Open reduction internal fixation and implant retention is a reasonable alternative surgical strategy in patients’ with extracapsular femoral neck periprosthetic fractures around well- fixed and functioning hip resurfacing arthroplasties.
Dr. Arpit Bakulash Patel,
Department of Trauma and Orthopaedic Surgery,
Barnet Hospital, Royal Free NHS Foundation Trust, London, United Kingdom.
E-mail: a.b.patel@doctors.org.uk
Introduction : Background: Extracapsular femoral neck fractures in the presence of a resurfacing hip arthroplasty (RHA) appear to be independent of suboptimal technique during the initial implantation of the RHA and present with a similar etiology as native hip fractures – that is, a fragility fracture related to pathological or age-related osteoporosis, as a consequence of trauma. In the presence of a well-fixed and previously well-functioning RHA, the options for management include revision arthroplasty or open reduction and internal fixation (ORIF). In the absence of loosening through mechanisms of wear, infection, metallosis, or suboptimal prosthesis positioning, many authors have advocated ORIF with implant retention. However, there is often debate regarding the use of total hip arthroplasty in these cases
Case Report: The authors conducted a thorough assessment of the literature followed by a retrospective review of outcomes for three patients treated by ORIF with implant retention for extracapsular femoral neck fractures around a RHA, using a standardized technique. All patients were independently mobile and active with well-fixed and well-functioning RHAs before the date of injury. All patients suffered low-energy trauma resulting in the fracture. There were no intraoperative or perioperative complications. All patients achieved full weight-bearing status and independent mobility. Two patients achieved radiographic union and returned to full range of movement and independent mobilization comparable to their preoperative state. One patient was lost to follow-up.
Conclusion: The authors believe that fixation of extracapsular proximal femoral fractures distal to a well-fixed, well-functioning RHA is a good management option in an independent and active patient. A higher level of evidence is needed to investigate the surgical management options of these injuries comparing osteosynthesis with revision arthroplasty.
Keywords: Periprosthetic fracture, hip resurfacing arthroplasty, extracapsular neck of femur fracture, fixation, implant retention.
Fractures following a resurfacing hip arthroplasty (RHA) are a well-recognized complication with an incidence between 1% and 2.5% with multifactorial etiology [1, 2, 3, 4, 5, 6]. For intracapsular neck of femur fractures, technical factors are implicated, particularly femoral neck notching and malpositioning of the prosthesis, and this post-operative complication is found to occur in a higher percentage in female patients and patient with a high BMI or osteoporosis [2, 6, 7]. The treatment options for these fractures can range from non-operative management for those patients with undisplaced or incomplete fracture [8, 9] to operative management in the form of fixation or revision arthroplasty [9, 10] .
Extracapsular femoral fractures in the presence of a RHA appear to be independent of suboptimal technique during the initial implantation of the RHA and present with a similar etiology of those of native hip fractures – that is, a fragility fracture related to pathological or age-related osteoporosis in the presence of trauma [4, 9, 11, 12] .
In the presence of a well-fixed and previously well-functioning RHA, the options for management are revision arthroplasty or open reduction and internal fixation (ORIF). In the absence of loosening through mechanisms of wear, infection, metallosis, or suboptimal prosthesis positioning, many authors have advocated ORIF with implant retention, though there is often debate between surgeons regarding the use of total hip arthroplasty in these cases [13, 14].
According to the literature, the most commonly reported technique for fixation of an extracapsular fracture in the presence of a well-fixed RHA is the use of a contoured locking compression plate (LCP) [11, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30].There have also been reported incidences of this type of periprosthetic fracture being treated non-operatively [8, 9, 31]. Other techniques are reported – particularly the use of an intramedullary nail, proximal femoral blade plate, and dynamic hip screw [16, 20, 24, 28, 30, 32, 33]. However, there are recognized downsides to these devices including concerns about the adequacy of screw purchase in the proximal femur around the RHA.
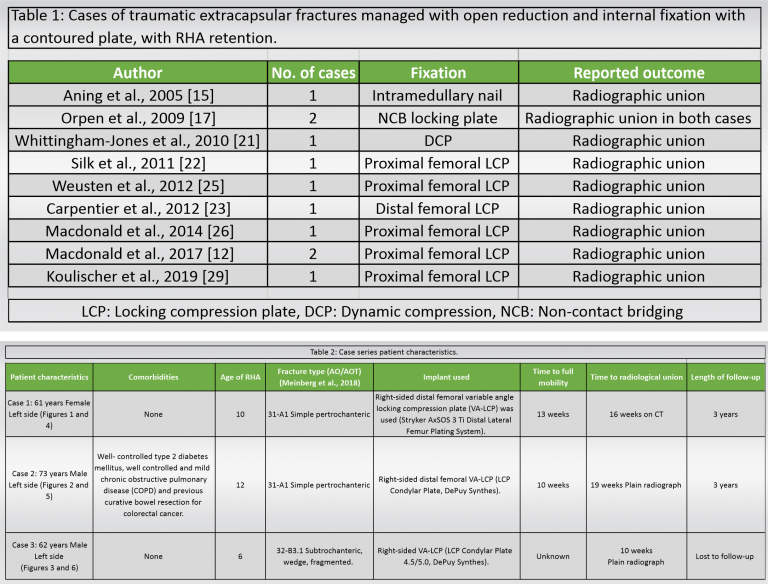
The evidence in the literature for successful treatment of this type of periprosthetic fracture with a locking plate is compelling with 100% of cases achieving union, though low in numbers and heterogeneous in technique (Table 1).
We present a case series of three patients using a standardized technique utilizing a contralateral sided distal femoral locking plate with the proximal and distal ends reversed (“upside-down”). We believe this series to be the largest series in the literature.
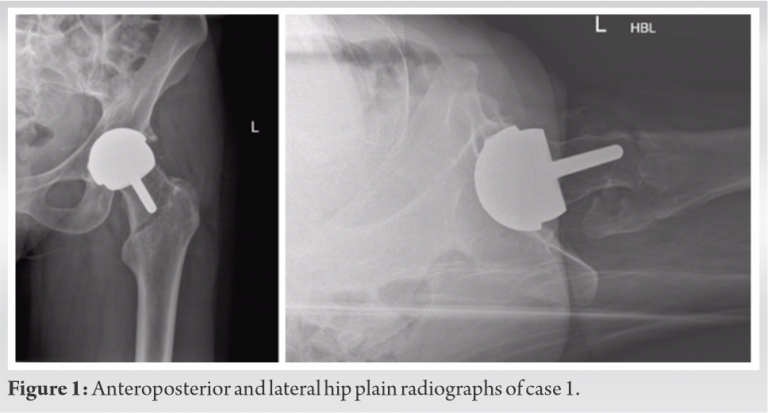
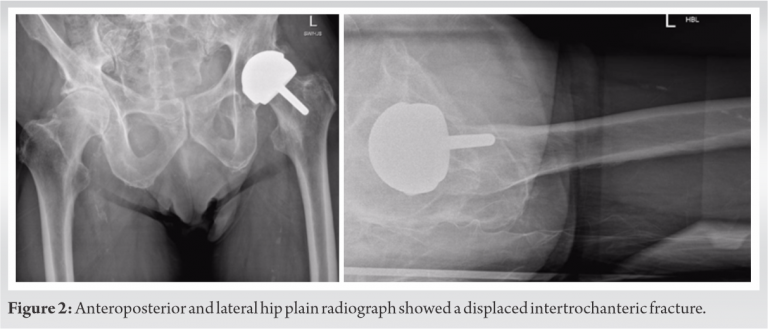
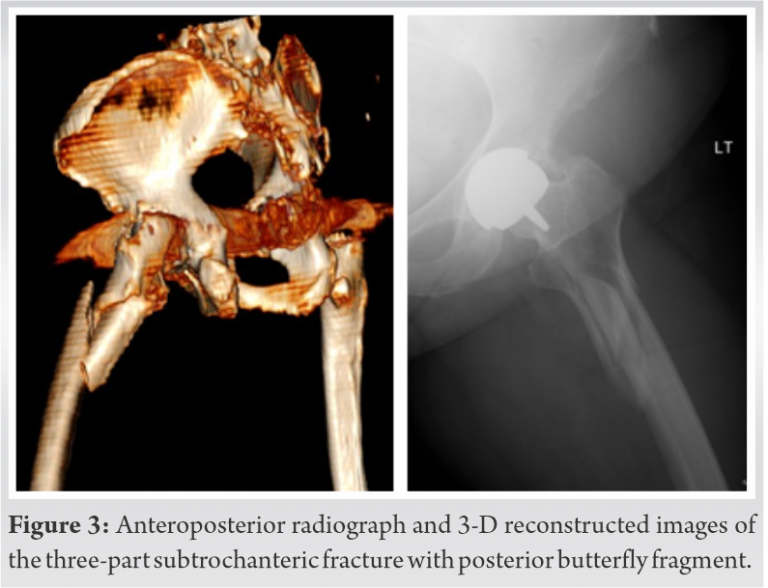
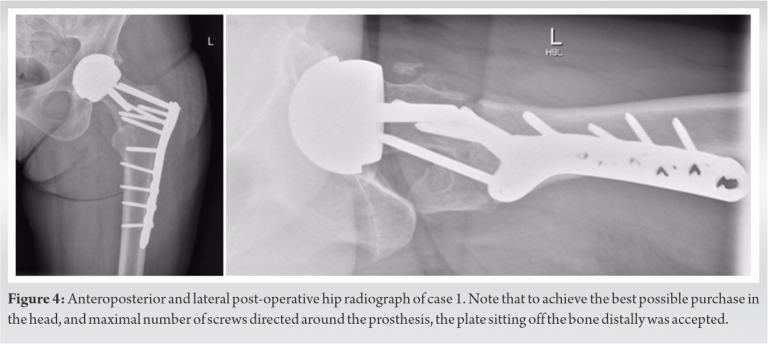
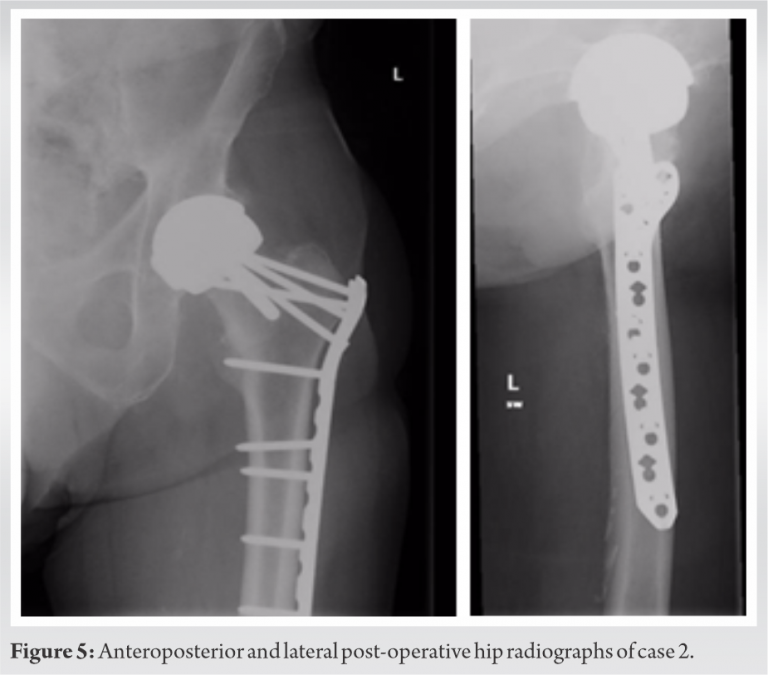
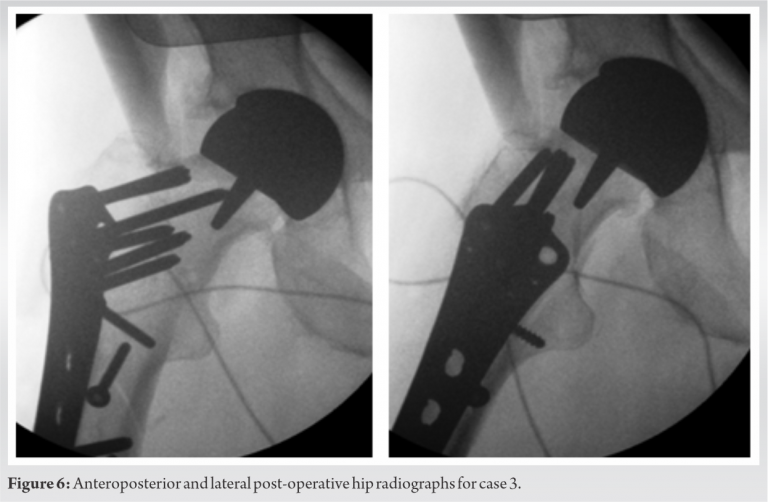
The three cases that we describe in this paper are homogenous in presentation, treatment and outcome, and therefore presented in the table below (Table 2). Pre-operative (Fig. 1-3) and post-operative (Fig. 4-6) radiographs are also included for each of the cases. 3-D reconstructed images from a computerized tomography (CT) scan for case 3 can be visualized as part of (Fig. 3).
All patients were independently mobile, active with well-fixed and well-functioning RHAs before the date of injury. All patients suffered low-energy trauma causing the fracture. All patients underwent CT scans to further delineate the fracture pattern, to assess for radiographic signs of loosening, and to assess bone stock and suitability for fixation. Intraoperatively, patients were placed on a traction table. Optimal closed reduction of the fracture was achieved using intraoperative image intensifier (II). An extended direct lateral approach to the proximal femur was used. The fascia lata was divided along its fibers and the vastus lateralis split. Fracture reduction was improved, held with 2 mm Kirschner wires placed across the fracture site, and position confirmed with II. An anatomically contoured distal femoral variable angle LCP (VA-LCP) intended for the contralateral distal femur was measured, selected, and positioned in an inverted manner (proximal and distal ends reversed). The position was checked using image intensifier. A non-locking fully threaded cortical screw was inserted distal to the fracture site to seat the plate to bone. The senior author believes that it is essential to achieve the best possible screw hold in the neck, and therefore accept to some extent that the plate distally may not sit perfectly centered over the shaft of the femur. Shaft screws can be inserted distally through a minimally invasive plate osteosynthesis technique if desired. All patients were asked to partially bear weight on the operated side for 8 weeks. The time to radiographic union and the time to discharge from physiotherapy with achievement of previous level of function were recorded for two patients. One patient, case 3 (Fig. 3, 6), was lost to follow-up as she moved out of the country.
The literature suggests two distinct fracture modalities emerging in the presence of an RHA: “Atraumatic” and “traumatic.” The predominant mode is an insidious “atraumatic” type of injury that is more often intracapsular and frequently undisplaced or minimally displaced at presentation. According to Carrothers et al., this was the most common cause of revision in a review of 5000 resurfacings [4]. Although there have been reported cases of implant retention in these types of injuries [8, 9], revision arthroplasty is the recommended definitive treatment [2]. The “traumatic” modality occurs in the setting of trauma and therefore does not have a defined timescale or incidence. This subset of fractures is predominantly extracapsular in nature [15, 20], although sub-capital fractures can occur [18]. Favorable results have been reported for extramedullary fixation of intracapsular fractures within this “traumatic” group [34], although once again the recommended course of action is revision arthroplasty. Complex arthroplasty treatment decisions are best made in conjunction with multidisciplinary team (MDT) discussions, as these cases were [35]. This paper presents 3 cases of fracture around well-fixed and well-functioning hip resurfacing arthroplasties in independent high functioning individuals. To reduce the risks associated with revision arthroplasty and following discussions with the MDT as well as the patients, fixation was the selected treatment in these cases. A distal femoral VA-LCP condylar plate was used as it has more screw options compared to most proximal femoral locking plates. The reversed distal femur plate of the contralateral limb has an anatomic profile that sits well in the proximal femur and allows for increased screw purchase and screw density in the proximal femur around a RHA. It was also decided to avoid using plates with greater trochanteric extensions to reduce the risk of lateral hip pain, iliotibial band irritation, and need for future removal of metalwork. Patients are suitable for this treatment if they have a well-function and well-fixed prosthesis, if they have good bone stock and are able to fully or partially bear weight without discomfort (in the opinion of the operating surgeon and MDT). An inability to bear weight, in these cases, could be viewed as a surrogate marker of fitness and further guide the decision to fix or revise. Revision to a total hip replacement remains the treatment of choice for a failed resurfacing, where the mode of failure is loosening, osteonecrosis of the head and collapse, or early fracture due to poor positioning or patient factors. Several studies have shown that the outcome from revision does significantly reduce patient-reported outcome measures (PROMS), when compared to pre-revision or even pre-primary surgery level [29, 36]. Whilst it is recognized that conservative management is an option, particularly in the undisplaced and potentially incomplete fracture, the risks associated with non-operative management of patients with neck of femur fractures are not acceptable to the active and high functioning patient. These risks include fracture displacement, non- and mal-union, and reduced mobility [8, 9, 31]. Complications of fixation around the femoral prosthesis of a hip resurfacing arthroplasty include increased risk of deep vein thrombus or pulmonary embolus due to non-weight-bearing status and increased immobility in the rehabilitation period. In addition, trochanteric bursitis and plate irritation may necessitate the removal of the plate. Other complications include periprosthetic fracture distal to the plate fixation, non- and mal-union, and a potentially more complex revision surgery to THA in the future (if required). Avascular necrosis and subsequent collapse if blood supply to the femoral neck is disrupted are a possibility, but this is more likely in the case of an intracapsular fracture, as reported in one case study [18]. The current literature regarding the treatment of pertrochanteric fractures around a well-fixed and well-functioning hip resurfacing almost universally reports favorable outcomes following fixation with both proximal and distal locking compression plating or intramedullary nailing and there is a substantial body of evidence built up over several years that include 11 cases so far with an outcome of radiological union [12, 15, 17, 21, 22, 23, 25, 26, 29]. In summary, we present our technique that is reproducible and achieves good fixation into the femoral neck. This is yet another tool in the surgeons’ armamentarium of techniques to treat these difficult fractures.
We believe that fixation of extracapsular femoral neck fractures in the presence of a well-fixed, well-functioning resurfacing arthroplasty is a reasonable option in an independent and active patient. A higher level of evidence is needed to investigate the surgical management options of these injuries comparing osteosynthesis with revision arthroplasty.
Extracapsular femoral neck fractures in the presence of a RHA can be challenging to treat. Fixation with implant retention in the presence of a well-fixed and well-functioning RHA is a suitable alternative management option for independent and active patients.
References
- 1.Amstutz HC, Campbell PA, Le Duff MJ. Fracture of the neck of the femur after surface arthroplasty of the hip. JBJS 2004;86:1874-77. [Google Scholar]
- 2.Shimmin AJ, Back D. Femoral neck fractures following Birmingham hip resurfacing. J Bone Joint Surg Series B 2005;87:463-4. [Google Scholar]
- 3.Steffen RT, Foguet PR, Krikler SJ, Gundle R, Beard DJ, Murray DW. Femoral neck fractures after hip resurfacing. J Arthroplasty 2009;24:614-9. [Google Scholar]
- 4.Carrothers AD, Gilbert RE, Jaiswal A, Richardson JB. Birmingham hip resurfacing: The prevalence of failure. J Bone Joint Surg 2010;92:1344-50. [Google Scholar]
- 5.Kohan L, Field CJ, Kerr DR. Early complications of hip resurfacing. J Arthroplasty 2012;27:997-1002. [Google Scholar]
- 6.Marker DR, Seyler TM, Jinnah RH, Delanois RE, Ulrich SD, Mont MA. Femoral neck fractures after metal-on-metal total hip resurfacing: A prospective cohort study. J Arthroplasty 2007;22:66-71. [Google Scholar]
- 7.Anglin C, et al. Hip resurfacing femoral neck fracture influenced by valgus placement and bone mineral density. In: Orthopaedic Proceedings. England: The British Editorial Society of Bone & Joint Surgery; 2008. p. 133. [Google Scholar]
- 8.Cumming D, Fordyce MJ. Non-operative management of a peri-prosthetic sub capital fracture after metal-on-metal Birmingham hip resurfacing. J Bone Joint Surg 2003;85:1055-6. [Google Scholar]
- 9.Cossey AJ, Back DL, Shimmin A, Young D, Spriggins AJ. The nonoperative management of periprosthetic fractures associated with the Birmingham hip resurfacing procedure. J Arthroplasty 2005;20:358-61. [Google Scholar]
- 10.Ball ST, Le Duff MJ, Amstutz HC. Early results of conversion of a failed femoral component in hip resurfacing arthroplasty. JBJS 2007;89:735-41. [Google Scholar]
- 11.Brennan SA, Devitt BM, O’Neill CJ, Nicholson P. Periprosthetic fractures in the resurfaced hip-a case report and review of the literature. Injury 2013;44:263-5. [Google Scholar]
- 12.Macdonald J, Pagoti R, Cusick L. Bilateral fixation of a periprosthetic intertrochanteric hip fracture below Birmingham hip resurfacing. BMJ Case Rep 2017. 2017:bcr2016218840. [Google Scholar]
- 13.Nie B, Wu D, Yang Z, Liu Q. Comparison of intramedullary fixation and arthroplasty for the treatment of intertrochanteric hip fractures in the elderly: A meta-analysis. Medicine 2017;96:e7446. [Google Scholar]
- 14.Morsi EM, Drwish AE, Saber AM, Nassar IM, Zaki AE. The use of standard cemented femoral stems in total hip replacement after failed internal fixation of intertrochanteric femoral fractures. J Arthroplasty 2020;35:2525-8. [Google Scholar]
- 15.Aning J, Aung H, Mackinnon J. Fixation of a complex comminuted proximal femoral fracture in the presence of a Birmingham hip resurfacing prosthesis. Injury 2005;36:1127-9. [Google Scholar]
- 16.Weinrauch P, Krikler S. Proximal femoral fracture after hip resurfacing managed with blade-plate fixation: A case report. J Bone Joint Surg Series A 2008;90:1345-7. [Google Scholar]
- 17.Orpen NM, Pearce O, Deakin M, Keys RI. Internal fixation of trochanteric fractures of the hip after surface replacement. Injury Extra 2009;40:32-5. [Google Scholar]
- 18.Zustin J, Winter E. Failed internal fixation due to osteonecrosis following traumatic periprosthetic fracture after hip resurfacing arthroplasty: A case report and review of the literature. Acta Orthop 2009;80:666-9. [Google Scholar]
- 19.Baxter JA, Krkovic M, Prakash U. Intertrochanteric femoral fracture after hip resurfacing managed with a reverse distal femoral locking plate: A case report. Hip Int 2010;20:562-4. [Google Scholar]
- 20.Lein T, Schlee J, Kothe M, Moritz F, Wubtaye DT. Periprosthetic intertrochanteric fracture of the femur following articular resurfacing of the hip joint: treatment with lag screw osteosynthesis. Der Unfallchirurg 2010;113:944-50. [Google Scholar]
- 21.Whittingham-Jones P, Charnley G, Francis J, Annapureddy S. Internal fixation after subtrochanteric femoral fracture after hip resurfacing arthroplasty. J Arthroplasty 2010;25:334.e1-4. [Google Scholar]
- 22.Silk G, Sangster M, Sandhu H. Internal fixation of trochanteric fracture following hip resurfacing. Injury Extra 2011;42:183-5. [Google Scholar]
- 23.Carpentier K, Govaers K. Internal fixation of an intertrochanteric femoral Fracture after Birmingham hip resurfacing arthroplasty. Acta Orthop Belg 2012;78:275-8. [Google Scholar]
- 24.Peskun CJ, Townley JB, Schemitsch EH, Waddell JP, Whelan DB. Treatment of periprosthetic fractures around hip resurfacings with cephalomedullary nails. J Arthroplasty 2012;27:494.e1-3. [Google Scholar]
- 25.Weusten AJ, Khan SK, Bonczek SJ, Elsharief D, Wallace IW. Internal fixation of a traumatic fracture around a hip resurfacing arthroplasty using the proximal femoral locking compression plate. Acta Orthop Belg 2012;78:688-93. [Google Scholar]
- 26.Macdonald J, Robinson A, Brown I. Fixation of a periprosthetic intertrochanteric hip fracture below a Birmingham hip resurfacing. Case Rep Orthop 2014;2014:393984. [Google Scholar]
- 27.Banerjee S, Little T, Little N. Intramedullary fixation of pertrochanteric fractures after hip resurfacing arthroplasty-do we have the answer? Case report and literature review. J Orthop 2015;12:66-9. [Google Scholar]
- 28.Chou DT, Davis B. Trochanteric femoral fracture around a Birmingham hip resurfacing prosthesis: A case report and review of the literature. JBJS Case Connector 2017;7:e7. [Google Scholar]
- 29.Koulischer S, Devos S, Verstraeten PB, Delahaut O, Muhadri A. Internal fixation of an intertrochanteric fracture after resurfacing arthroplasty: A case report. J Orthop Case Rep 2020;9:65. [Google Scholar]
- 30.van Rijn J, Koper MC, Bos PK. Routine fracture fixation for a periprosthetic hip fracture below Birmingham hip resurfacing: A case report. JBJS Case Connector 2020;10:e19. [Google Scholar]
- 31.Morgan D, Myers G, O’Dwyer K, Thomas AM. Intertrochanteric fracture below Birmingham hip resurfacing: Successful non-operative management in two cases. Injury Extra 2008;39:313-5. [Google Scholar]
- 32.Setia P, Gaitonde A. Proximal femoral nailing for intertrochanteric fracture in birmingham hip resurfacing arthroplasty. Int J Orthop 2020;7:1407-9. [Google Scholar]
- 33.Vajapey SP, Li M. Intramedullary nailing of a periprosthetic intertrochanteric fracture in the setting of prior hip resurfacing: A new technique for fracture fixation. Tech Orthop 2021; 36(2), 151-156. [Google Scholar]
- 34.Kutty S, Pettit P, Powell JN. Intracapsular fracture of the proximal femur after hip resurfacing treated by cannulated screws. J Bone Joint Surg 2009;91:1100-2. [Google Scholar]
- 35.Ibrahim MS, Raja S, Khan MA, Haddad FS. A multidisciplinary team approach to two stage revision for the infected hip replacement: A minimum five-year follow-up study. Bone Joint J 2014;96:1312-8. [Google Scholar]
- 36.Gilbert RE, Cheung G, Carrothers AD, Meyer C, Richardson JB. Functional results of isolated femoral revision of hip resurfacing arthroplasty. JBJS 2010;92:1600-4. [Google Scholar]