While functional outcomes of perilunate dislocations are poor, operative fixation through open reduction internal fixation with ligamentous repair is necessary to maximize return of function in the acute setting following injury.
Dr. Nicholas Frane,
Department of Orthopaedic Surgery, Zucker School of Medicine at Hofstra/Northwell, Plainview, New York, United States.
E-mail: nicholasfrane@gmail.com
Introduction: Perilunate dislocations are rare high-energy injuries, and the diagnosis is not infrequently missed at initial presentation. The combination of fractures resulting in a trans-styloid, trans-scaphoid, and trans-triquetral perilunate fracture dislocation is extremely rare. Early recognition and diagnosis of these injuries is prudent to restore patient function and prevent morbidity. This injury pattern may progress through several distinct phases often involving the greater or lesser arc. The injury begins with traumatic disruption of the scapholunate joint, followed by an ordered progression of injury to the capitolunate, lunotriquetral, and radiolunate joints. When the radiolunate joint is disrupted, the lunate often dislocates volar transposing into the carpal tunnel, associated with median nerve compression. These injuries have the potential to cause lifelong disability of the wrist. Early treatment may prevent or lessen the chance of median neuropathy, post-traumatic wrist arthrosis, chronic instability, and fracture nonunion. Non-operative treatment is not indicated and is associated with poor functional outcomes and recurrent dislocation. Open reduction and internal fixation (ORIF) with ligamentous repair after emergent closed reduction and splinting is indicated for acute injuries (<8 weeks after injury).
Case Report: We report a case of a 48-year-old right hand dominant male with a trans-styloid, trans-scaphoid, trans-triquetral, and perilunate dislocation after mechanical fall from height. He was evaluated in the ER and provisionally treated with closed reduction and splinting. ORIF of scaphoid, radial styloid, and triquetrum was performed, with ligamentous repair of the scapholunate joint and carpal tunnel decompression.
Conclusion: The combination of fractures/injuries in this case has been very rarely been published in case reports to date. It is necessary to recognize these wrist injuries. Great detail should be given to physical and radiographic evaluation, as adequate reduction can help prevent median nerve damage and minimize post-injury complications such as cartilage damage, avascular necrosis, chronic pain, and deformity. As most cases present in the acute setting, ORIF and ligamentous repair are most likely to maximize return of function. While operative intervention can help to minimize sequelae, functional outcomes are generally poor following these injuries.
Keywords: Perilunate dislocation, perilunate, Mayfield progression, hand trauma.
Perilunate dislocations are rare high-energy injuries, constituting <10% of all wrist injuries [1]. The diagnosis is often missed on clinical and radiographic evaluation, up to 25% of cases [2]. Early recognition and diagnosis of these injuries is prudent to restore patient function and prevent morbidity. This injury pattern may progress through several distinct phases often involving the greater or lesser arc. The injury begins with traumatic disruption of the scapholunate joint, followed by an ordered progression of injury to the capitolunate, lunotriquetral, and radiolunate joints. When the radiolunate joint is disrupted, the lunate often dislocates volar transposing into the carpal tunnel, associated with median nerve compression, which can be present in up to 25% of these cases [3]. These injuries have the potential to cause lifelong disability of the wrist. Early treatment may prevent or lessen the chance of median neuropathy, post-traumatic wrist arthrosis, chronic instability, and fracture nonunion. Non-operative treatment is not indicated and is associated with poor functional outcomes and recurrent dislocation [4]. Open reduction and internal fixation (ORIF) with ligamentous repair after emergent closed reduction and splinting is indicated for acute injuries (<8 weeks after injury).
A 48-year-old right hand dominant male presented to the emergency department for the right wrist pain. The patient was an out-of-state resident who was visiting the area. He reported that he was up late consuming alcoholic beverages with family members when he remembered suffering a mechanical fall from standing height, during which he caught himself with his right hand. He presented to the ED 9 h later for evaluation with continued pain and decreased function of his right wrist, as well as right ankle pain. The patient has a history of psoriasis and hypertension, alcohol, and tobacco use.
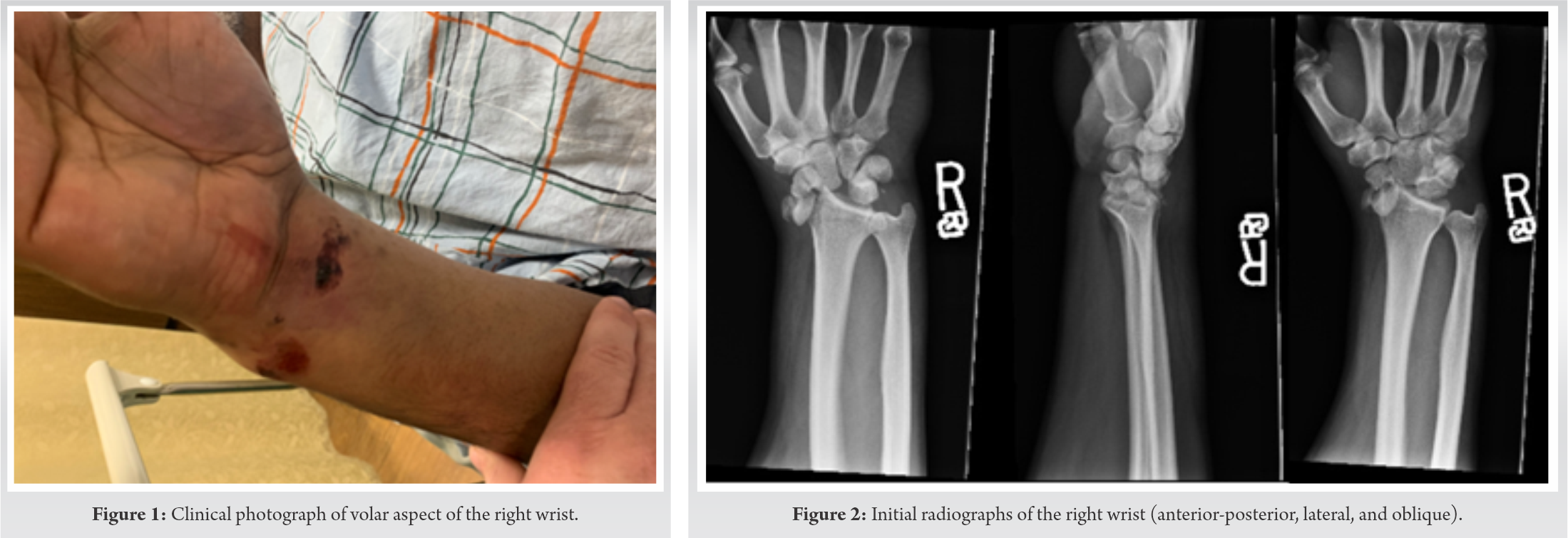
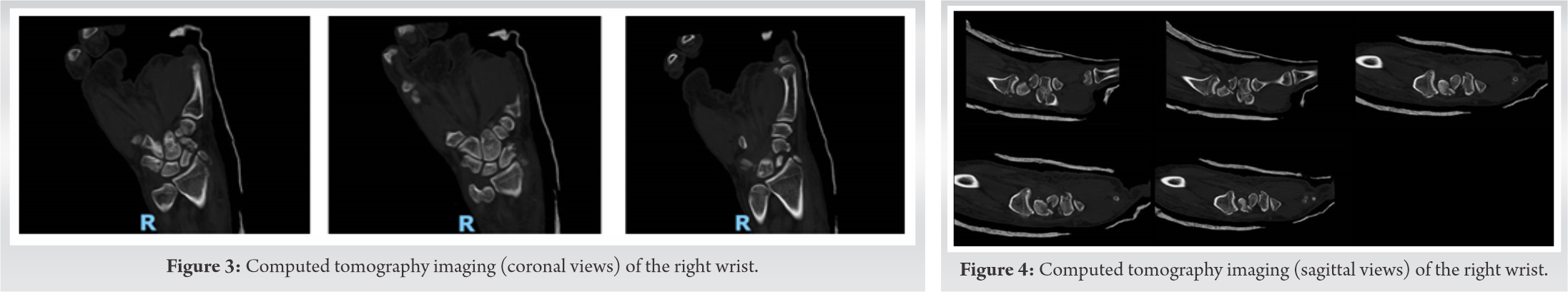
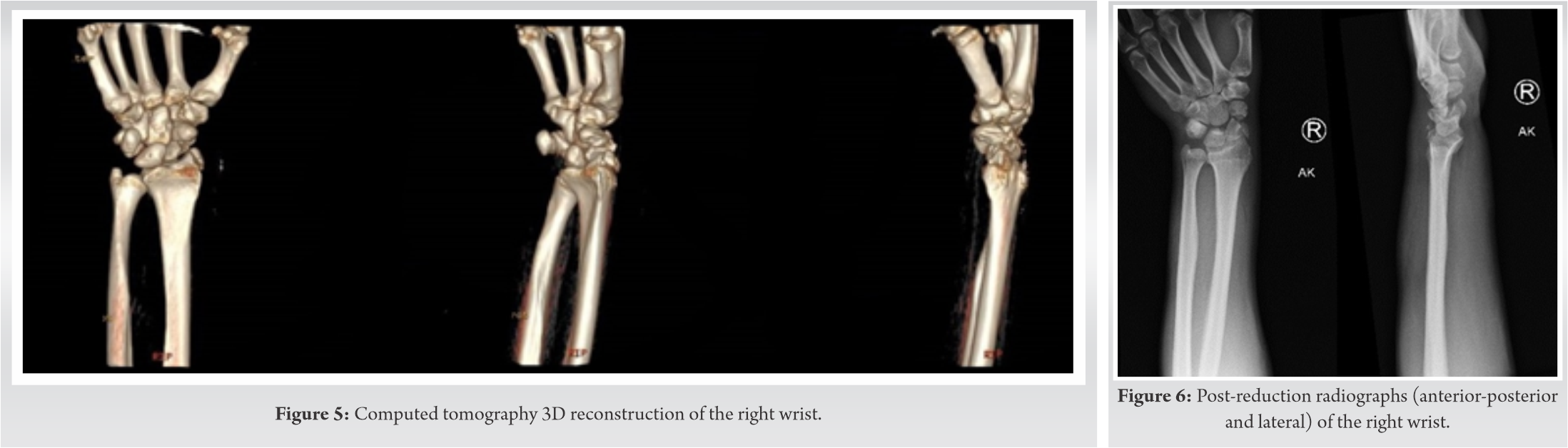
On examination, the patient had an abrasion over the volar aspect of his right wrist with associated swelling, ecchymosis, obvious deformity, and severe tenderness to palpation and range of motion (Fig. 1). He had decreased sensation within the distribution of the median nerve, but all other nerve functions remained intact (including the anterior interosseous nerve, posterior interosseous nerve, ulnar, and radial nerves). Brisk capillary refill was noted. On secondary examination, the patient was noted to have right hip pain with log roll and tenderness over his greater trochanter. Swelling was noted over his right ankle with mild pain to both passive plantar flexion and dorsiflexion. His lower extremities were neurovascularly intact. No other obvious injuries or deformities were found. He was noted to be intoxicated on evaluation. Imaging of his right wrist, right ankle, right hip, and pelvis was obtained. X-rays of his right wrist revealed a trans-radial styloid, trans-scaphoid, trans-triquetral, and perilunate dislocation (Fig. 2). All other imaging were reviewed and found to be negative. Computed tomography (CT) imaging of the wrist was obtained to further classify the injury for pre-operative planning (Fig. 3-5).
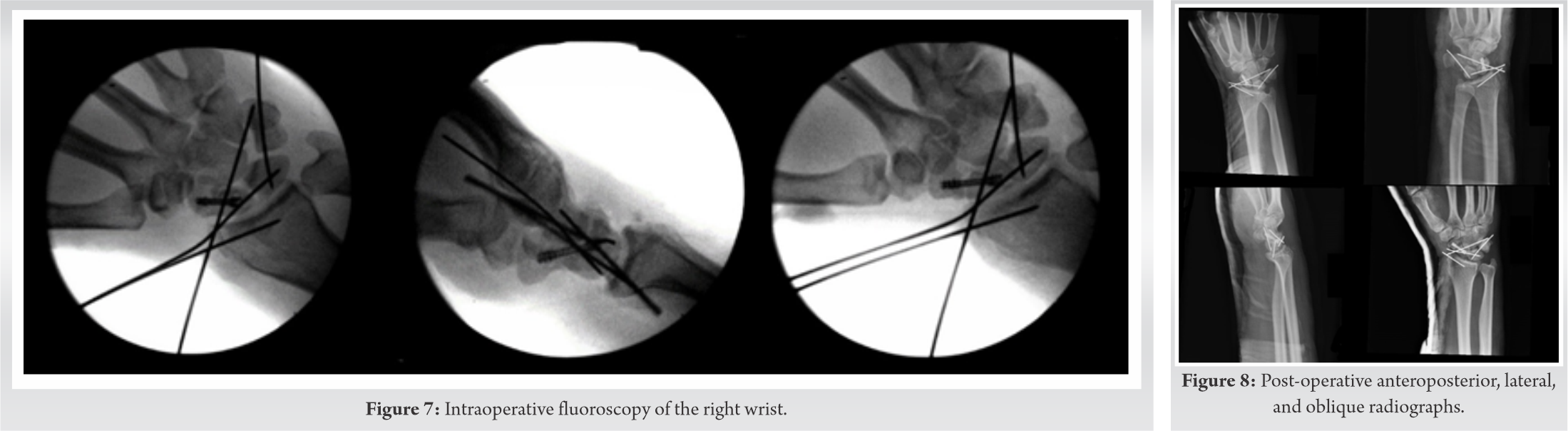
Closed reduction under sedation was obtained on first attempt with reasonable alignment following the use of longitudinal traction for 10 min. Splint was placed for stabilization before definitive management. After post-reduction observation and evaluation, the patient continued to have acute carpal tunnel syndrome and the proximal pole of the scaphoid was still malrotated (Fig. 6). He was taken to the operating room that evening for extended carpal tunnel release, ORIF of the scaphoid, radial styloid, and scapholunate ligamentous repair. A primary proximal row corpectomy would have been considered, but with a radial styloid fracture, the radioscaphocapitate ligament was likely incompetent. A dual incision approach, dorsal and volar, was used to obtain repair. An extended carpal tunnel release was performed. Dorsally, incision was made over the wrist joint extending in line with the third ray. The floor of the third dorsal extensor compartment was incised and the joint capsule was clearly torn. The proximal pole of the scaphoid was completely detached from any soft-tissue fragments. A 0.045 K-wire was placed into the proximal pole to use as a joystick. The scaphoid fracture was reduced and the K-wire was advanced. This was difficult secondary to comminution at the scaphoid waist. A 4 mm × 20 mm headless compression screw was placed in the center-center position through the scaphoid. The scapholunate ligament (SL) was torn off the scaphoid and still attached to the lunate. The patient was also noted to have a lunotriquetral ligament (LT) tear which was also visible on fluoroscopy by widening of the interval. The LT gap was reduced and held in place with a 0.045 K-wire. A K-wire was placed across the SL interval to hold reduction. This pin also served as a buttress force to the radial styloid fragment. A suture anchor was placed in the proximal portion of the scaphoid and the SL ligament was repaired. After this, attention was changed to the radial styloid fracture. A small 1 cm incision was made over the radial styloid and nick and spread technique was used to dissect down to the fracture fragment. The styloid fracture was pinned in place with a K-wire. For further stability, a K-wire was placed from the scaphoid to the capitate (Fig. 7). The wound was irrigated and closed and the patient was placed into a thumb spica plaster splint (Fig. 8).
The patient outcome was evaluated 16 months after index procedure. The patient reported excellent outcome with pin removal at 11 months with imaging performed before removal of hardware (Fig. 9). Standardized subjective scoring measures were obtained including disabilities of the arm, shoulder, and hand (DASH) (5.83/100), patient-rated wrist evaluation (PRWE) (1/100), and SF-12 Health Survey (33/47). DASH and PRWE showed terrific outcome with lower score representing improved outcome, and SF-12 showed moderate outcome with higher score significant for improved outcome. The patient complained of limitations and mild difficulty with recreational activities and moderate stiffness of his wrist. Of note, the patient had recent liver transplant at time of interview and attributed most of his deficits on the SF-12 to his recovery from recent surgery rather than the outcome of his wrist.
Perilunate dislocations are rare, constituting <10% of all wrist injuries, and are associated with poor functional outcomes [1, 2, 3]. These dislocations occur through high-energy injuries through which an axial load is transmitted through the volar aspect of the wrist causing forced extension and ulnar deviation. This injury progresses through several distinct phases, known as the Mayfield progression, and may involve the greater or the lesser arc [5]. Greater arc injuries occur as the force passes through the carpal bones, while the lesser arc pathway consists only of capsuloligamentous involvement. In accordance with the Mayfield staging, the injury begins with disruption of the scapholunate joint, followed by an ordered progression of injury to the capitolunate, lunotriquetral, and radiolunate joints [6, 7]. When the radiolunate joint is disrupted, the lunate may dislocate with volar displacement. This is often associated with median nerve compression, as it transposes into the carpal tunnel. Most commonly, perilunate injuries occur trans-scaphoid, known as a de Quervain injury [8]. They may also present through isolated perilunate dislocation (through lesser arc injuries), trans-radial styloid, or trans-scaphoid-trans-capitate injuries, or some combination of these associated injuries. With regard to greater arc injuries, different forces cause involvement of the carpal bones within the Mayfield progression. The trans-radial component is caused by the stress placed on the radial styloid after a fall on an outstretched hand in ulnar deviation. Fractures of the radial styloid body occur through intense strain on the radioscaphocapitate ligament, whereas radial styloid tip fractures occur through injury of the radial collateral ligament. If associated with a fracture dislocation, involvement of the scaphoid is the most common injury [9, 10]. These usually occur at the middle (waist) of the scaphoid. The trans-capitate component of the injury results from hyperextension of the wrist. As the lunate rotates dorsally, the dorsal lip of the lunate impinges on the body of the capitate, causing a fracture that is usually transverse relative to its long axis. The next part of this sequence, the trans-triquetral component, occurs through an avulsion of the long radiocapitate ligament or the palmar ulnotriquetral ligament. There have been reports of perilunate fractures associated with two components of this pattern, but very few have reported the combination of the carpal fractures and the styloid fracture, we observed in our patient [2, 11, 12]. In our case, the patient suffered a greater arc injury with trans-styloid, trans-scaphoid, and trans-triquetral components. This suggests that our patient sustained his wrist injury by falling on an outstretched hand with ulnar deviation and hyperextension of the carpus. The trans-styloid and trans-triquetral components indicate likely associated ligamentous injury. Majeed and Kumar [13] reported on a trans-styloid, trans-scaphoid, trans-triquetral, and perilunate dislocation, with associated ulnar styloid fracture, that presented 4 weeks after the injury occurred. Morin and Becker [12] reported on a trans-styloid, trans-scaphoid, trans-triquetral, and perilunate dislocation that presented in the acute setting, 4 h after injury. In this case, operative intervention was delayed for 1 week until the swelling subsided. In both of these cases, a higher energy injury occurred as both patients were injured while on their bicycles. When conventional imaging (posteroanterior [PA], lateral, and oblique) is reviewed, several abnormalities may be noted. On PA view, abnormal widening of the scapholunate interval >3 mm (Terry Thomas sign) and loss of normal carpal collinear lines (Giulia lines) are noted [5]. The lunate often appears triangular in appearance, which is known as the “piece of pie sign.” On the lateral view, the “spilled tea cup sign” may be noted with volar dislocation of the lunate [5]. Non-operative treatment is not indicated and is associated with poor functional outcomes and recurrent dislocation. ORIF with ligamentous repair after emergent closed reduction and splinting is indicated for acute injuries (<8 weeks after injury). While return to full function is unlikely, emergent closed reduction decreases risk of median nerve and cartilage damage. For chronic injuries (>8 weeks after injury), proximal row carpectomy or total wrist arthrodesis can be considered. Complications associated with perilunate dislocations include median nerve neuropathy through acute carpal tunnel syndrome which requires surgical release. This occurs in approximately 24–45% of patients and is most common in stage IV injuries in which the lunate dislocates from the lunate fossa into the carpal tunnel [4]. Post-traumatic arthritis, avascular necrosis, and chronic perilunate injury (pain, instability, and deformity) are common complications. Return to full function after perilunate dislocations is uncommon.
Perilunate dislocations should be an important consideration with patients presenting with wrist pain, especially after high-energy trauma. It is necessary to recognize these injuries, as adequate reduction can help minimize post-injury complications such as avascular necrosis. As most cases present in the acute setting, ORIF and ligamentous repair are most likely to maximize return of function. While operative intervention can help to minimize sequelae, functional outcomes are generally poor following these injuries.
It is imperative to identify and properly manage perilunate dislocations to minimize long-term sequelae.
References
- 1.Dobyns JH, Linscheid RL, Cooney WP. Fractures and dislocations of the wrist and hand, then and now. J Hand Surg Am 1983;8:687-90. [Google Scholar]
- 2.Subramanian K, Arora B, Bhatnagar A, Jan I. Perilunate dislocation-case report and review of literature. J Clin Diagn Res 2017;11:RD06-8. [Google Scholar]
- 3.Herzberg G, Comtet JJ, Linscheid RL, Amadio PC, Cooney WP, Stalder J. Perilunate dislocations and fracture-dislocations: A multicenter study. J Hand Surg Am 1993;18:768-79. [Google Scholar]
- 4.Stanbury SJ, Elfar JC. Perilunate dislocation and perilunate fracture-dislocation. J Am Acad Orthop Surg 2011;19:554-62. [Google Scholar]
- 5.Scalcione LR, Gimber LH, Ho AM, Johnston SS, Sheppard JE, Taljanovic MS. Spectrum of carpal dislocations and fracture-dislocations: Imaging and management. Am J Roentgenol 2014;203:541-50. [Google Scholar]
- 6.Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: Pathomechanics and progressive perilunar instability. J Hand Surg Am 1980;5:226-41. [Google Scholar]
- 7.Kennedy SA, Allan CH. In brief: Mayfield et al. Classification: Carpal dislocations and progressive perilunar instability. Clin Orthop Relat Res 2012;470:1243-5. [Google Scholar]
- 8.Melsom DS, Leslie IJ. Carpal dislocations. Curr Orthop 2007;21:288-97. [Google Scholar]
- 9.Cooney WP, Bussey R, Dobyns JH, Linscheid RL. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res 1987;214:136-47. [Google Scholar]
- 10.Frane N, Goldenberg W. Perilunate dislocation. In: Stat Pearls. Treasure Island, FL: Stat Pearls Publishing; 2020. [Google Scholar]
- 11.Soejima O, Iida H, Natio M. Transscaphoid-transtriquetral perilunate fracture dislocation: Report of a case and review of the literature. Arch Orthop Trauma Surg 2003;123:305-7. [Google Scholar]
- 12.Morin ML, Becker GW. An unusual variant of perilunate fracture dislocations. Case Reports Plast Surg Hand Surg 2016;3:7-10. [Google Scholar]
- 13.Majeed SA, Kumar SM. Transstyloid, transscaphoid, transtriquetral perilunate dislocation-a late presentation. Indian J Orthop 2010;44:345-8. [Google Scholar]