This article shows a reproducible novel reconstruction technique for chronic triceps tendon injury with excellent results.
Dr. Natalie Holmes,
Orthopaedic Registrar, William Harvey Hospital.
E-mail: n.holmes@doctors.org.uk
Introduction: Triceps tendon injuries are rare and often caused by direct trauma to the arm. There are no clear guidelines on the management of these and typically partial tears are treated conservatively whilst full thickness tears are treated with primary surgical repair. We aim to review the literature on the methods for triceps repair and propose a novel surgical technique.
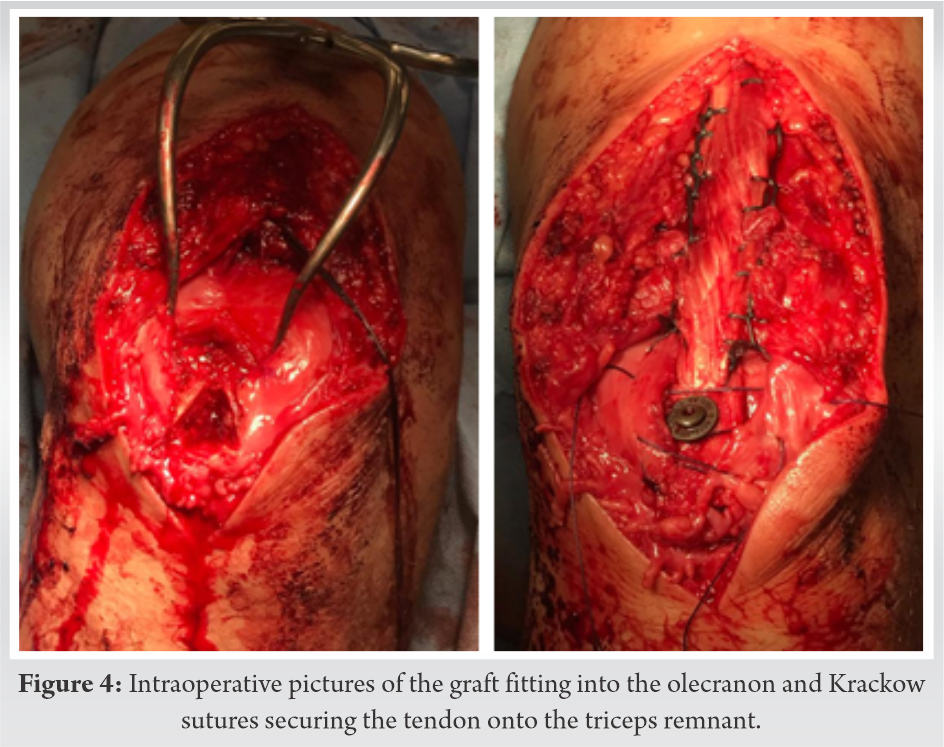
Methods: A “Medline” and “Embase” literature search of titles and abstracts combining “triceps brachii muscle,” “reconstruct/ed” or “reconstruction” alongside “reconstructive surgical procedures,” and further cross referenced with “repair/s/ed.” Excluded those related to brachial plexus injuries or general elbow trauma and removing duplicate results. 32 English results within 10 years were relevant and reviewed. Results: A 50-year-old gentleman with a 4-month-old full thickness triceps tear was repaired with a novel surgical technique of using an Achilles bone-tendon allograft fashioned into a “shark-fin” pyramidal shape and secured to the proximal ulnar in a lock and key type construct. The tendon was secured to the triceps remnant using a Krackow stitch. Complete radiological and clinical recovery was made by 18 months postoperatively with return to full physical activity. The literature review concluded no consensus in the method of treatment for delayed triceps reconstruction.
Conclusion: The use of the bone-tendon allograft specifically shaped to fit congruently into an olecranon osteotomy site allows for direct bone-to-bone healing has not previously been mentioned in the literature. Results have been encouraging and the technique described is easily reproducible.
Keywords: Triceps rupture, delayed, reconstruction, achilles allograft, surgical technique, literature review.
Triceps brachii has three muscle bellies; long head, medial head; and lateral heads all of which converge into the triceps tendon inserting onto the olecranon. Triceps tendon injuries are rare accounting for <1% of all tendinous injuries and classically occurring in the 3–5th decades of life. Typically affecting the distal insertion site they are most commonly sustained following direct trauma to the arm or a fall on an outstretched arm with the contracted triceps muscle encountering an acute deceleration force [4]. There are, however, non-traumatic causes that can predispose an individual to triceps tendon injury including local factors such as the use of topical steroids or “wear and tear” from degenerative arthritis as well as systemic factors including renal disease and diabetes mellitus [13] [17]. Inability to fully extend the elbow, ecchymosis, swelling, and pain on resisted extension are clinical signs of a triceps injury. A palpable defect proximal to the olecranon can sometimes be felt; however, this can be masked by swelling in the acute phase [17]. Often radiographic findings are minimal and mostly demonstrate soft-tissue swelling or bony avulsions near the olecranon. Ultrasound has a role in the acute setting while an Magnetic Resonance Imaging scan (MRI) can demonstrate the extent of the tear allowing accurate operative management. Unfortunately, due to the rarity and lack of reports of these injuries, there is no clear guidance on their management nor post-operative care and rehabilitation [7]. Typically, partial tears are treated nonoperatively with physiotherapy and avoiding resisted extension. Acute full thickness tears are often surgically repaired with various techniques including the use of sutures or anchors whilst chronic tears, frequently require reconstruction with a graft [2, 3]. Due to the variety in both the types of tears and the repair techniques, it is difficult to determine the superiority of any one technique over the other [11]. We present the case of a 50-year-old male who following a traumatic tear of the triceps tendon, underwent delayed surgical reconstruction using an Achilles bone-tendon allograft.
A fit and well 50-year-old gentleman presented to the hospital Emergency Department (ED) with the right elbow swelling and pain on extension. The patient had sustained trauma to the limb in question 4 weeks prior after falling from a push bike and landing on an outstretched hand. He presented with moderate non-tender swelling palpable directly overlying the elbow with pain on resisted extension.
Initial plain X-rays demonstrated significant soft-tissue swelling with no acute bony injury. An MRI performed 8 weeks after the injury confirmed the diagnosis of a distal triceps tear. The tear showed significant retraction and involved both the superficial and deep fibers (Fig. 1a-c).

Four months after the initial presentation, the patient underwent a delayed reconstruction of the triceps tendon using an Achilles tendon-bone allograft (AtbA). A general anesthetic was used and the patient was positioned in the lateral decubitus position with the right arm extended over an L-bar. A posterior approach involving a midline incision allowed good visualization of a retracted and scarred superficial triceps tendon. The central triceps tendon was also ruptured and retracted. The triceps tendon was fully exposed, refreshed, and mobilized highlighting a 3 cm defect in 30° of flexion.
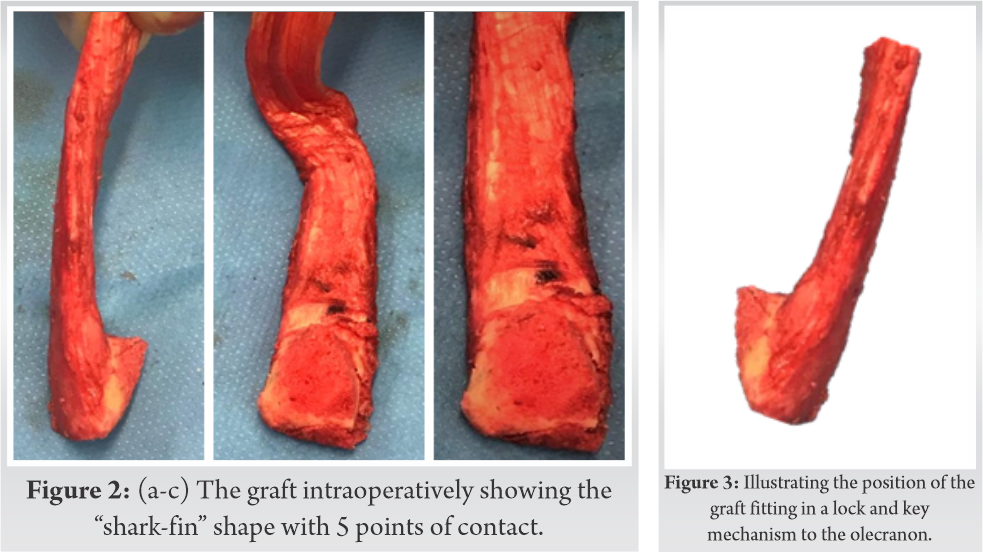
The calcaneum of the AtbA was prepared and a two-plane chevron osteotomy of the olecranon was created. (Fig. 2a-c) The bone of the allograft was shaped into pyramidal shark-fin shape to fit the olecranon osteotomy in a “lock and key” style (Fig. 3). The Achilles tendon of the AtbA graft was secured proximally with a Number 5 Braided Non-Absorbable suture using a continuous interlocking Krackow technique and distally to the remnants of the triceps. A 4.5 mm cannulated screw was used to secure the graft to the osteotomized olecranon (Fig. 4a, b). Fixation was stable in full flexion and following closure was placed in a front plaster-of-Paris slab in 30° of flexion for 2 weeks with no active elbow extension for 4 weeks.
The patient made a good recovery and 2 weeks postoperatively he was able to flex actively up to 90˚ with radiographs indicating the fixation was holding. He was placed in a hinged elbow brace allowing full passive extension but limited flexion to 90˚ for a further 4 weeks.
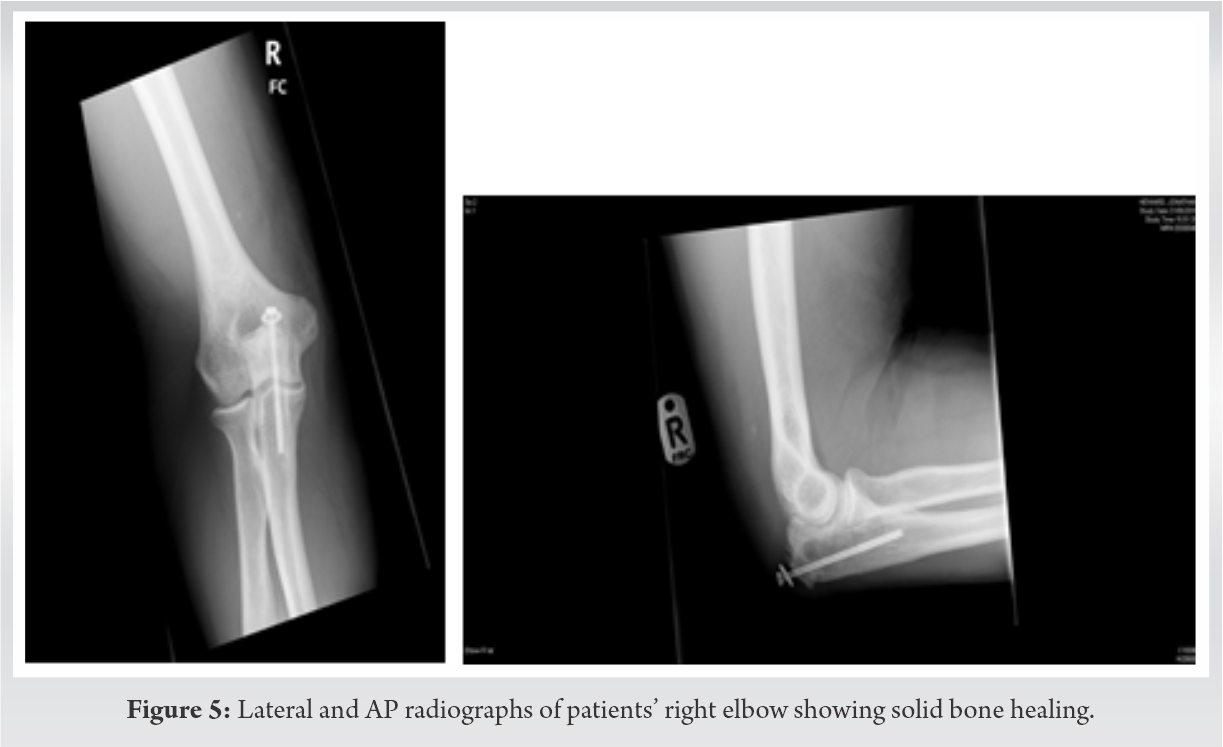
The patient continued to improve and his range of movement was gradually increased over the following 6 months. 3 months postoperatively he started gentle physiotherapy. 18 months post-reconstruction, our patient had made a full recovery. He returned to the gym, lifting 30 kg weights and boxing although he had not yet returned to judo. He regained a full range of pain free movement at the elbow with flexion ranging from 0˚ to 145˚. Clinically, the elbow was stable and radiographs showed solid healing of the bone fragments (Fig. 5a, 5b).
There are three potential sites of triceps injury, the muscle belly (proximal), the musculotendinous junction or the osseous tendon junction (distally) [10], with the latter being most common [8]. At present, there is no established standardized treatment protocol for triceps injuries. Partial tears are often managed conservatively, taking into consideration various factors including patient’s baseline functional status and pain; however, if these conservative measures fail, then surgery is considered [1, 4]. Complete tendon ruptures are often surgically repaired at the earliest opportunity. With delayed repairs, scarring, and retraction of the tendon makes primary repair difficult; therefore, in such cases, reconstruction is recommended [7, 11].
Primary surgical repair involves locking a non-absorbable suture along the triceps tendon and securing it directly through a transosseous fixation to the olecranon [11]. Yeh et al. described this suture anchor technique using 2 suture anchors placed in the triceps anatomical footprint on the ulna with mattress sutures from each anchor. These fiber-wire sutures are then passed in a Krackow type locking whipstitch up each side of the tendon [19]. The transosseous cruciate repair is the most commonly described technique in the literature fiber-wire locking Krackow whipstitch is placed through the end of the triceps tendon and up the lateral and medial sides. Two transosseous drill holes are placed in the proximal olecranon and a suture anchor is placed in each. These sutures are passed through the distal tendon in a horizontal mattress stitch. These stitches and the Krackow sutures are tied and secured to two anchors placed on the ulna footprint. Mica et al. (2018) looked at the anchor technique for triceps tendon repairs concluding that at 1-year postoperatively, peak strength of the patients to be approximately 80% of their baseline with endurance returning to 99%. They evaluated on average there was 10 of extension loss on the operative side when compared to non-operative [5]. Petre et al. showed that for distal triceps avulsions, fortification using tendon grafts (in cadaver models) improve tendon strength twofold, compared to direct repairs alone [12]. Similar to our use of an AtbA, there are cases which have used grafts of palmaris longus [16], rotational anconeus flaps, and semitendinosus to augment the primary repair [7]. All literature suggests that operative repair from a complete rupture should be performed within 2 weeks of the injury for the best results. Dimock et al. [6] described a Triceps pulley-pullover technique involving identification of the triceps tendon footprint and placing 2 double stranded suture anchors at the proximal 1/3 of this 15 mm apart. Sutures are passed from the radial side, deep to superficial through the tendon. A1-C1 forming a loop and is tied off. The anterior triceps is pulled down and the remaining strands form a Krackow stitch. A second-row anchor is used similar to the rotator cuff anchor inserted into on the dorsal side of the ulna at in the midline. Dimock reports this as a strong, anatomical reattachment with the pulley aiding tension on the tendon. The second row increases the contact area for bone to tendon healing [6]. Scheiderer et al. [15] described a V-shaped triceps tendon repair with a unicortical button fixation on cadavers. They compared the transosseous cruciate technique to the knot-less suture bride and V-shaped technique. The V-shaped technique and the knot-lee suture provided anatomical footprint coverage much better than the transosseous cruciate technique of repair. [15] In a case report by Yazdi et al. 2012 [18] the V-Y-plasty involved incising an inverted V into the triceps muscle tendon at the medal and lateral heads of the triceps. These tendons are reattached to its origin at 70 of elbow flexion using an anchor suture with fiber-wire sutures being passed through bone tunnels created at the proximal olecranon [18]. Knotless repair was studied in cadavers with 2 braded sutures woven through the central triceps tendon and is passed through the distal tendon. 2 parallel bone tunnels created in the olecranon, 3 strands of the sutures are passed through these tunnels, and the 4 strands are secured to the anchor placed on the dorsal olecranon.
Reconstruction of a ruptured triceps is most often performed with an anconeus flap whereby a lateral triceps flap is lifted from the ulna and mobilized over the olecranon before being reattached to the extensor mechanism at 30 of flexion. Results from Sanchez-Sotelo [14] showed full range of movement by 49 months. Achilles augmentation has been used when there is a large deficit or when the injury has resulted in devitalization of anconeus. Cadaver study by Petre et al. 2011 [12] showed that augmentation with the Achilles allograft resulted in a stronger, stiffer repair with the ability to absorb more energy when compared to a primary repair [12]. This study was performed using the calcaneal bone and a V shaped osteotomy with screw fixation and the proximal tendon allograft was attached to triceps muscle and tendon remnant with similar outcomes to that of aconeuous flap. Reconstruction using semitendinosus graft involves passing the graft through a hole in the tip of the olecranon. The proximal and distal part of the muscles is sutured, and they are then immobilized at 90µ˚ of flexion for 6 weeks to allow healing. Described by Gupta in 2017, the paper describes these patients participating in active exercises at 6 weeks and back to full strength at 6 months [7]. Both Yeh and Sanchez-Solelo [14, 20] used Achilles allograft in triceps injuries when there is a small defect and using the tendon to overly the distal biceps. The technique involved passing a suture through distal triceps tendon and creating cross tunnels in the proximal ulna. Further sutures were woven through the tendon and then passed through the bone tunnels. The calcaneum from the Achilles allograft is removed unless there is a defect identified in the olecranon. When there is a larger defect in the triceps Yeh continued to recommend the use of Achilles allograft in a bridging technique securing the distal Achilles to the proximal ulna with sutures. This study by Yeh et al. [19] was the largest study described using 27 cadaver elbows with random allocation into one of three repair techniques (transosseous cruciate, anchor and anatomical repair) after artificially creating a distal triceps tendon injury. Results suggested that an anatomical repair underwent the least amount of distraction and displacement at the repair site when subjected to load and compared to other repair techniques [14, 20]. Singh et al. 2012 [18] used the extensor carpi radialis longus (ECRL) and palmaris longus (PL) tendons to repair chronic triceps insufficiency. The ECRL tendon is released from its site of insertion and pulled through a proximal incision while the PL tendon was released at the level of the first wrist crease and pulled through a proximal incision. The two grafts were sutured together to create a double stranded graft. A drill hole is created through the olecranon and the double stranded graft is pulled through the bone tunnel. The graft is brought together proximally and the 4 strands are sutured as a single unit. The benefits of using an AbtA includes its accessibility, secure fixation, the ability to mobilize early postoperatively and potential to return to normal function. Other ligamentous grafts are reportedly weaker and more at risk of atrophy, although muscle strength is good by 5 years. Reconstruction often discusses the use of a graft to repair a defect weaving the graft through the distal triceps remnant and attaching this, through an anchor to the olecranon. All the literature suggests that the best outcome is that of an acute repair with greater approximation of the triceps tendon to the original footprint resulting in better restoration of strength and function. A repair of chronic insufficiency has multiple techniques described with no clear surgical technique identified. Most often the anconeus technique is used for small deficits while Achilles tendon allografts are used to bridge larger deficits. In our case, we used an Achilles bone-tendon allograft to optimize healing of the triceps tendon. By securing the allograft to an osteotomized olecranon in a “lock and key” mechanism, we have enabled maximum bone to bone healing with 5 planes of contact to the native bone. This is known to have both rapid and predictable outcomes when compared to tendon-bone healing. The bone fragment aids in the fixation stability and the technique used in this case meant the screw fixation was not altogether necessary but further added to the overall construct [9].
We report the use of AbtA to optimize the delayed repair of complete triceps tendon rupture. By creating a “lock and key” construct to secure the allograft to an osteotomized olecranon it allowed bone to bone healing further enhancing the technique. Triceps tendon injuries are notoriously missed at first presentation. The technique we have used for this patient is easily reproducible with good overall results 2 years after the surgery. The allograft is easily accessible and does not increase the morbidity in the donor site. It has a wide proximal aponeurosis ideal for quality fixation to the native residual tendon/muscle.
Our patient was able to regain full and pain free range of motion at the elbow thus enabling him to return to his daily routines. Furthermore, as evidenced by post-operative radiographic imaging, the bone-tendon allograft demonstrated good integration and healing.
This study introduces a novel new technique of reconstructing chronic triceps tendon injury with good results at 2 years. It is an easily reproducible technique and would benefit from a larger study.
References
- 1.Anzel SH, Covey KW, Weiner AD, Lipscomb PR. Disruption of muscles and tendons: An analysis of 1014 cases. Surgery 1959;45:406-14. [Google Scholar]
- 2.Aunon-Martin I, Prada-Caizares A, Jimenez-Diaz V, Vidal-Bujanda C. Treatment of a complex distal triceps tendon rupture with a new technique: A case report. Arch Trauma Res 2016;5:e32221. [Google Scholar]
- 3.Bennett JB, Mehlhoff TL. Triceps tendon repair. J Hand Surg 2015;40:1677-83. [Google Scholar]
- 4.Bunshah JJ, Raghuwanshi S, Sharma D, Pandita A. Triceps tendon rupture: An uncommon orthopaedic condition. BMJ Case Rep 2015;2015:bcr2014206446. [Google Scholar]
- 5.Conti-Mica M, Van-Riet R. Triceps tendon Repair. JBJS Essent Surg Tech 2018;8:e4. [Google Scholar]
- 6.Dimock R, Kontoghiorghe C, Considhere P, Salamat S, Imam MA, Narvani AA. Triceps pulley-pullover technique. Arthrosc Tech J 2018;8:e85-91. [Google Scholar]
- 7.Gupta RK, Soni A, Malhotra A, Masih GD. Triceps tendon reconstruction using autologous semitendinosis graft in professional kabaddi player-a rare case report. J Clin Orthop Trauma 2017;8 Suppl 1:S38-40. [Google Scholar]
- 8.Keener J, Sehti P. Distal triceps tendon injuries. Hand Clin J 2015;31:641-50. [Google Scholar]
- 9.Lui PPY, Zhang P, Chan KM, Qin L. Biology and augmentation of tendon-bone insertion repair. J Orthop Surg Res 2010;5:59. [Google Scholar]
- 10.McMaster PE. Tendon and muscle ruptures: Clinical and experimental studies on causes and locations of subcutaneous ruptures. J Bone Joint Surg Am 1933;15:705-22. [Google Scholar]
- 11.Paniago AF, Storti TM, Faria RS, Morais DC, Souza MP. Reconstruction of chronic tearing of the distal triceps using the double-row configuration: Technical note. Rev Bras Ortop 2015;50:596-600. [Google Scholar]
- 12.Petre BM, Grutter PW, Rose DM, Belkoff SM, McFarland EG, Petersen SA. Triceps tendons: A biomechanical comparison of intact and repaired strength. J Shoulder Elbow Surg 2011;20:213-8. [Google Scholar]
- 13.Pina A, Garcia I, Sabater M. Traumatic avulsion of the triceps brachii. J Orthop Trauma 2002;16:273-6. [Google Scholar]
- 14.Sanchez-Sotelo J, Morrey BF. Surgical techniques for reconstruction of chronic insufficiency of the triceps: Rotation flap using anconeus and tendo Achilles allograft. J Bone Joint Surg 2002;84:1116-20. [Google Scholar]
- 15.Scheiderer B, Imhoff FB, Morikawa D, Lacheta L, Obopilwe E, Cote MP, et al. The V-shaped distal triceps tendon repair: A comparative biomechanical analysis. Am J Sports Med 2018;46:1952-8. [Google Scholar]
- 16.Scola J. Triceps tendon reconstruction using palmaris longus autograft. Orthop Online 2013;36:e117-20. [Google Scholar]
- 17.Sharma P, Vijayargiya M, Tandon S, Gaur S. Triceps tendon avulsion: A rare injury. Ethiop J Health Sci 2014;24:97-9. [Google Scholar]
- 18.Shuttlewood K., Beazley J, Smith C. Distal triceps injuries (including snapping triceps): A systematic review of the literature. World J Orthop 2017;8:507-13. [Google Scholar]
- 19.Yazdi H, Qomashi I, Eloseni M. Neglected triceps tendon avulsion: Case report, literature review and a new repair method. Am J Orthop 2012;41:e96. [Google Scholar]
- 20.Yeh PC, Stephens KT, Solovyova O, Obopilwe E, Smart LR, Mazzocca AD, et al. The distal triceps tendon footprint and a biomechanical analysis of 3 repair techniques. Am J Sports Med 2010;38:1025-33. [Google Scholar]









