Gossypibiomas Presentation and Prevention.
Dr. Gabriel Pina,
Department of Orthopeadics, Centro Hospitalar Tondela-Viseu, Viseu Dão Lafões, Portugal.
E-mail: gabrielpina950@hotmail.com
Introduction: Gossypiboma or textiloma is the technical term used to describe a surgical complication related to accidental retention of surgical material within the body, most often surgical swabs. Since it is rare in orthopedic surgery, its diagnostis is less common and often initially mistaken with soft-tissue tumors. The aim of this study is to point out the importance of this differential diagnosis in the event of clinical swelling or accidental intraoperative finding associated with previous surgery.
Case Report: Female patient presenting with 3 weeks hip pain and inflammatory signs, with a past history of a total hip arthroplasty 15 years before. Analytically presented C-reactive protein CRP of 13.67 mg/dl. Ultrasound and computed tomography CT scan revealed a solid lesion in the anterior thigh root and a liquid lesion in the lateral region of the hip.
Discussion: Gossypibomas can be classified into two types: The aseptic fibrous type, which produces adhesions and a fibrotic capsule, and the exudative type, which is characterized by abscess formation. This case report refers to an aseptic fibrous type, given an asymptomatic evolution over 15 years and histopathological findings. However, this diagnosis occurred following a periprosthetic hip infection.
Keywords: Gossypiboma, muslinoma, textiloma, total hip arthroplasty.
Gossypiboma, textiloma, gauzoma, or muslinoma are the technical term used to describe a surgical complication related to accidental retention of surgical material inside the body, most often surgical swabs[1]. This type of operative complication is more frequent in abdominal and thoracic surgeries[2]. In the orthopedic field, the most common sites are hip and spine surgery. However, it is a surgical area where this type of diagnosis is rare, usually leading to others differential diagnosis, such as soft-tissue tumors [3]. From a clinical point of view, textilomas can have two types of clinical evolution: Silent asymptomatic evolution for years, being accidental intraoperative finding the most frequent form of diagnosis in this context. Another type of clinical course is symptomatic course, with a generally earlier diagnosis. The presence of symptoms is usually associated with compressive effects or infectious complications secondary to the foreign body presence [4]. The diagnosis is mostly made by computed tomography (CT), in 61% of cases, followed by X-ray, in 35% of cases and 34% by ultrasound [5]. Several risk factors are associated with gossypiboma, such asobesity, intraoperative surgical protocol modification, emergency surgery, and non-counting swabs during surgery [4, 5].
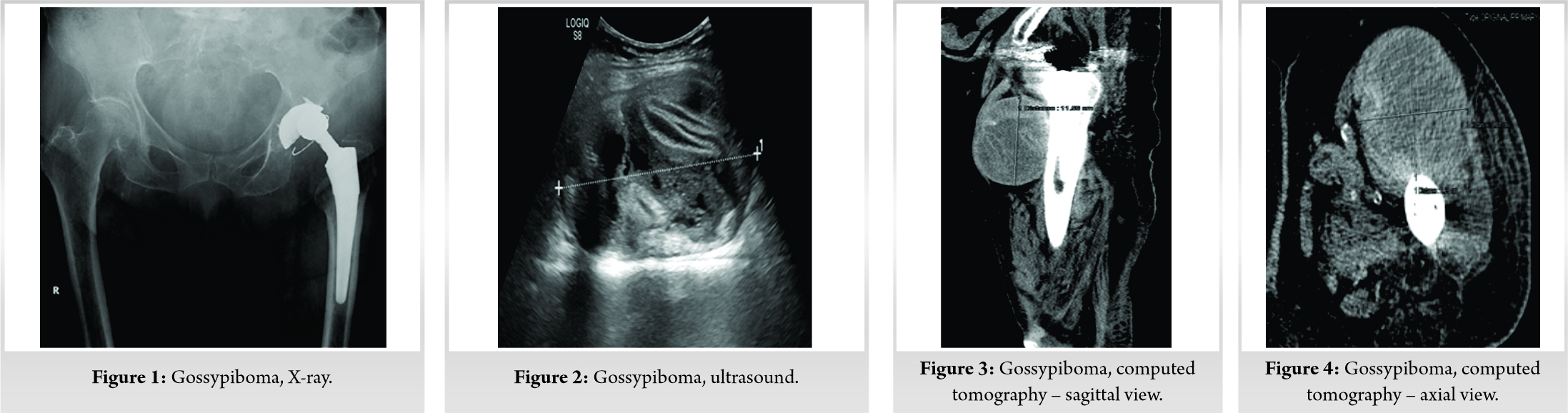
An 80-year-old female patient, independent daily activities, presented at the emergency department with a 3 weeks progressive intensity left thigh pain. The patient denied recent trauma. She also denied anorexia, weight loss, or asthenia. She had a history of total left hip arthroplasty 15 years ago due to hip osteoarthritis. Immediately after the arthroplasty, the patient reported that a swelling in the anterolateral thigh with no symptoms associated. At presentation, she was apyretic. She had edema of the anterolateral region of the left thigh root and flushing of the lateral hip region, without fistulas or wounds. On palpation, she had heat and pain. Range of motion was normal. Conventional pelvic X-ray (Fig. 1) revealed the presence of a soft-tissue shadow in the left proximal femur region and signs of total hip arthroplasty (THA) polyethylene wear. The acetabular and femoral components presented without signs of osteolysis or detachment. Analytically, the blood count presented valueswithin the normal range and a C-reactive protein (CRP)value of 13.67 mg/dl. At this stage, the hypothesis of periprosthetic infection was the most likely, considering the clinical and analytical findings. However, to clarify left anterolateral thigh swelling, a soft-tissue ultrasound was requested. Ultrasound (Fig. 2) revealed a well-defined solid nodular lesion of regular contours suggestive of foreign body in the anterior region of the left thigh root and a liquid collection in the lateral region of the hip. After these ultrasound findings, the accidental gossypiboma diagnosis was suggested. Following, a left hip CT scan (Fig. 3-5) was requested for better pre-operative characterization of the nodular lesion and the liquid collection.
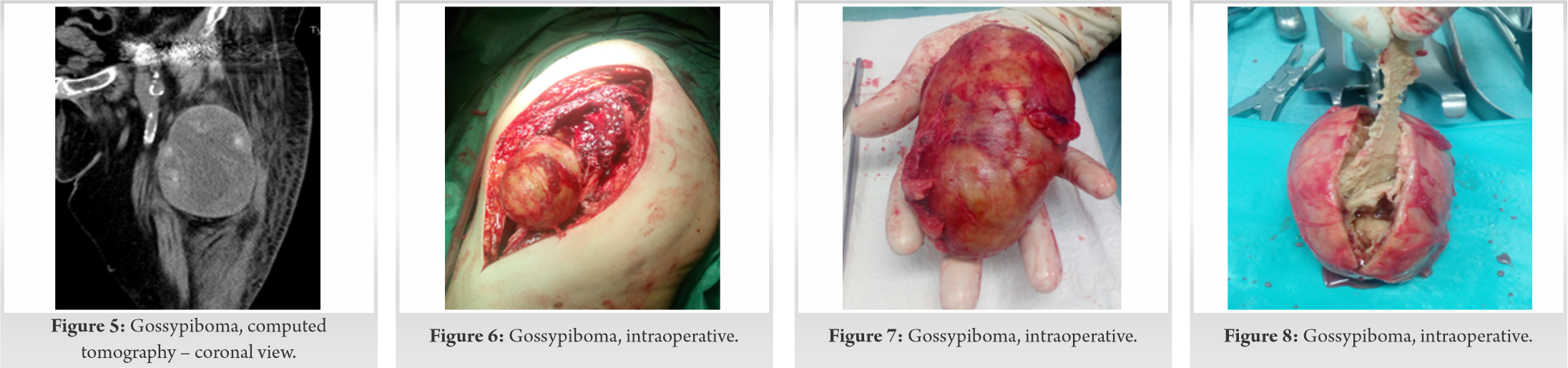
The patient was programmed for total hip prosthesis extraction, surgical debridement, and mass excision. A posterolateral approach was used. After removal of the hip prosthesis components, a well-defined, solid, capsulated 250 g, 12 cm × 8cm larger diameter lesion located in the anterior region of the left thigh root was identified intraoperatively (Fig. 6-8). It was also observed a periprosthetic purulent-like fluid. The anatomopathological study revealed that the removed surgical specimen had characteristics coincident with foreign body granuloma and the presence of elastic tissue inside. The microbiological examination was negative. Postoperatively, the patient underwent 4 weeks of empirical intravenous antibiotic therapy, followed by 2 weeks of empirical oral antibiotic therapy. No perioperative complications were observed. During the follow-up, the patient revealed inflammatory signs resolution of the anterolateral thigh and lateral hip, and blood test with CRP normalization. The second stage replacement arthroplasty was performed 8 months after the extraction of the prosthesis without complications. After 1 year of follow-up, she presented without pain and an independent walking ability. The Harris Hip Score recorded was 84 points at the date of the last follow-up.
While abdominal surgery stands out with 75% of textiloma cases, orthopedic surgery accounts for only 6% [6]. Gossypiboma can be classified into two types, according to Olnicket al. The aseptic fibrous type, which produces a well-defined fibrotic capsule. Olnick et al. also defined a second type of organic reaction, the exudative form of this pathology, where abscess formation is the characterizing element of this gossypiboma subtype [7]. Regarding the clinical case presented, its classification falls within the aseptic fibrous type. Although the patient has presented with a recent clinical and analytical exudative type, characterized by the early development of inflammatory symptoms in the perioperative period [8], the timing onset of these symptoms does not fit with the primary surgery, which was performed 15 years ago, period during which the patient was asymptomatic, highlighting the presence of anterolateral thigh swelling from the perioperative period of the first surgery. On the other hand, either imaging, where the lesion is defined as being well circumscribed and solid nature, or histopathologically, where the lesion is characterized as capsular and fibrotic, allows us to conclude its classification as aseptic fibrotic. Therefore, it can be said that this diagnosis is an accidental finding, since what motivated the patient’s search for health care was the emergence of a recently developed periprosthetic hip infection. Suh et al. described a case of a gossypiboma following a textiloma-induced pathological fracture of the proximal femur 60 years after surgical treatment [9]. Malot and Meena reported a gossypiboma following a femoral shaft fracture surgery of a child undergoing open reduction and internal fixation. Twenty years after surgery, he had a gossypiboma-induced lytic femoral lesion [10]. In a clinical condition also located in the thigh, following a failure of plate and screw femoral diaphysis fracture osteosynthesis, Arora and Johal published a case of aseptic fibrous gossypiboma [11]. Iwase et al. reported a case associated with hip hemiarthroplasty, diagnosed 12 years after surgery following an accidental fall leading to the chronic hip pain onset [12]. Wui et al. also reported a case associated with hip hemiarthroplasty. (Table 1) It can be stated that most textiloma cases found in orthopedic surgery are aseptic fibrous type and usually accidental findings, several years after the initial surgery, which is usually in an urgent context. Our case, to date, as well as the literature reviewed, appears to be the only case reported associated with THA, as well as being an accidental finding discovered following a periprosthetic infection. Imaging plays an essential role in the diagnosis of gossypiboma. The presence of suggestive changes on plain radiographs is not always present. The most frequent radiographic finding is a soft-tissue shadow [8,13], sign that was present in our case. However, the presence of this finding does not allow to make the diagnosis. Calcifications or the presence of a radiographic marker present in a dressing may be other findings [7,13]. The methods of diagnostic choice for textiloma are ultrasound, CT, and magnetic resonance imaging. Ultrasound findings are characterized by the presence of a well-defined formation with posterior shadow and the central presence of hyperechogenic and hypoechogenic zones. In CT, the spongiform and heterogeneous appearance of the mass content with a well-defined and thick contour is the most frequently observed change [7, 13, 14]. These changes described in the literature are similar with the findings found in the clinical case described.
The presence of a surgical scar associated with an underlying swelling should always suggest in the differential diagnosis the hypothesis of gossypiboma. On the other hand, prevention should be the cornerstone addressing this type of occurrence. Swabs count as well as the use of contrast swabs is essential to prevent this operative complication.
The presence of a surgical scar associated with an underlying swelling should always suggest in the differential diagnosis the hypothesis of gossypiboma.
References
- 1.Cima RR, Kollengode A, Garnatz J, Storsveen A, Weisbrod C, Deschamps C. Incidence and characteristics of potential and actual retained foreign objectevents in surgical patients. J Am Coll Surg 2008;207:80-7. [Google Scholar]
- 2.Rappaport W, Haynes K. The retained surgical sponge following intra-abdominal surgery. Arch Surg 1990;125:405-7. [Google Scholar]
- 3.Uchida K, Nakajima H, Yayama T, Hirai T, Chen K, Guerrero AR, Baba H. Unusual foreign body granuloma (gauzoma) found 46 years after open reduction and fixation surgery for femoral shaft fracture. Joint Bone Spine 2010;77:486-7. [Google Scholar]
- 4.Akhaddar A, Baallal H, Elktaibi A. Abscess due to textiloma (gossypiboma: Retained surgical cottonoid). Surg Neurol Int 2018;9:70. [Google Scholar]
- 5.Wan W, Le T, Riskin L, Macario A. Improving safety in the operating room: A systematic literature review of retained surgical sponges. Curr Opin Anaesthesiol 2009;22:207-14. [Google Scholar]
- 6.Liessi G, Semisa M, Sandini F, Roma R, Spaliviero B, Marin G. Retaines surgical gauzes: Acute and chronic CT e US findings. Eur J Radiol 1989;9:182-6. [Google Scholar]
- 7.Olnick HM, Weens HS, Rogers JV Jr. Radiological diagnosis of retained surgical sponges. JAMA 1995;159:1525-7. [Google Scholar]
- 8.Kopka L, Fischer U, Gross AJ, Funke M, Oestmann JW, Grabbe E. CT of retained surgical sponges (textilomas): Pitfalls in detection and eveluation. J Comput Assist Tomogr 1996;2:919-23. [Google Scholar]
- 9.Suh DH, Yoon JR, Kang KB, Han SB, Kim HJ, Lee SJ. A gossypiboma-induced pathological fracture of the proximal femur. Clin Radiol 2009;64:1132-5. [Google Scholar]
- 10.Malot R, Meena DS. Gossypiboma of the thigh mimicking soft tissue sarcoma: case report and review of literature. J Orthop Case Rep 2012;2:21-4. [Google Scholar]
- 11.Arora R, Johal K. Gossypiboma in thigh case report. J Orthop Case Rep 2014;4:22-4. [Google Scholar]
- 12.Iwase T, Ozawa T, Koyama A, Satake K, Tauchi R, Ohno Y. Gossypiboma (foreign body granuloma) mimicking soft tissue tumor with hip hemiarthroplasty. J Orthop Sci 2007;12:497-501. [Google Scholar]
- 13.Lu YY, Cheung YC, Ko SF, Ng SH. Calcified reticulate rind sign: A characteristic feature of gossypiboma on computed tomography. World J Gastroenterol 2005;11:4927-9. [Google Scholar]
- 14.Kalovidouris A, Kehagias D, Moulopoulos L, Gouliamos A, Pentea S, Vlahos L. Abdominal retained surgical sponges: CT appearance. Eur Radiol 1999;9:1407-10. [Google Scholar]
- 15.Wui NG, Ariff MA, Rani RA, Yahaya NH. Retained fragment of surgical gauze in hip arthroplasty case report and literature review. Brunei Int Med J 2017;13:207-10. [Google Scholar]