surg 1996;36:180-91. [Google Scholar]