Global softening of femoral head after one year of neglected dislocation warrants replacement of the femoral head.
Dr. Shakti Swaroop,
Department of Orthopaedic Surgery, Institute of Medical Sciences and SUM Hospital, Bhubaneswar, Odisha, India.
E-mail: drshaktiswaroop@hotmail.com
Introduction: Neglected hip dislocation in adults may present as a dilemma to an orthopedic surgeon and is an uncommon occurrence. Literature mentions both closed reduction and open reduction as methods of management but mostly in children. Few cases have been present in the literature regarding adults with neglected hip dislocations. While almost all have failed in closed reduction, the open reduction has not yielded good results and total hip arthroplasty (THA) as a single stage procedure has not been explored much in regard to neglected isolated posterior dislocations of the hip. We report a series of three cases all with neglected dislocation of over 1 year which was managed with single stage total hip replacement.
Case Report: Three cases of neglected posterior dislocation of the hip of more than 1 year (26 years, 28 years, and 32 years of age all males) presented with right leg in adduction, flexion, and internal rotation deformity and painful limp. They were all managed inadequately by traditional bonesetters. No signs of acetabular fracture or avascular necrosis (AVN) were present in radiography and computer tomography. A global softening of the femoral head was encountered in all the cases and uncemented THA was done. All patients did well with good to excellent functional outcomes (Harris hip score [HHS] of 81, 91, and modified HHS of 83) with a minimum of 1 year follow-up. No post-operative complications were encountered.
Conclusion: We want to emphasize the lack of literature concerning adult patients with neglected dislocations. Single stage THA is the best option considering the occurrence of AVN of the femoral head with global softening in such cases. A single stage THA attains good to excellent functional outcomes without any early post-operative complications.
Keywords: Avascular necrosis, neglected dislocation, total hip replacement.
It is extremely rare to find hip dislocations that have been neglected in adults for more than a year. But in some developing countries, where remains a strong belief in the traditional bone setters, one may bump upon such a case in his/her practice. Due to rarity, there is a paucity of literature and hence a suitable algorithm of management for these cases in young adults is lacking. Most of the published articles related to neglected dislocations have been in children who have largely been managed by open reduction with variable results [1, 2, 3, 4]. Adults however differ from children in some aspects which throws additional challenges in their management.
1. Osteonecrosis is less in children due to the lower energy required to cause dislocation.
2. Children have the great potential of remodeling once dislocation is reduced.
3. Children have more pliable tissues, cartilage, and better vascularity. In adults, good results have been achieved in only four out of six patients with neglected dislocation of more than 3 months managed with primary reconstruction [5]. Ilyas and Rabbani have mentioned primary total hip arthroplasty (THA) to have better outcomes in such cases [6]. However, both these articles mention only Types II, III, IV, and V (Epstein Thompson classification) fracture dislocations of the hip which are inherently unstable. Attempts of closed reduction have failed in adults when the duration of neglect has been more than 3 months as fibrous tissue is present in the acetabulum [4]. Li et al. have mentioned the results of open reduction in neglected hip dislocations in 13 patients with a mean duration from injury to the intervention being 5 months, only 7 of 13 patients reported favorable outcomes and only 5 patients were pain free [7]. Here, we report our experience in dealing with three patients (2017–2020) of Type 1 (Epstein and Thompson classification) neglected dislocation of greater than a year duration which were managed with single stage primary THA.
Case 1
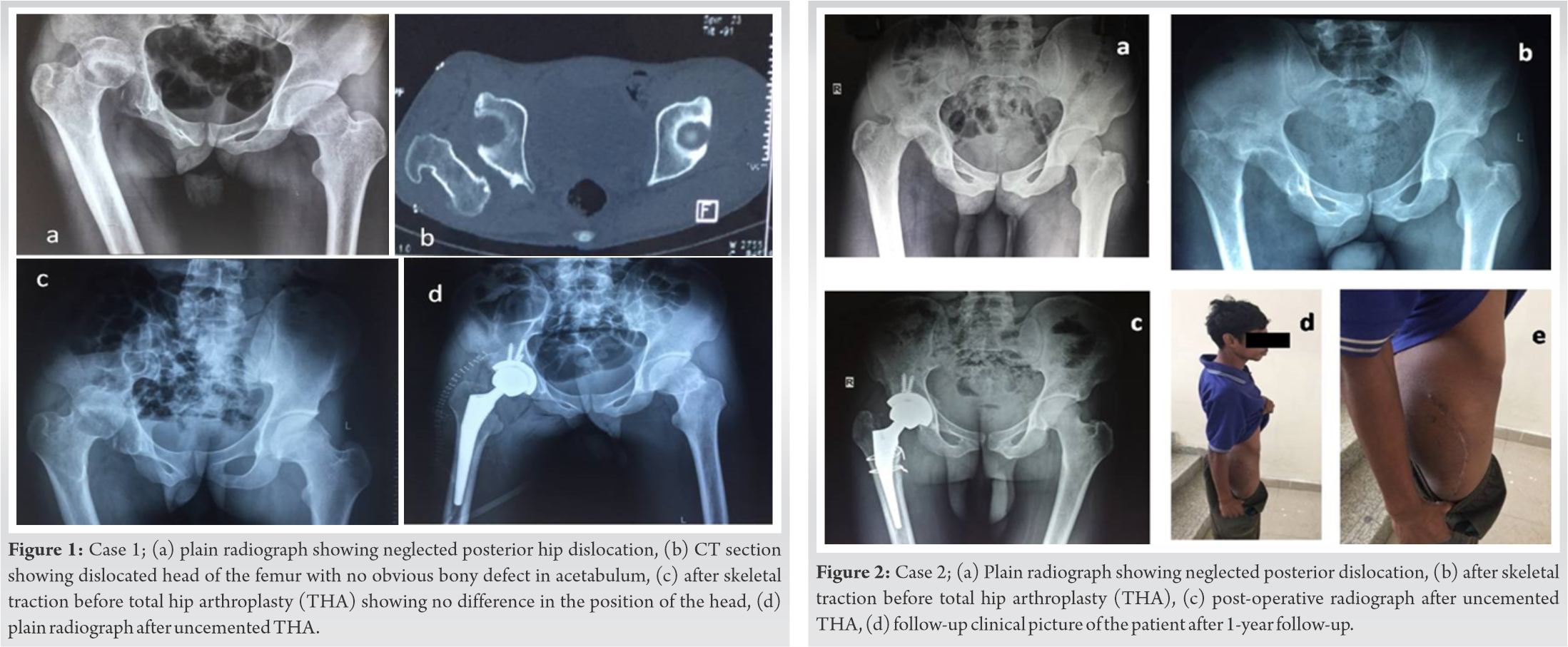
A 26-year-old male presented to us with an antalgic Trendelenburg gait over the right leg. He gave a history of a 2-year-old road traffic injury and subsequent treatment at a local hospital for about 2 months for a head injury. He went to the bone setters for further treatment. He presented to us with a fixed flexion, adduction, internal rotation deformity and shortening of 5 cm with a Harris hip score (HHS) of 42 (Fig. 1).
Case 2
A 28-year-old male patient presented to us with fixed flexion, adduction. internal rotation and 4 cm shortening deformity post 1½ years history of fall from height. He too had visited the traditional bonesetters. He had similar deformities and shortening of 4 cm in his right lower limb with HHS of 35 (Fig. 2).
Case 3
This 32-year-old gentleman with a history of a road traffic accident a year before, now presented with a painful limp, shortening, adduction, and internal rotation deformity again in the right lower limb. The patient confessed to having taken some traditional treatment for 4 months. Then he visited a local medical center but received treatment only in the form of traction for 4 weeks but the dislocation persisted. He had a shortening of 3 cm and his HHS was 27 (Fig. 3). Radiographs and computer tomography were done to look for any acetabular defects. However, the usefulness of magnetic resonance imaging (MRI) was not going to change the plan of management and hence was not done. The plan was to go for either an open reduction or THA depending on the condition of the femoral head. Discussion regarding the risks and benefits of both the procedures were done with the patient. The chances of residual shortening and neuro deficit were explained in detail.
Initial heavy traction (10–12 kg) was given for 4 weeks preoperatively. The surgery involved a posterior (Southern) approach to the hip and the femoral head was found to be globally soft. Hence, it was decided to replace the joint. Generous releases were performed all around the head and the neck was osteotomized as low as feasible. Fibrous tissue was found to be obliterating the acetabulum and was debrided. The femoral trial was tested first for a reduction in the native acetabulum to check for the need for a femoral shortening osteotomy. Subsequently, the acetabulum was prepared and uneventful cementless THA was done (Fig. 4).
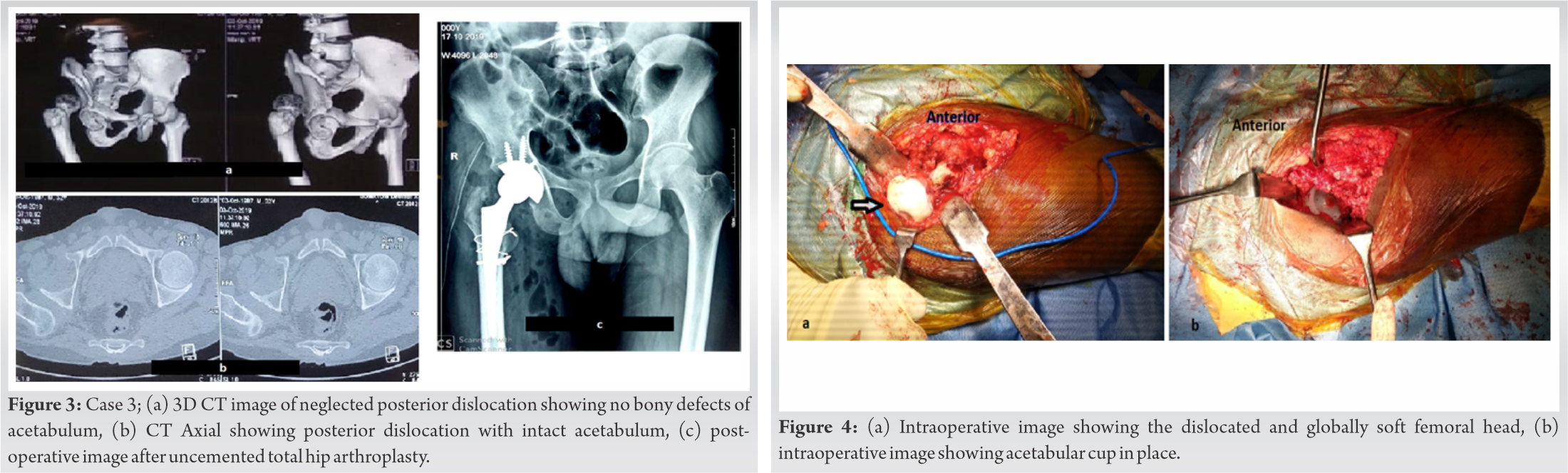
No immediate post-operative complications were noted. Partial weight bearing with a walker was allowed from the 3rd post-operative day and patients were discharged after suture removal. They had gained length (3–3.5 cm) but there was no neurological deficit. These patients are on regular follow-up. The first two patients have a 2 years follow-up with HHS of 81 and 91, respectively, while the third has been doing all activities at home but failed to turn up due to the COVID-19 pandemic. On telephonic interview, we found a modified HHS of 83. Thus, all have a good outcome (HHS>80).
Neglected posterior dislocation of the hip is found in developing countries due to several reasons. Sometimes, the patient is unable to reach the medical facility timely or at times he/she reaches when the dislocation is already old due to inadequate treatment by local bone setters as seen in all our cases. A dislocation of the hip can also be missed in polytrauma patients, where the more conspicuous or life-threatening injuries take precedence and the patient has had blunted consciousness. Hip dislocation is an emergency and must be reduced within the first 6 h to avoid the chances of devascularization of the femoral head that increases by 20 folds post the critical time, leading to avascular necrosis (AVN) [8]. Hougaard and Thomsen reported an incidence of 6% of AVN in dislocations reduced within 6 h after injury and this incidence markedly increased to 58% in hips reduced after a delay beyond 6 hours [9]. Few authors have reported AVN in 100% cases of neglected hip dislocation treated with initial traction and open reduction [9, 10]. Most of the literature consists of children or adolescents who require less energy trauma for dislocation to occur and have lower chances of AVN as compared to adults [2, 4]. As the energy of trauma is also an important factor in causing AVN with high energy trauma having more chances of AVN [11, 12, 13]. Few authors have reported rates of 0–15% of AVN even in cases of neglected dislocations mostly in children which can be attributed to the low energy of trauma [2, 3, 4]. An unreduced pure posterior hip dislocation is an unsolved problem with most of the literature reporting cases in the pediatric age group [2, 4, 10, 14]. Most of the authors recommend initial traction followed by open reduction by either lateral or posterolateral approach [2, 3, 11]. Concentric reduction is very important in children as the femoral head must remain in the acetabulum for normal growth and remodeling. Studies on neglected cases of pure posterior dislocation (Type I) are lacking in adults. Few articles dealing with neglected dislocations having associated acetabulum fracture (Type II or higher) have found that primary THA yields the best results [6, 12]. However, we are reporting young adult patients of >1-year-old dislocations without associated fractures which have not been adequately managed as previous literature is scarce (Table 1).
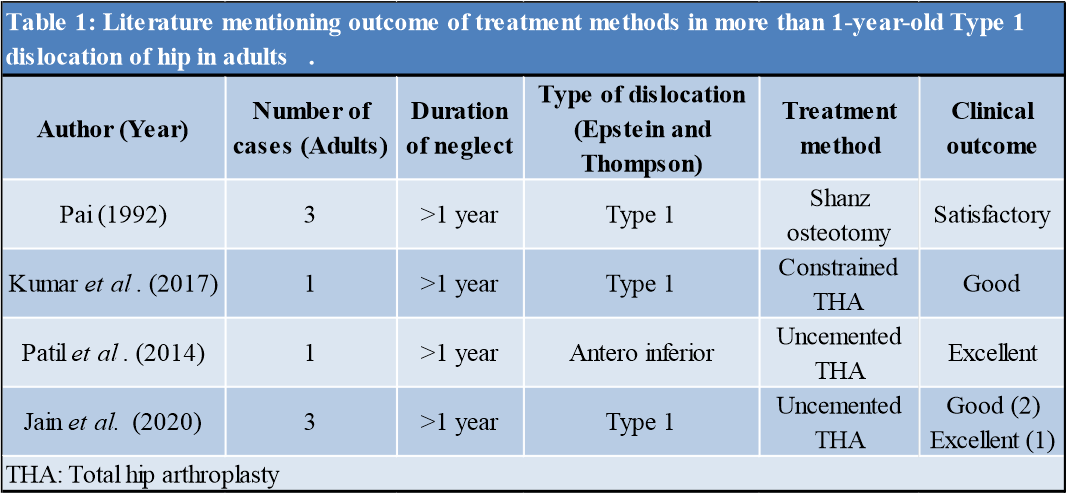
The occurrence of AVN and early arthritis is still high in such cases which may affect long-term outcomes [10, 11]. Banskota et al. reported a mean follow-up of 7 years and 7 months in 8 patients all of whom had limp and 5 had persistent pain [10]. It is a different scenario in adults with neglected dislocation as they have a higher chance of AVN, that is, >50% and chances of post-traumatic arthritis of 24% with a sedentary lifestyle and in 37.5% with active lifestyle [9, 15]. AVN can cause poor functional outcome in cases which have been manipulated and reduced irrespective of open or closed methods after a prolonged delay. Gardner et al. in their study of 7 cases reported 1 with gross softening of the femoral head, who did not do well after open reduction as the softening lead to flattening of the head with associated limp and pain [3]. We noted global softening of the femoral head in all our cases and thus planned for total hip replacement. As the femoral head was in a non-weight bearing position, the radiological changes of AVN were probably not present and the head appeared spherical. All patients achieved good functional scores and were followed up for a minimum of 1 year. Closed reduction with heavy traction and abduction in adults has been described but has failed when the delay has been more than 9 months [14]. Pai achieved closed reduction by traction in 2 out of 6 adult patients who were of a duration < 3 months [4]. Other authors have failed to achieve closed reduction and have had to resort to open reduction with good to excellent results in 37 of 39 cases which were mostly children [2, 3, 7, 10, 11]. Fibrous tissue develops in the acetabulum after 3 months of delay which makes close reduction impossible or causes a non-concentric reduction thus needing open reduction [12]. Li et al. achieved good to excellent results in only 7 adult patients out of the 13 patients treated with traction and open reduction with a mean duration from injury to treatment being 5 months [7]. In our study, two cases were more than 1-year old and one case was more than 2-years-old Type 1 dislocations. Pai in 6 cases of more than 1-year old dislocations did Shanz osteotomy and achieved satisfactory results; however, these procedures are less satisfactory in the current scenario than a total hip replacement [4]. Ilyas and Rabbani in their published article performed THA in Grades III and IV type of dislocations and achieved significant improvement in outcome [6]. Thus, our study is unique as it mentions Type 1 dislocation with more than 1-year delay in an adult age group which has been managed successfully with single stage THA. We justify not doing MRI before the tentative procedure as it would have made no difference to our plan of management which was either an open reduction or THA subject to the condition of the femoral head. Our recommendation would be a single stage THA in cases of more than 1-year old neglected dislocations in steps as described. Kumar et al., Pankaj et al., and Patil et al. have also managed a 2 year old posterior dislocation, a 6-month-old obturator type dislocation, and a more than 1-year antero-inferior type dislocation respectively with uncemented THA and reported good to excellent outcomes [16, 17, 18]. We can achieve a mobile painless and stable joint that gives the patient a productive life. Even without the softening of the femoral head open reduction may further increase the chances of AVN due to the various soft-tissue releases required to reduce the head and lead to arthritis as articular defects may have occurred due to the initial injury or during manipulation intraoperatively. We have excellent to good outcomes in all our cases with a minimum of 1-year follow-up.
AVN occurs even in the absence of radiographical changes as seen intraoperatively in all our cases. Single stage THA done in steps as described gives a good to excellent functional outcome in young adults presenting with neglected hip dislocations of more than a year. However, we must keep collecting follow up data and reporting a larger number of such cases in the future.
This case series will enhance clarity into the controversial topic of dealing with neglected dislocation of the hip in adults and highlight the good functional results that can be achieved by single stage total hip replacement. Very few cases of more than 1 year of neglected dislocations in adults have been reported in the literature and very limited literature is present regarding single stage total hip replacement in such cases.
References
- 1.Pal CP, Kumar D, Sadana A, Dinkar KS. Neglected posterior dislocation of hip in children-a case report. J Orthop Case Rep 2014;4:21-4. [Google Scholar]
- 2.Aguilar JA. Treatment of neglected traumatic posterior hip dislocation in children. Tech Orthop 2006;21:143-9. [Google Scholar]
- 3.Gardner RO, Worku N, Nunn TR, Zerfu TT, Kassahun ME. Management of neglected traumatic hip dislocation in children. J Pediatr Orthop 2020;40:e554-9. [Google Scholar]
- 4.Pai VS. The management of unreduced traumatic dislocation of the hip in developing countries. Int Orthop 1992;16:136-9. [Google Scholar]
- 5.Garrett JC, Epstein HC, Harris WH, Harvey JP Jr., Nickel VL. Treatment of unreduced traumatic posterior dislocations of the hip. J Bone Joint Surg Am 1979;61:2-6. [Google Scholar]
- 6.Ilyas I, Rabbani SA. Total hip arthroplasty in chronic unreduced hip fracture-dislocation. J Arthrop 2009;24:903-8. [Google Scholar]
- 7.Li P, Tao F, Song W, Dong J, Qiu D, Zhou D. External fixation-assisted reduction for the treatment of neglected hip dislocations with limb length discrepancy: A retrospective study of 13 cases. BMC Musculosk Disord 2019;20:1-5. [Google Scholar]
- 8.Mehlman CT, Hubbard GW, Crawford AH, Roy DR, Wall EJ. Traumatic hip dislocation in children: Long-term follow up of 42 patients. Clin Orthop Related Res 2000;376:68-79. [Google Scholar]
- 9.Hougaard KJ, Thomsen PB. Traumatic posterior fracture-dislocation of the hip with fracture of the femoral head or neck, or both. JBJS 1988;70:233-9. [Google Scholar]
- 10.Banskota AK, Spiegel DA, Shrestha S, Shrestha OP, Rajbhandary T. Open reduction for neglected traumatic hip dislocation in children and adolescents. J Pediatr Orthop 2007;27:187-91. [Google Scholar]
- 11.Kumar S, Jain AK. Neglected traumatic hip dislocation in children. Clin Orthop Related Res 2005;431:9-13. [Google Scholar]
- 12.Epstein HC. Traumatic dislocations of the hip. Clin Orthop Related Res 1973;92:116-42. [Google Scholar]
- 13.Stewart MJ, Milford LW. Fracture-dislocation of the hip: An end-result study. JBJS 1954;36:315-42. [Google Scholar]
- 14.Gupta RC, Shravat BP. Reduction of neglected traumatic dislocation of the hip by heavy traction. J Bone Joint Surg 1977;59:249-51. [Google Scholar]
- 15.Upadhyay SS, Moulton A, Srikrishnamurthy K. An analysis of the late effects of traumatic posterior dislocation of the hip without fractures. J Bone Joint Surg 1983;65:150-2. [Google Scholar]
- 16.Kumar S, Dahuja A, Narula MS, Garg S, Kaur R. Neglected hip dislocation: An unusual presentation, its management and review of the literature. Strateg Trauma Limb Reconstruct 2017;12:189-92. [Google Scholar]
- 17.Pankaj A, Sharma M, Kochar V, Naik VA. Neglected, locked, obturator type of inferior hip dislocation treated by total hip arthroplasty. Arch Orthop Trauma Surg 2011;131:443-6. [Google Scholar]
- 18.Patil K, Daultani D, Bami M, Ithli M. Neglected antero-inferior dislocation of hip treated with primary reverse hybrid THR-a rare case report. World J Med Surg Case Rep 2014;3:1-28. [Google Scholar]








