In cases of chronic osteomyelitis not responding to treatments, clinicians and radiologists should always suspect history of foreign body prick, even though patient does not recall any such precedent incident.
Dr. Sanjay Desai,
Department of Radio Diagnosis, Deenanath Mangeshkar Hospital, Pune, Maharashtra, India.
E-mail: mskraddmh@gmail.com
Introduction: Thorn prick is commonly seen in people that are involved in gardening. In some cases, they are unaware of the precedent thorn prick or present for medical attention quite late and forget about the history of thorn prick. In such cases, it is challenging for the clinicians and the radiologist to rule out the cause of the osteomyelitis caused by an unrecognized foreign body.
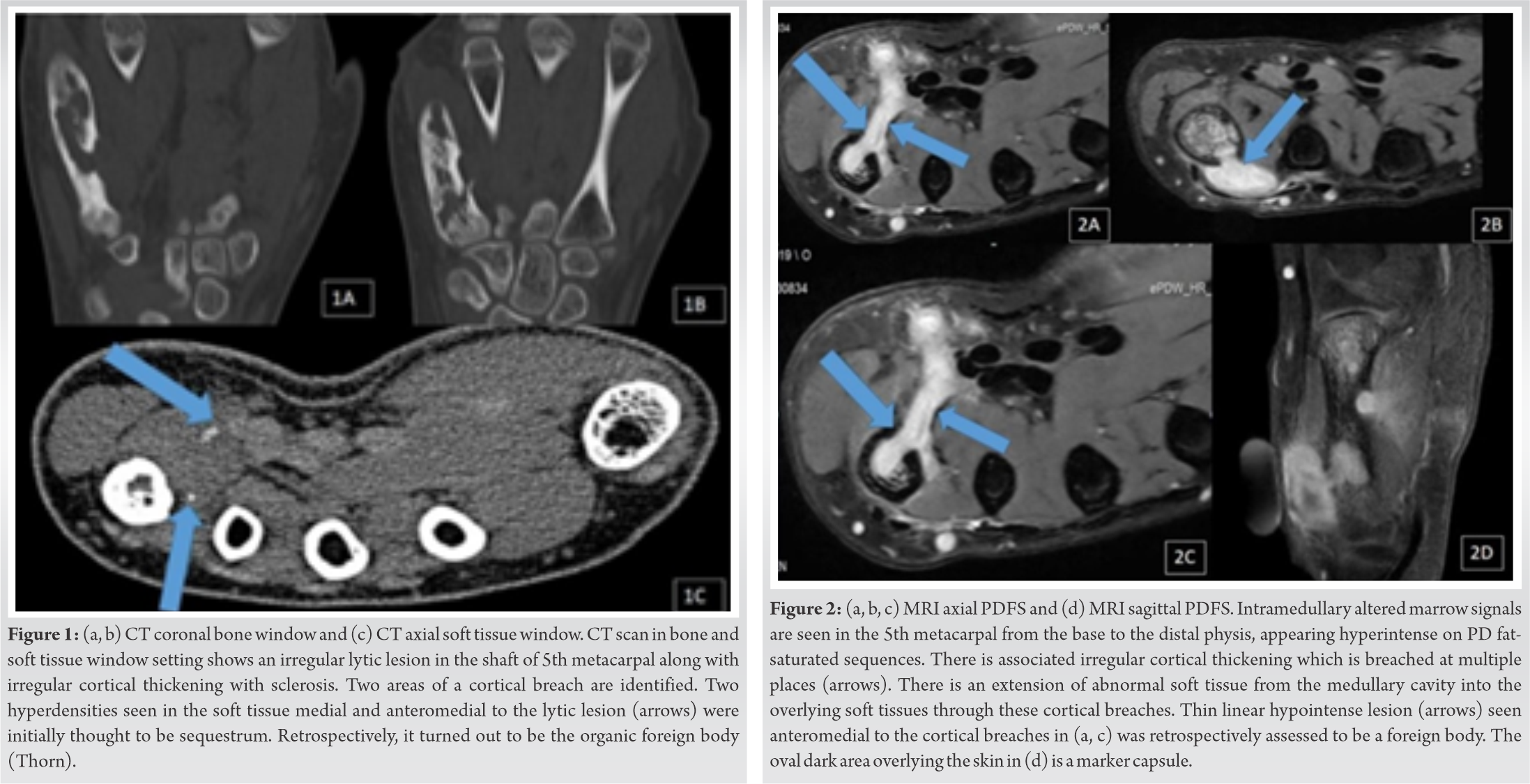
Case Report: A 14-year-old girl presented with a swelling of the hand and discharging sinuses with a radiographic picture of osteomyelitis of the 5th metacarpal. The CT and MRI showed features consistent with osteomyelitis as well, possibly tuberculous in etiology. Even after the completion of AKT (anti-tubercular treatment), the patient continued to have discharging sinuses out of which a plant thorn spontaneously egressed, and subsequently, the patient was completely relieved of her symptoms. Retrospective evaluation of the MRI showed the presence of a foreign body that was hyperdense on CT and was initially thought to be a sequestrum.
Conclusion: Hence, even though a definite history of trauma/thorn prick is not given (although highly unusual in the case of hand), an organic foreign body should be considered in the etiologic differential diagnosis of non-responding chronic osteomyelitis and discharging sinuses.
Keywords: Thorn, osteomyelitis, hand.
To detect retained wooden foreign material in the body remains a very difficult task. There is a tendency for the patients to often present for assessment even months to years after they have had their initial injury, and therefore, during evaluation clinicians may not be able to get a proper antecedent history of skin puncture by a foreign body. And even when there is a history of penetrating trauma, one is unable to estimate the severity of the puncture clinically. Even when we have a high suspicion of a retained foreign body, it still remains a difficult job to localize it on imaging. Wood may remain as an unrecognized nidus for infection, therefore its detection is very much important. Since it is organic, it acts as a vulnerable medium for infections, hence retained wooden foreign bodies may also result in fistula formation along with cellulitis or abscess formation as well as osteomyelitis and synovitis. This case report demonstrates such a case in which the initial investigations pointed to tuberculous osteomyelitis for which AKT was taken. After spontaneous relief of symptoms due to extrusion of the foreign body, the retrospective analysis pointed that the foreign body was initially thought to be a sequestered bony fragment secondary to osteomyelitis. Hence, a strong suspicion of a foreign body must be entertained in each case of hand/foot osteomyelitis.
A young girl presented with swelling of the hand and discharging sinuses for a few months. No definite history of trauma was given. The plain CT scan revealed an irregularly marginated lytic lesion in the shaft of the 5th metacarpal with irregular cortical thickening and sclerosis. Few areas of the cortical breach were identified with associated soft tissue lesions. Few hyper densities seen within the soft tissue component were thought to be sequestra prompting the diagnosis of chronic osteomyelitis (Fig. 1). For further evaluation of the soft tissues, MRI was done which revealed intramedullary T2/PDFS hyperintense signals in the 5th metacarpal bone from the base to the distal physis with associated cortical breaches at multiple places. Associated soft tissue component was seen showing predominantly peripheral post-contrast enhancement with central liquefied components, suggestive of abscesses. The thin linear hypointense area adjacent to the soft tissue collection near one of the cortical breaches corresponding to CT hyperdensity was assessed to be sequestrum (Fig. 2). Considering the clinical profile with discharging sinuses and history of a few months, chronic osteomyelitis, possibly tuberculous in etiology was considered. Anti-tubercular therapy (ATT) was, therefore, initiated. However, even after completion of ATT, the patient continued to have discharging sinuses and no obvious symptomatic relief was seen. One day, a plant thorn spontaneously egressed from the sinus and subsequently, the patient was completely relieved of her symptoms. Subsequent antibiotic therapy led to the resolution of osteomyelitis as well. Retrospective evaluation of the CT and MRI showed the presence of a foreign body which was initially thought to be sequestrum. Hence, even without a definite history of trauma / thorn prick, an organic foreign body should be considered in the etiologic differential diagnosis of non-responding chronic osteomyelitis and discharging sinuses.
We can identify glass, ceramic, and metallic foreign matters on plain radiographs as they are radiopaque. Organic materials and plastics, however, appear radiolucent [1]. Bone changes usually manifest several months to years after the trauma in the case of foreign bodies [2]. The diagnostic challenge arises as the patients may forget about the initial injury, just as in our case. Thorn is an organic foreign body, which can develop foreign body granuloma, resulting in periosteal reaction or even osteolysis. It can also cause synovitis due to a chemical reaction within the joint. If it remains in the sub-periosteal region for some time, it can cause a sub-periosteal reaction with fluid collection followed by periosteal elevation. Subsequently, this causes devitalization of the cortical bone, hence, resulting in a sequestrum [3, 4]. The periosteal reaction can mimic conditions like osteomyelitis, bone cysts, or any aggressive bony neoplasms. In soft tissues, the retained plant thorn can also cause foreign body cyst, bursitis, tenosynovitis, and synovitis [2, 5]. Since they are not radio-opaque, X- rays are negative for the organic foreign matter until and unless bony lesions develop which warrants further investigations [3]. On ultrasonography, a thorn is highly echogenic due to the presence of entrapped air with acoustic shadowing and can therefore help identify the wooden foreign body [6]. In CT, wood appears as a linear cylindrical area of increased attenuation, which is better seen in wide window settings [6]. It may also demonstrate hyper dense lesion, which is suggestive of sequestrum, and indicates the possibility of osteomyelitis [2]. With MR imaging, these foreign bodies show a variable signal intensity that is equal to or less than that of skeletal muscle on both T1- and T2-weighted images with surrounding inflammatory response [6]. Ipaktchi et al. [7], have suggested a diagnostic algorithm for the detection of these types of radiolucent foreign bodies where high-frequency ultrasonography is preferred first. If only it cannot visualize the lesion, CT/MRI can be used for further evaluation. According to their algorithm, if there is a history of trauma with metallic object then plain radiography should be done and if radiography is negative for a foreign body or if there is history of trauma with non-metallic object, then high-frequency linear ultrasonography should be done in the emergency department (ED). If the ultrasonography is negative, then CT/MRI should be considered. In cases where radiography or ultrasonography is positive, then superficial palpable foreign body should be explored in ED and operating room evaluation should be done for all other foreign bodies. Intraoperative pre-procedural ultrasonography localization of the foreign body should also be done. For ultrasound-guided foreign body removal, only a small incision in the skin is required, which must be wide enough for the foreign body to pass through. Surgical forceps are inserted to reach the foreign body under ultrasonography guidance to remove it [8]. According to this study, the effectiveness of US-guided percutaneous removal can be near 100%. For foreign bodies that are deep and not accessible through ultrasound, a three-dimensional CT data set can be used with intraoperative navigation systems in order to facilitate surgical removal [9]. Culture sensitivity of tissue/pus obtained along with the foreign body is usually inconclusive although the osteomyelitis is primarily induced by it [10].
In few cases of foreign body-induced osteomyelitis, the patients may not recall a history of foreign body prick. These patients are, therefore, evaluated with CT/MRI as first line study, which sometimes fail in identification of these foreign bodies from sequestrum. Hence, clinicians and radiologists should be highly suspicious for the foreign body as a possible etiology, in patients unresponsive to routine treatment protocols. Radiography for radiopaque, ultrasonography for recent/superficially located and CT are useful for radiodense and wooden foreign bodies with MRI remaining a problem-solving device in few isolated cases.
Even in cases when the patient does not recall any history of foreign body/ thorn prick, clinicians and radiologists should always suspect foreign body as etiology, whenever osteomyelitis does not resolve after completion of antibiotics/ antitubercular treatment.
References
- 1.El Bouchti I, Ait Essi F, Abkari I, Latifi M, El Hassani S. Foreign body granuloma: A diagnosis not to forget. Case Rep Orthop 2012;2012:439836. [Google Scholar]
- 2.Curiel AV, Romon MV, Lucia FC, Del Portal Bermundo MR, Bencano AC. Injuries from palm tree thorn simulating tumoral or pseudotumoral bone lesions. Acta Orthop Belg 2001;67:279-82. [Google Scholar]
- 3.Suresh SS. Orthopaedic manifestations of date thorn injury: Case series. Sultan Qaboos Univ Med J 2008;8:347-52. [Google Scholar]
- 4.Peters V, Rubin L, Gloster ES, Aprin H. Foreign-body osteitis of the metacarpal bone. Clin Orthop Relat Res 1992;278:69-72. [Google Scholar]
- 5.Barry M, Maffulli N, Good C. The missed thorn. Acta Orthop Belg 1992;58:468-70. [Google Scholar]
- 6.Peterson JJ, Bancroft LW, Kransdorf MJ. Wooden foreign bodies: Imaging appearance. AJR Am J Roentgenol 2002;178:557-62. [Google Scholar]
- 7.Ipaktchi K, Demars A, Park J, Ciarallo C, Livermore M, Banegas R. Retained palmar foreign body presenting as a late hand infection: Proposed diagnostic algorithm to detect radiolucent objects. Patient Saf Surg 2013;7:25. [Google Scholar]
- 8.Del Cura JL, Aza I, Zabala RM, Sarabia M, Korta I. US-guided localization and removal of soft-tissue foreign bodies. Radiographics 2020;40:1188-95. [Google Scholar]
- 9.Ji Y, Jiang H, Wan L, Yuan H. Effect of navigation system on removal of foreign bodies in head and neck surgery. J Craniofac Surg 2018;29:e723-6. [Google Scholar]
- 10.Gupta M, Kumar D, Jain VK, Naik AK, Arya RK. Neglected thorn injury mimicking soft tissue mass in a child: A case report. J Clin Diagn Res 2015;9:RD03-4. [Google Scholar]











