This case highlights long-term natural history of neglected post-tuberculous affection of thoracolumbar region of vertebral column and management challenges of severe thoracolumbar kyphosis.
Dr. Nandan Marathe,
Saraswati Prasad, Gaul Wada, Vasai (West), Palghar – 401 201, Maharashtra, India. India.
E-mail: nandanmarathe88@gmail.com
Introduction: Thoracolumbar kyphosis is common cause of sagittal spinal malalignment. Neglected tuberculous infection in childhood often presents as kyphotic deformity in adulthood, especially in India, where tuberculosis is endemic. Complete clinical and radiological evaluation is necessary to decide need for surgical intervention. We came across this case of severe thoracolumbar kyphosis extending into lower lumbar spine due to block vertebra formation from fusion of T12 to L4 vertebrae.
Case Report: The patient presented with debilitating mechanical low back pain without any neurological abnormality in lower limb. The patient was treated surgically with posterior corrective three-column osteotomy and fixation in view of the persistent mechanical low back pain. At 1-year follow-up, the patient showed significant improvement in low back disability score.
Conclusion: After performing three-column osteotomy, we obtained 63% correction in thoracolumbar kyphosis resulting in relief of symptomatic severe axial low back pain and ambulatory capacity with Oswestry Disability Score of 10%. This case highlights long-term natural history of neglected post-tuberculous affection of thoracolumbar region of vertebral column and management challenges of severe thoracolumbar kyphosis.
Keywords: Kyphosis, thoracolumbar, spinal osteotomy.
Sagittal alignment of spine is important for maintaining erect posture with little muscular effort [1]. Sagittal alignment is taken into utmost consideration in spinal deformity correction surgeries for a good short- and long-term outcome [2]. Kyphotic deformity in adulthood can be a result of either a pediatric pathology or may be related to pathology arising in adulthood. These include senile kyphosis due to osteoporotic burst fracture, post-laminectomy syndrome, neurofibromatosis, ankylosing spondylitis, and degenerative diseases [3]. Ultimate result of loss of sagittal alignment is pain, cosmetic concerns, and structural instability [2]. Post-tuberculous kyphosis is a major cause of spinal malalignment in Indian population which is often associated with neurodeficit [4]. Surgeons must evaluate the whole spine to restore sagittal balance. This includes finding whether deformity is regional/global or more segmental/focal. Other factors include presence of flexibility of kyphosis. Here, we present a case of severe thoracolumbar kyphosis with rare block vertebra formation due to fusion of T12 to L4 vertebrae, most probably post-tuberculous in nature. The patient was managed with a three-column osteotomy with resultant post-operative deficit which recovered gradually to full recovery over a period of time.
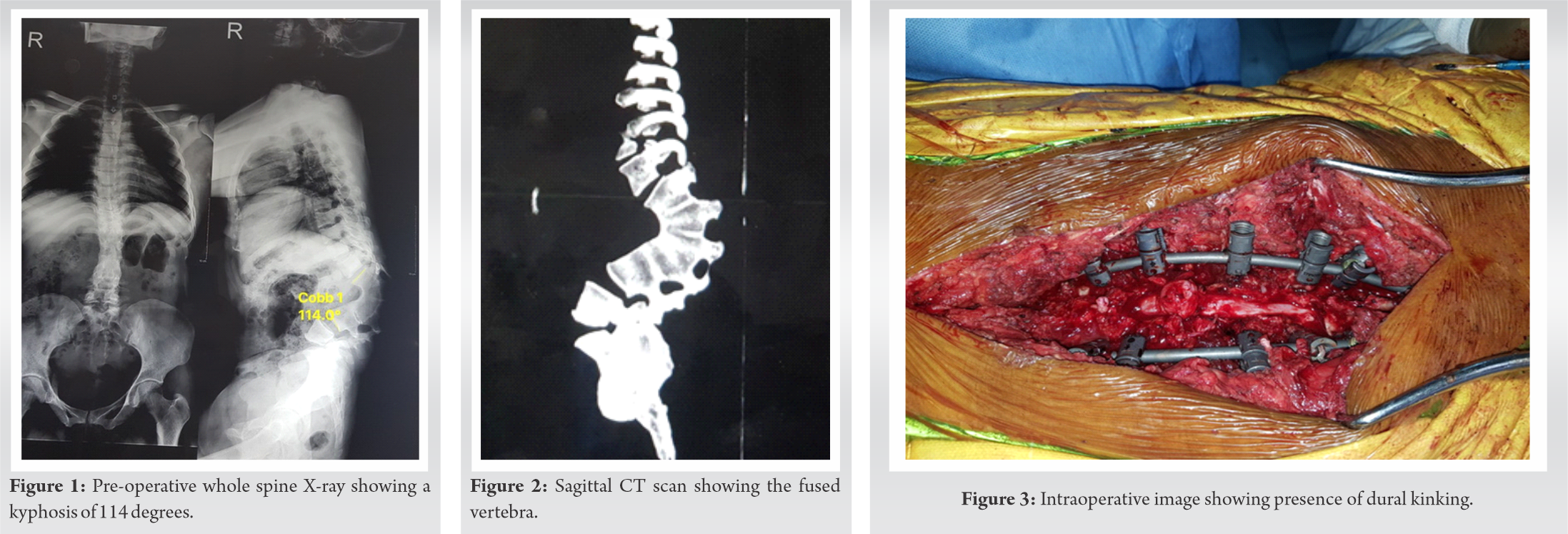
A 32-year-old female presented to our outpatient clinic with inability to lie in supine position due to prominence in her back. She also had severe debilitating axial mechanical back pain. The patient first noticed this deformity 5 years ago and it gradually progressed to present magnitude. However, she reported late due to the social stigma of deformity and did not give any history of childhood infection. Apart from local tenderness and gibbus over lower back, she had normal neurology as per MRC grading in lower limbs with Oswestry disability index (ODI) score of 70%. The visual analog score (VAS) for back pain was 8. Radiographs and computed tomography (CT) scan of thoracolumbar spine showed marked round kyphosis of 114 degrees due to fusion of T12 to L4 vertebrae with corresponding wedging of anterior vertebral bodies (Fig. 1, 2).
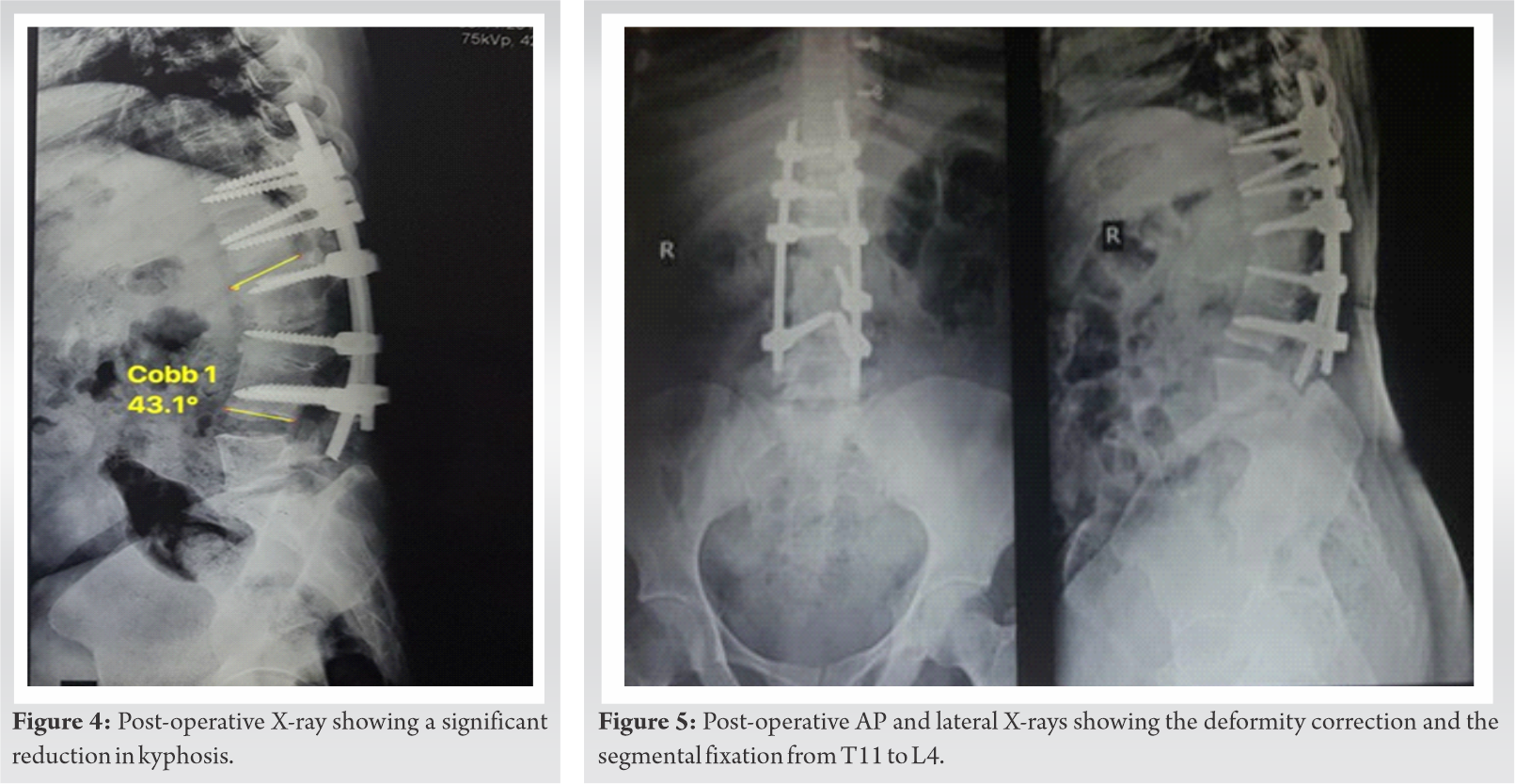
The patient had a positive sagittal imbalance with sagittal vertical axis deviation by 41.6 mm. CT also revealed dysplastic pedicles of L1 and L2 vertebrae. MRI scan revealed spinal cord ending at L2 with no other intraspinal anomaly. Thecal sac was draped over internal gibbus manifested by the deformity. The patient was explained about spinal osteotomy surgery and possible need of another surgery in future to achieve further correction. L2 pedicle subtraction osteotomy (PSO) was planned initially. However, intraoperative correction of thoracolumbar kyphosis was insufficient; hence, PSO involving both L1 and L2 vertebrae was performed and the segmental fixation extended from T11 to L4. Significant dural kinking was noted at level of correction (Fig. 3). Hence, further correction was abandoned. The patient woke up with monoplegia involving right lower limb with normal neurology in the left lower limb. Post-operative CT scan showed medial breach of the right L3 pedicle screw. The patient was taken to operating room immediately and right side L3 pedicle screw was removed. Post-operative day 2, the patient started showing brief ankle movement with significant spasticity in the right lower limb which improved over a period of 1 month to normal neurology as per MRC grading. VAS score for back pain improved to 2 on 14th post-operative day. Follow-up X-ray at 6 months showed fusion at osteotomy site (Fig. 4, 5). At present, the patient has been mobilized without any assistive device with a 1-year follow-up duration. The ODI at 1-year follow-up is 10% with no back pain.
Importance of sagittal plane balance in spine cannot be overemphasized as it is associated with a good long-term functional outcome. The most common pathology responsible for kyphosis in adulthood are continuation of childhood kyphosis such as congenital kyphosis, Scheuermann’s kyphosis, or new occurrence due to fractures involving thoracolumbar region, post-laminectomy, and iatrogenic flat back deformity following segmental instrumentation [5]. Although degenerative pathologies or systemic pathologies like ankylosing spondylitis are most common in western half of world, infectious pathologies predominantly tuberculosis is leading cause of kyphosis in developing world [6]. Unfortunately, large portion of these tuberculosis cases remains untreated and present late in adulthood. The most common reason for their presentation in adulthood are late onset paraplegia due to compressive myelopathy or severe axial back pain due to kyphosis-induced unfavorable sagittal imbalance [7, 8, 9]. Distinction should be made while evaluating kyphotic deformities, whether they are global or regional. Well-balanced global kyphosis deformities may not require any intervention or only isolated posterior column osteotomies may suffice in such cases [10]. In contrast, segmental fixed sagittal kyphosis may require anterior column intervention in the form of PSO or VCR depending on correction desired [11]. Flexibility of kyphotic curve should also be taken into consideration. Flexible curve can just be corrected with cantilever maneuver without need of osteotomy. In our case, there was fusion involving T12 to L4 leading to significant segmental sagittal imbalance [5]. However, due to the presence of mobile L4-L5 and L5-S1 disc which normally contributes maximally for lumbar lordosis, compensated the deformity and maintained lordosis to 41.1 degree. These values have been calculated with imaginary superior L1 end plate due to absence of mobile T12-L1 disc space. Thoracolumbar kyphosis changed from pre-operative value of 114 to 43 degrees following three-column osteotomy involving wedge resection of L1 and L2 vertebra. This resulted in disappearance of clinical gibbus in thoracolumbar region and the patient could lie in supine position comfortably which was not possible preoperatively. Neurological complication rate reported in literature following lumbar PSO is around 11 % which includes both temporary and permanent weakness [12]. In our case, it is violation of medial pedicle breach rather than dural kinking, which could have been responsible of neurological deficit as it was unilateral in nature. The patient showed picture of conus medullaris syndrome as there was spasticity in the right lower limb. This could have resulted due to low lying conus reaching up to L2 vertebra where osteotomy was performed. The patient recovered neurology within 1 month completely with residual minimal spasticity which disappeared over a period of 1 year. Post-tuberculous deformity is commonly seen in thoracic spine or thoracolumbar region [13]. It is rare to see such extensive involvement of lumbar spine till L4 vertebra starting from thoracolumbar region. These patients usually develop coexisting myelopathy due to internal draping of spinal cord over internal gibbus in narrow thoracic spinal canal leading to occurrence of late onset paraplegia. In our case, as deformity involved spacious lumbar spine with cord ending at L2, the patient was disabled with predominant axial back pain and had no evidence of neurological disturbance preoperatively. We assume this deformity to be post-tuberculous based on geographical prevalence and pattern of deformity. Most common variety of spinal tuberculosis is paradiscal in nature with contiguous vertebral involvement [4, 14]. This leads to destruction of disc space and wedging of vertebral bodies due to destruction of end plates. This culminates into progression of kyphosis in affected region of vertebral column similar to above-mentioned deformity which showed kyphosis with wedging of L1-L2 vertebral bodies. After performing three-column osteotomy, we obtained 63% correction in thoracolumbar kyphosis resulting in relief of symptomatic severe axial low back pain and ambulatory capacity with ODI score of 10% [15].
This case highlights long-term natural history of neglected post-tuberculous affection of thoracolumbar region of vertebral column and management challenges of severe thoracolumbar kyphosis.
This case highlights long-term natural history of neglected post-tuberculous affection of thoracolumbar region of vertebral column and management challenges of severe thoracolumbar kyphosis.
References
- 1.Bhosale S, Pinto D, Srivastava S, Purohit S, Gautham S, Marathe N. Measurement of spinopelvic parameters in healthy adults of Indian origin–A cross sectional study. Journal of Clinical Orthopaedics and Trauma. 2020 Sep 1;11(5):883-8. [Google Scholar]
- 2.Macagno AE, O’Brien MF. Thoracic and thoracolumbar kyphosis in adults. Spine (Phila Pa 1976) 2006;31:S161-70. [Google Scholar]
- 3.Winter RB, Lonstein JE, Anderson M. Neurofibromatosis hyperkyphosis: A review of 33 patients with kyphosis of 80 degrees or greater. J Spinal Disord 1988;1:39-49. [Google Scholar]
- 4.Rajasekaran S. Kyphotic deformity in spinal tuberculosis and its management. Int Orthop 2012;36:359-65. [Google Scholar]
- 5.Yaman O, Dalbayrak S. Kyphosis and review of the literature. Turk Neurosurg 2014;24:455-65. [Google Scholar]
- 6.Bhosale S, Prabhakar A, Srivastava S, Raj A, Purohit S, Marathe N. Pattern of drug resistance in primary spinal tuberculosis: A single-center study from India. Glob Spine J 2020;??? :2192568220941445. [Google Scholar]
- 7.Srivastava S, Marathe N, Bhosale S, Purohit S, Raj A, Amin A, et al. Golden wires and rectangle: A cost-effective treatment for tuberculosis of the thoracic spine. Asian J Neurosurg 2020;15:328-32. [Google Scholar]
- 8.Jain AK, Jena AN, Dhammi IK, Kumar S. Fate of intervertebral disc space in paradiscal tuberculous lesions. Indian J Orthop 1999;33:90-4. [Google Scholar]
- 9.Tuli SM. Severe kyphotic deformity in tuberculosis of the spine. Int Orthop 1995;19:327-31. [Google Scholar]
- 10.Diebo BG, Henry J, Lafage V, Berjano P. Sagittal deformities of the spine: Factors influencing the outcomes and complications. Eur Spine J 2015;24:S3-15. [Google Scholar]
- 11.Bridwell KH, Lewis SJ, Lenke LG, Baldus C, Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am 2003;85:454-63. [Google Scholar]
- 12.Bridwell KH, Lewis SJ, Edwards C, Lenke LG, Iffrig TM, Berra A, et al. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine (Phila Pa 1976) 2003;28:2093-101. [Google Scholar]
- 13.Sharma A, Chhabra HS, Chabra T, Mahajan R, Batra S, Sangondimath G. Demographics of tuberculosis of spine and factors affecting neurological improvement in patients suffering from tuberculosis of spine: A retrospective analysis of 312 cases. Spinal Cord 2017;55:59-63. [Google Scholar]
- 14.Rathod TN, Sathe AH, Marathe NA. Response to letter to the editor on “it’s never too late: Neurological outcome of delayed decompression in tuberculosis of spine”. Glob Spine J 2021;11:420-1. [Google Scholar]
- 15.Fairbank JC, Pynsent PB. The Oswestry disability index. Spine (Phila Pa 1976) 2000;25:2940-52. [Google Scholar]