Early diagnosis and management of humerus fractures with brachial artery thrombosis helps in getting better outcome with less complications.
Dr. Prasanna Kumar G S,
Department of Orthopaedics, Grant Government Medical College, Mumbai, Maharashtra, India.,
E-mail: prasannakumargs5@gmail.com
Introduction: The humerus fractures can present as isolated or associated with other injuries and these fractures can be associated with both primary and secondary iatrogenic or traumatic neurovascular injuries. The timely management of these injuries helps in preventing catastrophic consequences.
Case Presentation: Two cases of humerus fractures were presented with brachial artery thrombosis. First case is 56-year-old female with distal humerus fracture and second is 32-year-old female with humerus shaft fracture. Both the patients had feeble pulse at the time of presentation. Urgent CT angiography of the upper limb was performed and vascular surgeon intervention was taken. First case showed complete non opacification of distal brachial artery due to thrombosis, which was managed with bicolumnar plating with embolectomy. The second case of humerus shaft fracture showed non contrast opacification at the fracture, which was managed with intramedullary nailing with removal of the bony fragment impinging on the artery and embolectomy. Postoperatively, both the patients are having good functional and radiological outcome without any complications.
Conclusion: Proper early clinical evaluation for vascular deficits helps to prevent the delayed diagnosis and radiological investigations helps to identify the cause and location of the vascular insults. Early surgical intervention in association with vascular surgeons helps in getting better outcome and prevents complications related to vascular injuries.
Keywords: Distal humeral fracture, brachial artery thrombosis, humerus shaft fracture, embolectomy.
The humerus fractures can present as isolated or associated with other injuries and these fractures can be associated with both primary and secondary iatrogenic or traumatic neurovascular injuries. Vascular injuries are rare in distal humerus fracture. Brachial artery lesion may be secondary to various insults, such as entrapment, division, spasm of the vessel, the presence of an intimal tear, or thrombus formation. On the other hand, the relative incidence of nerve injuries has been reported as being 12–20% [1, 2] and they mainly (86–100%) consist of neuropraxia, which usually resolve spontaneously. The annual incidence of brachial artery injuries after closed elbow injuries ranges from 0.47% to 0.5% [3]. The complications of brachial artery injury include gangrene and limb loss as well as long-term complications of limb ischemia including reduced range of motion, Volkmann’s contracture, and cold intolerance. We present two cases closed humerus fractures with brachial artery thrombosis in adult patients and their management.
Case 1
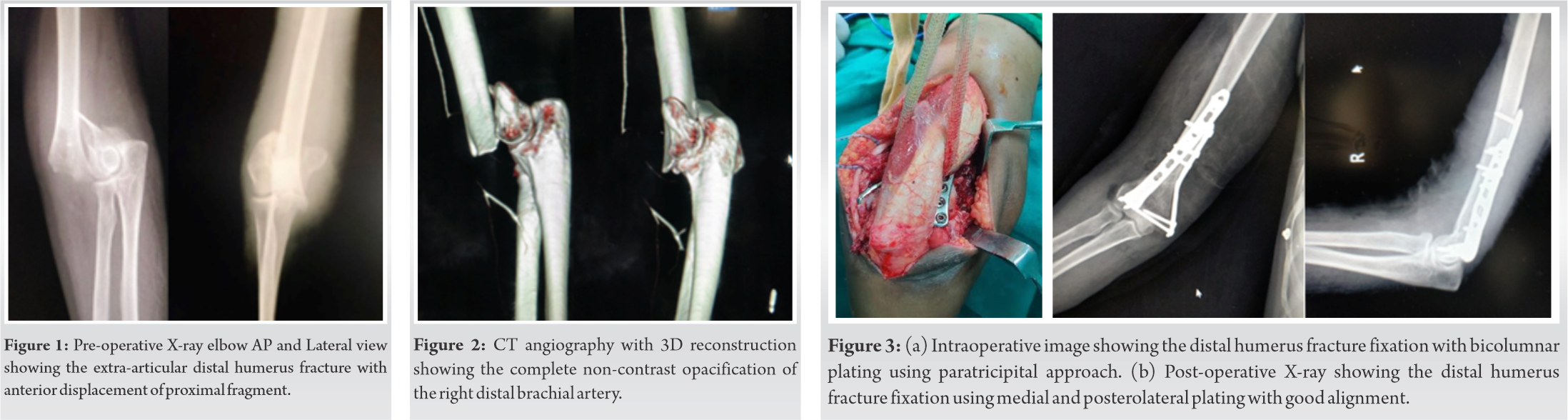
A 56-year-old female patient presented with pain, swelling in the right elbow since 4 h. Patient had a history of fall due to slip. Examination revealed the deformity at the right elbow with absent radial pulse. X-ray of the right elbow revealed extra-articular distal humerus fracture with anterior displacement of the proximal fragment (Fig. 1). Urgent CT angiography of the right upper limb revealed complete non-contrast opacification of right distal brachial artery approximately for a length of 2.8cm suggestive of thrombosis (Fig. 2). CVTS opinion was taken and they advised urgent embolectomy SOS interposition grafting. The extra-articular distal humerus fracture was fixed with medial and posterolateral bicolumnar plating using paratricipital approach (Fig. 3a, 3b).
After the bony fixation, CVTS surgeons intervened and explored the brachial artery through anterior midline incision. Arteriotomy was done after the adequate heparinization, Fogarty catheter was passed distally in each branch and proximally. Around 3–4 cm thrombus removed (Fig. 4), adequate flow confirmed and arteriotomy closed using proline 6–0. After the embolectomy, the radial and ulnar pulsation’s were normal. Postoperatively, patient was started on injection heparin 5000IU IV, Tab warfarin 2mg OD, Tab ecosprin 75 mg OD, and antibiotics for 5 days. Post-operative repeat Doppler showed no significant abnormality. At follow-up, patient is having good functional and radiological outcome without any complications.
Case 2
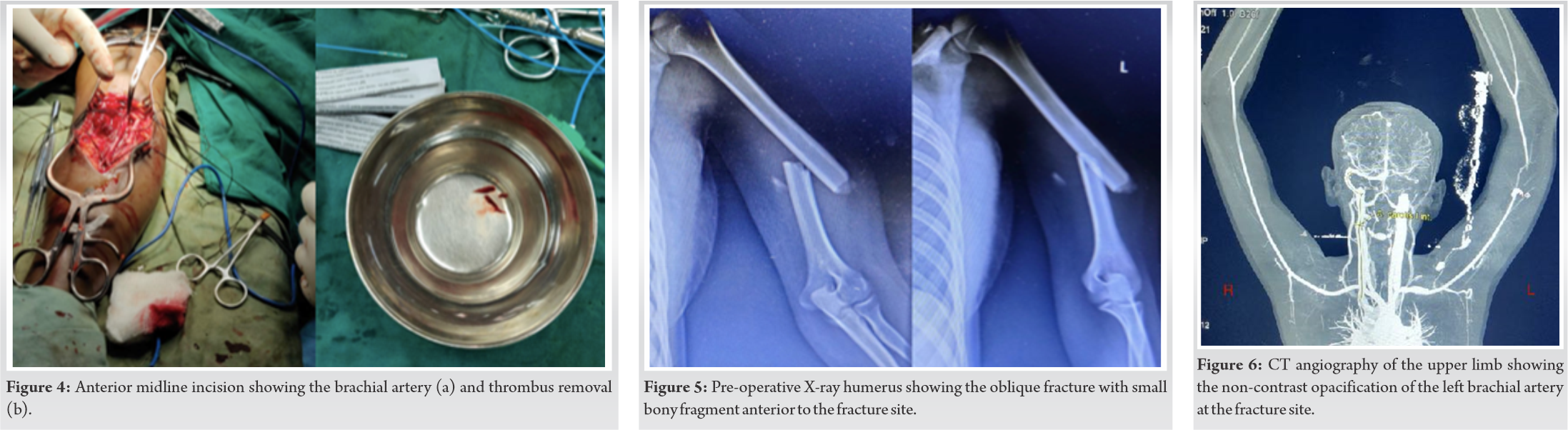
A 32-year-old female came with complaints of mid backache, left wrist pain, left arm pain, and deformity. Patient had a history of fall from 3rd floor. On examination, tenderness was present over mid back, left wrist and arm. Left upper limb radial pulse was absent with normal pinprick and capillary refill. X-ray of the LS spine, wrist and arm revealed the L2 compression fracture with left distal radius dorsal Barton’s fracture and left humerus shaft oblique fracture with one small bony fragment lying anterior to the fracture (Fig. 5). CT angiography of the left upper limb revealed left brachial artery short segment luminal narrowing, and partial contrast opacification around the fracture site (Fig. 6).
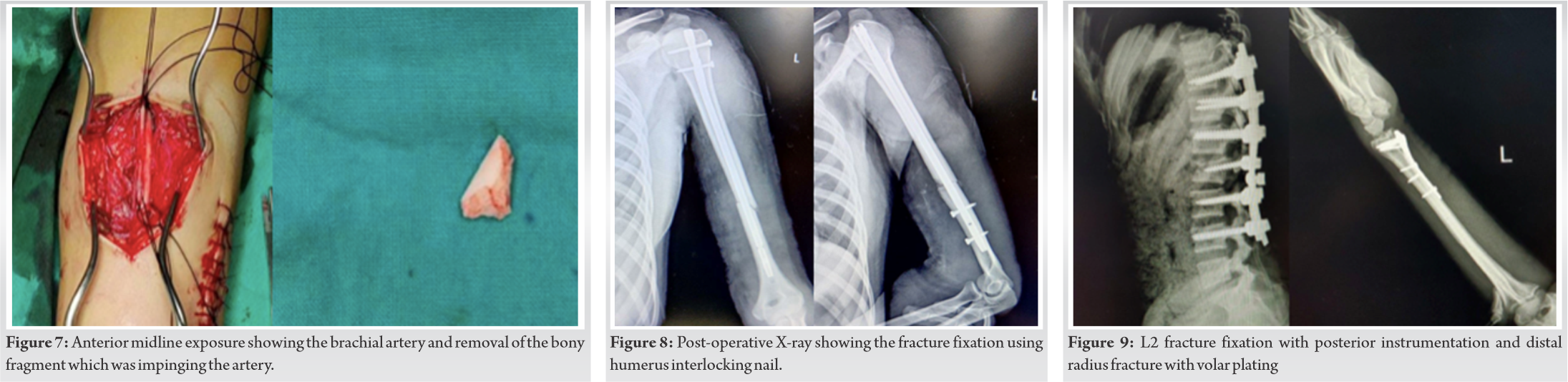
The CVTS reference was done for the same; they advised urgent bony fixation and exploration of the brachial artery. The bony fixation for the humerus shaft was done using closed humeral interlocking nail on the same day of trauma. After the bony fixation, the CVTS surgeons explored the brachial artery at the fracture site. They observed that, the small bony fragment which was away and anterior to the fracture site was impinging on the brachial artery. The bony fragment was removed and embolectomy was done using fogarty catheter (Fig. 7). After the embolectomy, the radial and ulnar pulses were present. Postoperatively injection heparin 5000 IU IV 6 hourly, tab warfarin 1 mg OD, Tab ecosprin 75 mg OD, and antibiotics were given for 5 days. Post-operative X-ray of the humerus showed good alignment at the fracture site (Fig. 8). Both the spine L2 fracture and distal radius fracture were operated in the same setting with posterior instrumentation, decompression, and volar plating, respectively, after 10 days of the initial surgery (Fig. 9). At follow-up, the patient is having good functional and radiological outcome (Fig. 10).
The brachial artery injury can be associated with displaced proximal humerus, humerus shaft, and distal humerus fractures. The nerve injuries are more common in humerus shaft fractures compared to arterial injuries. The brachial artery is more vulnerable to injury at its distal end, because this portion may be trapped between the rigid bicipital aponeurosis and the dislocated bony structures, particularly the distal part of the humerus [4]. There should be a high index of suspicion for brachial artery injury when a patient presents with blunt trauma from a fall onto the elbow, along with signs suggesting fracture or dislocation. The signs of limb ischemia are often not present, due to the rich collateral supply of the upper limb. Patients present with subtle signs such as palpable but diminished pulses, decreased capillary refill, and reduced pulse oximetry readings, such upper limbs are called “pink pulseless hands” by Brahmamdam [5]. The thorough clinical examination of the distal neurovascular deficits in any type of fracture/dislocations is very important to prevent these vascular insults. Vascular injuries secondary to supracondylar fractures of the humerus need emergency orthopedic and vascular management. Acute ischemic findings associated with elbow fractures include severe extremity edema and pain which make diagnosing the vascular injury much more difficult [6]. As a result, these patients are usually referred with a delay in diagnosis and signs of contracture and frank ischemia. Initially after trauma of the elbow, surrounding ecchymosis associated with joint deformity should be carefully and promptly evaluated. Pain, paresthesia, paralysis, pulselessness, pallor or poikilothermia when apparent are associated with muscular necrosis [7]. However, they may be noted early and can be helpful in guiding the management of vascular injury [8]. Radiographic evaluation of the vascular lesion includes both invasive and non-invasive techniques. Doppler, magnetic resonance angiography and color-flow duplex scanning are non-invasive techniques that may obtain anatomically and hemodynamically useful information. Angiography is an invasive technique that can be performed either before surgery in the angiography suite or in the operating room, with the aid of a C-arm. Its role in the investigation of an absent radial pulse is still under debate [7]. Pre-operative evaluation based on a thorough clinical examination with the aid of Doppler sonography is considered to be sufficient in evaluating the patency of the brachial artery. Color Doppler ultrasonography for the evaluation of arterial patency and circulation at the fracture site is useful. Arteriography in those patients with debatable vascular injury is indicated to localize the vascular injury [9]. Urgent vascular surgeon consultation and intervention are very important in managing these type of vascular insults. The fixation methods can be both external and internal. Compound fractures with vascular injuries are better managed with initial external fixator. The closed fractures with vascular injuries can be managed with internal fixation using plates or intramedullary nails as done in our case. Even small bony fragment can cause brachial artery impingement causing thrombosis, which is observed in our case.
Proper early clinical evaluation for vascular deficits helps to prevent the delayed diagnosis and radiological investigations helps to identify the cause and location of the vascular insults. Early surgical intervention in association with vascular surgeons helps in getting better outcome and prevents complications related to vascular injuries.
Vascular injuries are rare but one should not miss the diagnosis at the earliest. Knowledge regarding the vascular insults in humerus fractures is very essential to prevent the delayed diagnosis and related adverse outcomes. Management of humerus fractures with brachial artery injury requires the multidisciplinary approach with the involvement of orthopedic surgeons, radiologist, and vascular surgeons.
References
- 1.Campbell CC, Waters PM, Emans JB, Kasser JR, Millis MB. Neurovascular injury and displacement in Type III supracondylar humerus fractures. J Pediatr Orthop 1995;15:47-52. [Google Scholar]
- 2.Culp RW, Osterman AL, Davidson RS, Skirven T, Bora FW Jr. Neural injuries associated with supracondylar fractures of the humerus in children. J Bone Joint Surg Am 1990;72:1211-5. [Google Scholar]
- 3.Garrigues GE, Patel MB, Colletti TP, Weaver JP, Mallon WJ. Thrombosis of the brachial artery after closed dislocation of the elbow. J Bone Joint Surg Br 2009;91:1097-9. [Google Scholar]
- 4.Marcheix B, Chaufour X, Ayel J, Hollington L, Mansat P, Barret A, et al. Transection of the brachial artery after closed posterior elbow dislocation. J Vasc Surg 2005;42:1230-2. [Google Scholar]
- 5.Brahmamdam P, Plummer M, Modrall JG, Megison SM, Clagett GP, Valentine RJ. Hand ischemia associated with elbow trauma in children. J Vasc Surg 2011;54:773-8. [Google Scholar]
- 6.Kumar R, Trikha V, Malhotra R. A study of vascular injuries in pediatric supracondylar humeral fractures. J Orthop Surg (Hong Kong) 2001;9:37-40. [Google Scholar]
- 7.Shaw BA, Kasser JR, Emans JB, Rand FF. Management of vascular injuries in displaced supracondylar humerus fractures without arteriography. J Orthop Trauma 1990;4:25-9. [Google Scholar]
- 8.Copley LA, Dormans JP, Davidson RS. Vascular injuries and their sequelae in pediatric supracondylar humeral fractures: Toward a goal of prevention. J Pediatr Orthop 1996;16:99-103. [Google Scholar]
- 9.Friedman RJ, Jupiter JB. Vascular injuries and closed extremity fractures in children. Clin Orthop Relat Res 1984;188:112-9. [Google Scholar]