This case highlights long-term natural history of neglected post-tuberculous affection of thoracolumbar region of vertebral column and management challenges of severe thoracolumbar kyphosis.
Dr. Dhaarani Jayaraman,
Department of Pediatrics, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
E-mail: dhaaranij@yahoo.com
Introduction: Osteosarcoma (OS) is one of the most common primary malignant bone tumors in children and adolescents. OS incidence varies significantly with age and peak incidence is in adolescent age group. Telangiectatic osteosarcoma (TOS) is an unusual variant of OS, forming 3–10% of all OSs. Only few case reports of this rare variant of OS are described in the literature.
Case Report: We report a 6-year-girl who presented with fracture of the left proximal humerus after a trivial trauma. X-ray left shoulder showed osteolytic lesions in the left proximal humerus with fracture of proximal humerus. Open biopsy from the left proximal humerus osteolytic lesion suggested clusters of highly atypical cells like osteoid material and focal areas of hemorrhage and necrosis suggestive of TOS. The child was started on chemotherapy followed by limb-salvage surgery with wide resection of the tumor in the left proximal humerus. She completed her adjuvant chemotherapy and is currently doing well for the past 4 years.
Conclusion: OS occurs more frequently in adolescents around the knee in the metaphyses. The most common histologic type is osteoblastic/fibroblastic or chondroblastic type. Very few cases have been reported in <5 years age group and it’s relatively rare in 5–10-year-old children. Rare histologic variants, especially telangiectatic variant, are more common in younger children and occur more in upper limbs. Imaging reveals mainly osteolytic lesions, unlike in conventional OS. This case highlights the utmost role of histopathology in the diagnosis of the bone tumors which would guide the management appropriately.
Keywords: Osteosarcoma, pathological fracture, expansile lytic lesion, telangiectatic osteosarcoma.
Osteosarcoma or osteogenic sarcoma (OS) is a primary intramedullary high-grade malignant tumor in which the neoplastic cells produce osteoid[1]. Telangiectatic osteosarcoma (TOS), a rare histological variant, is characterized by multiple, aneurysmally dilated, blood-filled cavities with high-grade sarcomatous cells in the peripheral rim and septae. Identification of the unique histologic and radiographic features of TOS is crucial for correct diagnosis, as often, TOS can be easily confused with aneurysmal bone cyst (ABC), both radiologically and pathologically. Misdiagnosis always results in delay in initiation of proper therapy and potentially affects the prognosis[2].
Herewith, we are describing a 6-year-old child who presented with fracture of the left proximal humerus following a trivial trauma and had an expansile lytic lesion on imaging. Since OS is extremely rare in children ≤5 years of age, we sought to review the literature regarding tumor characteristics, treatment strategies, and differences in the outcome in pediatric population.
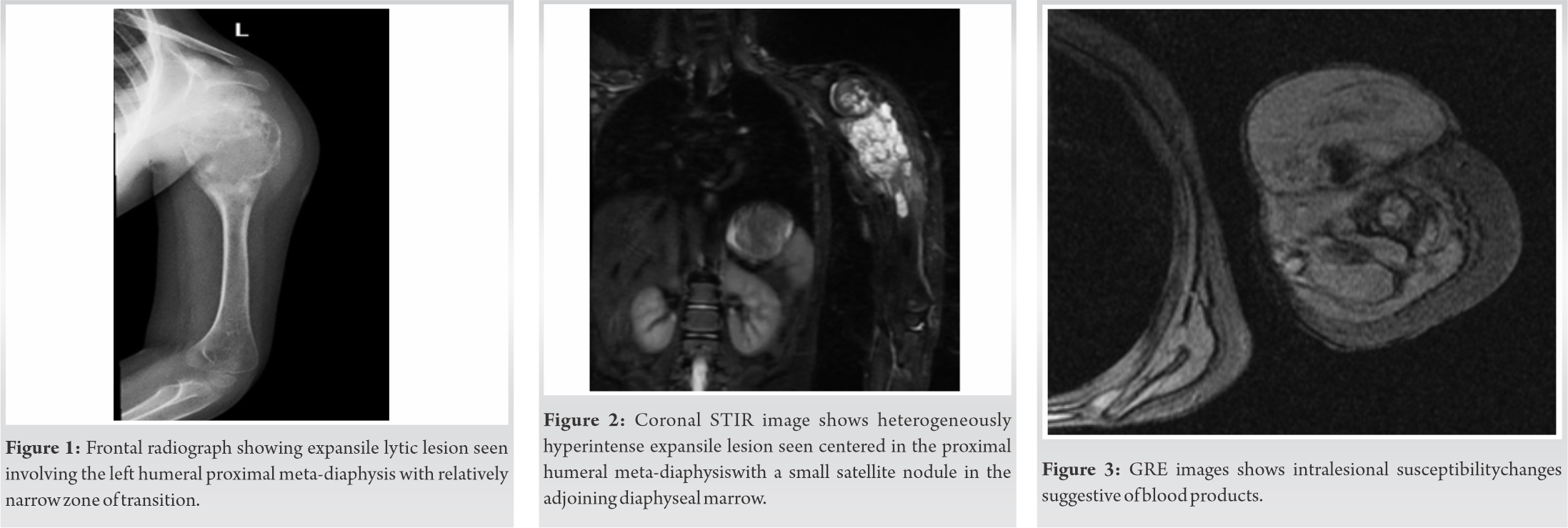
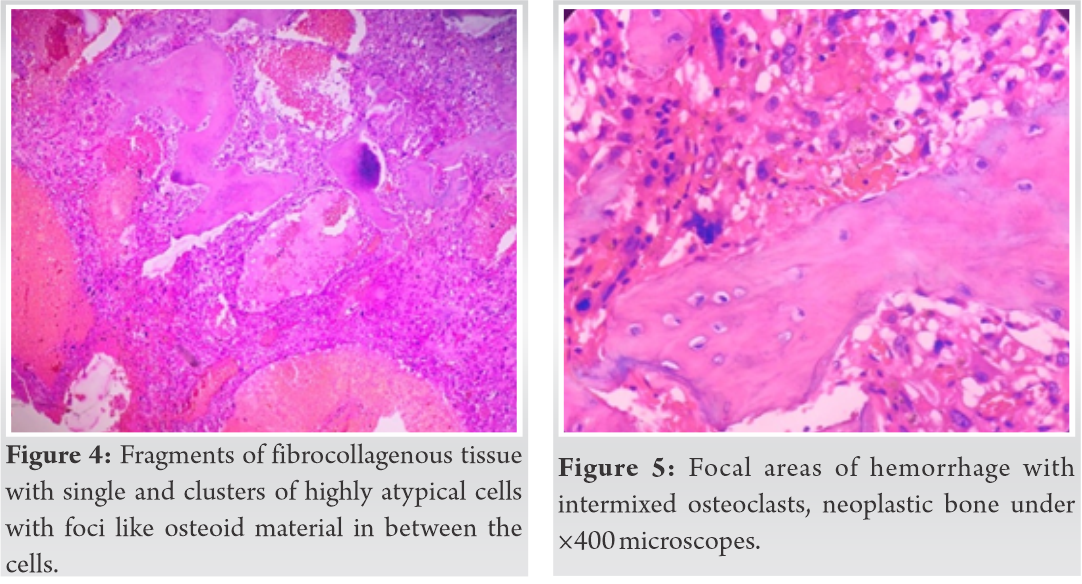
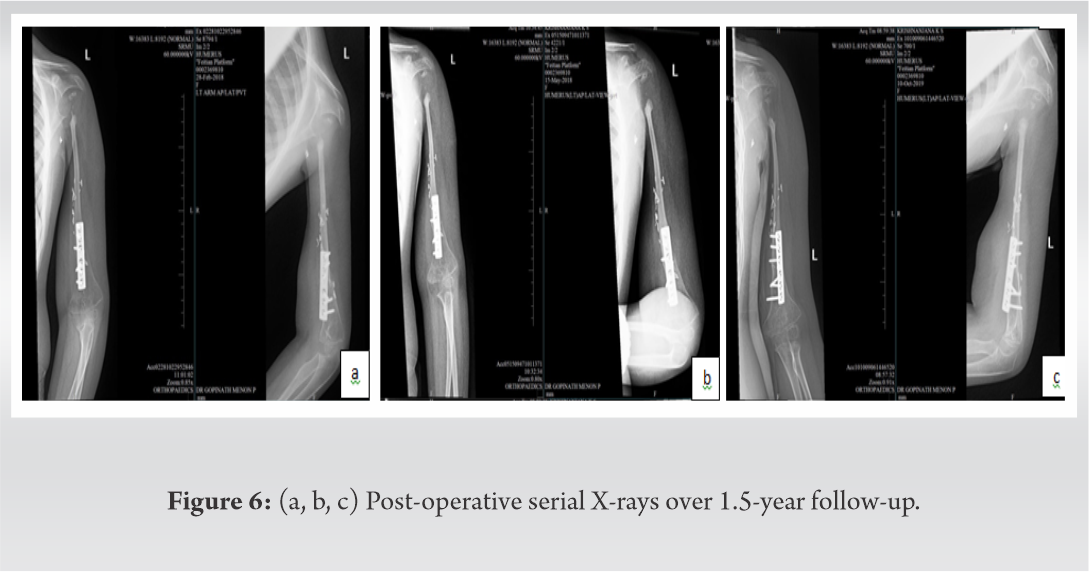
A 6-year-old girl presented to us with swelling of her left arm after trivial fall and apparent injury to her left arm. On examination, the child had a swelling with tenderness of her left arm around the shoulder joint with restriction of movement. The child was treated earlier with splinting for 6 weeks by a traditional bone setter. The child had no history of fever, loss of weight, or loss of appetite. X-ray left shoulder showed osteolytic lesion in the left proximal humerus with fracture of proximal humerus (Fig. 1). Magnetic resonance imaging (STIR and GRE, axial and coronal) showed a large expansile heterogeneous mass lesion involving the epi-, meta-, and diaphyseal regions of the left proximal humerus measuring 5.4 × 4.8 × 10.6 cm (anteroposterior×transverse×craniocaudal) (Fig. 2). The lesion had blood fluid levels, diffusion restriction, and moderate heterogeneous enhancement on post-contrast images (Fig. 3).
The child underwent open biopsy from the left proximal humerus osteolytic lesion and histopathology suggested fibrocollagenous tissue encompassing single and clusters of highly atypical cells with foci like osteoid material in between the cells having focal areas of hemorrhage and necrosis. Hence, a diagnosis of TOS was made. By immunohistochemistry, ki-67 index was 40% in the highest areas and p53 was negative (Fig. 4, 5, 6).
Positron emission tomography-computed tomographydone for staging revealed a mildly 18-fluorodeoxyglucose (FDG) avid expansile lytic lesion (standardized uptake valuemax –6.03) involving the proximal epiphysis, metaphysis, and diaphysis of the left humerus (length 88 mm) with secondary cortical disruption and associated soft-tissue component and non-FDG avid lymph node (7 × 7 mm) in the left axilla. There were no distant metastatic lesions elsewhere.
Chemotherapy was initiated as per children’s oncology group (COG – EURAMOS-1, COG AOST 0331) protocol with high-dose methotrexate, cisplatin, and doxorubicin (MAP regimen). The child underwent 2 cycles of neoadjuvant chemotherapy followed by limb-salvage surgery with wide resection of the tumor in the left proximal humerus (1–3cm tumor-free margin) and reconstruction with vascularized fibular graft with plate osteosynthesis and closure. Post-operative histology revealed TOS with 40% necrosis and 60% hemorrhage and margins were free of tumor. She was continued on adjuvant chemotherapy with intensified MAPIE regimen (MAP+ifosfamide and etoposide) as the percentage of tumor necrosis was <90%. She completed 7 adjuvant cycles of chemotherapy with appropriate monitoring for cardiac function, hearing, and renal functions. She is on regular follow-up for 4 years post-treatment and is in remission. She is able to use the limb for daily activities with mild restriction of movements. The post-operative X-rays are shown in (Fig.6a, b, c).
OS is one of the most common primary malignant bone tumors in children and adolescents. The peak incidence coincides with the pubertal growth spurt in adolescents. Inactivation of p53 gene is one of the most important factors associated with OS. Most common clinical features include pain and swelling at the local site (80–90%) followed by pathological fracture and joint effusions. Approximately 15–20% of children present with metastasis at diagnosis. Malignant osteoid formation is the characteristic histological feature in OS. OS is classified into histological variants which include classic (osteoblastic, fibroblastic, and chondroblastic), telangiectatic, parosteal, periosteal, and small cell variant.
TOS is an unusual variant of OS, forming 3–10% of all OSs[3]. TOS is characterized by multiple, aneurysmally dilated, blood-filled cavities with high-grade, sarcomatous cells in the peripheral rim and septae[4].There is a male predominance, with a male-to-female ratio of 2:1.
OS is extremely rare in patients 5years of age or younger [3]. The median age at presentation is 17.5 years and ranges from 15 to 20 years. The incidence of OS in <5 years age group and 5–9 years age group has been reported as 0.4/million and 2.4million cases/year, respectively [4]. Of the 2706 patients retrospectively analyzed by Cooperative Osteosarcoma Study Group, 28 children (1%) were very young (<5 years), of whom 22.2% had telangiectatic histology [5].OS in very young children has been reported to have predilection for upper limbs and to have telangiectatic histology (10% vs. 2.9%) compared to older children [2]. The least age of TOS reported is that of a 10-month-old infant who presented with a rib mass [6].
The most common location at presentation is the metaphyses of long bones most common being distal femur, followed by proximal tibia, proximal humerus, proximal femur, pelvis, skull bones, and ribs [7]. This distribution pattern holds true for the TOS variant, as well.
TOS was first described by Paget in the year 1854. Originally, it was considered to be a malignant bone aneurysm. Ewing considered this entity as a variant of OS. Children with TOS are at a higher risk of pathologic fractures than patients with conventional OS, as shown in a study done by Huvos et al. which revealed 29% of cases presenting with pathological fractures during initial presentation, however, the impact of pathologic fractures on the outcome of patients with TOS is unknown [8].
TOS is characterized radiologically and histologically based on these features – predominantly expansile lytic lesion with minimal sclerosis, grossly cystic medullary mass radiologically, and bone forming tumor with blood filled spaces lined by malignant cells with limited osteoid formation[9].
Histologically, TOS has to be differentiated from ABC and giant cell tumor. ABC is an expansive destructive, hemorrhagic, tumor-like condition and is a benign reactive vascular process. Both ABC and TOS resemble each other histopathologically, but unlike TOS, mesenchymal stromal cells in ABC are benign in nature. Central giant cell granuloma and central giant cell tumor does not show large sinusoidal spaces [9]. In the present case, there was presence of blood-filled spaces with delicate calcified osteoid like areas and anaplastic tumor cells.
Historically, the surgical treatment of patients with OS and pathologic fractures was immediate amputation. With the recent advent of pre-operative neoadjuvant chemotherapy, limb-salvage surgery has gained popularity for these patients. The regimens including high-dose methotrexate as in EURAMOS protocol, which is used for our patient, though carry short-term toxicities, have impacted the limb salvage and hence the quality of life in these children better. Such an approach, although it is associated with a small increased risk of local recurrence, has not been found to compromise the overall survival of patients [10]. Our patient underwent neoadjuvant chemotherapy followed by limb-salvage surgery and is currently doing well for 4 years after treatment.
The earlier concept that TOS variant has poor prognosis compared to conventional variant is not consistently reported and the prognosis remains the same as in other histological variants depending on chemosensitivity determined by the necrosis and metastasis at diagnosis. In a study done by Tomar et al., prevalence of lung metastasis at diagnosis was 11.5% and 69.2% of TOS patients died of lung metastases within 5 years of follow-up with the implementation of neoadjuvant chemotherapy, suggesting a poor prognosis for patients with TOS [11]. However, in our case, the child did not have lung metastasis.
TOS is very rare in children, however, constitutes a significant proportion of OS in very young children. Many case reports have revealed that misdiagnosed TOS as ABC led to delay in diagnosis and, hence, the outcomes in these children. Hence, TOS should be kept as a differential diagnosis in children presenting with pathological fractures with an expansile lytic lesion. Treatment in the form of intensified neo-adjuvant multiagent chemotherapy and limb-salvage procedures could improve the outcome and lead to good quality of life in young children.
High index of suspicion is important to consider such rare variants of common tumors, especially in young children. Well-coordinated multidisciplinary team management including pediatric oncologists, orthopedic surgeons, surgical oncologists, pathologists, radiologists, physiotherapist, and occupational therapists would help in a holistic care to these patients to provide a good quality of life.
References
- 1.Murphey M, wan Jaovisidha S, Temple H, Gannon F, Jelinek J, Malawer M. Telangiectatic osteosarcoma: Radiologic-pathologic comparison. Radiology 2003;229:545-53. [Google Scholar]
- 2.Worch J, Matthay K, Neuhaus J, Goldsby R, DuBois S. Osteosarcoma in children 5 years of age or younger at initial diagnosis. Pediatr Blood Cancer 2010;55:285-9. [Google Scholar]
- 3.Sangle N, Layfield L. Telangiectatic osteosarcoma. Arch Pathol Lab Med 2012;136:572-6. [Google Scholar]
- 4.Liu JJ, Liu S, Wang JG, Zhu W, Hua YQ, Sun W, et al. Telangiectatic osteosarcoma: A review of literature. Onco Targets Ther 2013;6:593-602. [Google Scholar]
- 5.Kager L, Zoubek A, Dominkus M, Lang S, Bodmer N, Jundt G, et al. Osteosarcoma in very young children: Experience of the cooperative osteosarcoma study group. Cancer 2010;116:5316-24. [Google Scholar]
- 6.Cepeda ML, Sosa AJ, Mora G. Osteosarcoma telangiectásico en un lactante [Telangiectatic osteosarcoma in an infant]. Bol Med Hosp Infant Mex 2017;74:60-4. [Google Scholar]
- 7.Rosen G, Huvos AG, Marcove R, Nirenberg A. Telangiectatic osteogenic sarcoma. Improved survival with combination chemotherapy. Clin Orthop Relat Res 1986;207:164-73. [Google Scholar]
- 8.Huvos AG, Rosen G, Bretsky SS, Butler A: Telangiectatic osteogenic sarcoma: a clinicopathologic study of 124 patients. Cancer 49: 1679–1689, 1982 Matsuno T, Unni KK, McLeod RA, Dahlin DC. Telangiectatic osteogenic sarcoma. Cancer 1976; 38: 2538-47. [Google Scholar]
- 9.Weiss A, Khoury JD, Hoffer FA, Wu J, Billups CA, Heck RK, et al. Telangiectatic osteosarcoma: The St. Jude Children’s Research Hospital’s experience. Cancer 2007;109:1627-37. [Google Scholar]
- 10.Tomar D. Central telangiectatic osteosarcoma of the mandible in a paediatric patient: A rarity. J Clin Diagn Res 2016;10:XD01-3. [Google Scholar]