Distraction osteotomy of the contralateral superior pubic ramus can help in managing irreducible OPSD cases 2. Anterior plate fixation can be safely done with SPC insitu.
Dr. Ajay Kumar Goel,
Department of Orthopaedics,
The Calcutta Medical Research Institute (CMRI), Kolkata, West Bengal, India.
E-mail: ajaygoelortho@gmail.com
Introduction: Overlapping pubic symphysis dislocation (OPSD) or a locked pubic symphysis is a compression of the pelvic ring with the intact pubis trapped into the contralateral obturator foramen. Reduction can be difficult and contralateral suprapubic osteotomy is a good way to address the irreducible OPSD. The technique has only been discussed thrice in the available literature.
Case Report: We report the case of a 26-year-old man who had his right pubic ramus entrapped within the contralateral obturator foramen, having an overlap of >4 cm with associated ipsilateral sacroiliac joint (SI joint) disruption and urethral injury. When all the maneuvers of closed and instrumented open reduction failed, we performed a superior pubic ramus osteotomy on the left side and unlocked the incarcerated right pubic ramus. The osteotomy site was stabilized with a 6-hole recon plate and SI joint was stabilized with a 6.5mm percutaneous sacroiliac screw. The patient underwent delayed urethral repair at 10 weeks after the index surgery. At 3-year follow-up, the patient did not report any pubic discomfort, urinary and sexual problems.
Conclusion: Locked OPSD is a rare injury and is frequently associated with sacroiliac and urethral injuries. Distraction osteotomy of the contralateral superior pubic ramus is a viable option for irreducible cases.
Keywords: Lateral compression injury, locked symphysis pubis, superior pubic ramus osteotomy, overlapping pubic symphysis dislocation.
Pelvic ring disruptions resulting in a locked symphysis pubis are an uncommon pattern of injury. By definition, an overlapping pubic symphysis dislocation (OPSD) or a locked pubic symphysis is a lateral compression of the pelvic ring, with the intact pubis trapped into the contralateral obturator foramen [1]. Although this type of injury was originally described by Eggers [2] in 1952, only thrice before a similar technique of reduction has been reported [1, 3, 4]. Urethral injury is the most commonly associated non-orthopedic injury(7–55%)[3, 5, 6, 7, 8, 9, 10]. It occurs mainly because of the shearing forces formed due to the overlapping and vertical displacement of the pubic bone. We report the case of a patient with a locked OPSD that was not amenable to the typical closed or open reduction techniques, and required an osteotomy of the contralateral superior pubic ramus to unlock and reduce the pubic bone which was incarcerated into the contralateral obturator foramen.
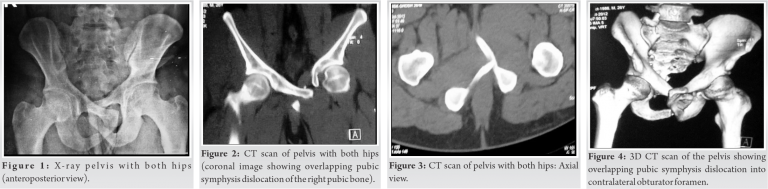
A 26-year-oldman presented to us following a high-velocity road traffic accident. He was unable to walk or pass urine after the injury. Following initial treatment elsewhere, he was referred to our hospital 2 days later for the treatment of the pelvic injury. There was a history of acute urinary retention, blood at the urethral meatus, and failed Foley’s catheterization. On arrival in the ER, the patient was hemodynamically stable with a Glasgow Coma Score of 12/15 and a suprapubic catheter (SPC)insitu. There was extensive ecchymoses over the suprapubic area and Morel-Lavallée lesion over the right proximal thigh and greater trochanteric region. The patient had tenderness on palpation of the right sacroiliac joint and symphysis pubis. His right anterior superior iliac spine was elevated anteriorly and displaced medially, but no apparent limb length discrepancy was noted. He was unable to perform an active straight leg raise on the right side. Both hip joints were non-tender with good rotatory movement. His right hip was observed to be in an attitude of hyperextension, adduction, and internal rotation. Digital rectal examination and focused assessment with sonography in trauma scans were normal. Pelvic compression and distraction tests were not performed because of the pain. Anteroposterior radiograph (Fig. 1) and computed tomography (CT) scan with 3D reconstruction of the pelvis (Fig. 2, 3, 4) showed disruption of the symphysis pubis with herniation of the right pubis into the left obturator foramen. This was associated with the right sacroiliac disruption.
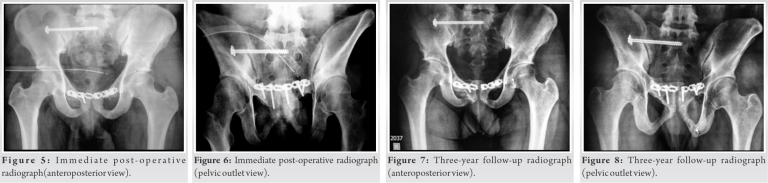
After proper evaluation by the urology, gastric surgery, and anesthesia team, the patient was planned for surgery. After failed initial attempts at closed reduction, the decision to proceed with open reduction was taken. A modified Pfannenstiel incision was made. The insertion of the rectus abdominis muscle was observed to be disrupted along nearly two-thirds of its bony insertion on the right side. The remaining part of the rectus was carefully divided a few millimeters above its insertion on the bone. Then, the cut edges of rectus abdominal muscles were retracted superiorly and the symphysis pubis was exposed subperiosteally. During the procedure, Gamjee pad was inserted posteriorly to protect the bladder and other visceral structures. The right pubis was observed to be incarcerated about 4 cm into the left obturator foramen after having been forced medially and posteriorly. Initial attempts to reduce the pubic symphysis by levering the locked right pubic body out from the left obturator foramen met with failure. Next, external fixator was applied with supra-acetabular Schanz pin placements and the pelvis was gradually distracted to achieve reduction; however, this maneuver also failed. Finally, we opted for a vertical osteotomy of the left superior pubic ramus approximately 2.5 cm from the midline. Lamina spreader was applied into the osteotomy site and it was gradually distracted. Progressively increasing the distraction at the osteotomy site freed the incarcerated right pubic ramus body and it gradually returned back to its normal anatomical position. Post-reduction, the symphysis pubis remained unstable and a 6-hole transpubic recon plate was applied, incorporating the osteotomy site, to achieve stability. The right sacroiliac joint was then stabilized with one 6.5mm × 70mm cannulated partially threaded cancellous screw percutaneously under image intensifier guidance (Fig. 5, 6). The wounds were closed in layers. Care was taken to repair the rectus abdominis insertion, augmented with non-absorbable sutures anchored to the periosteum.
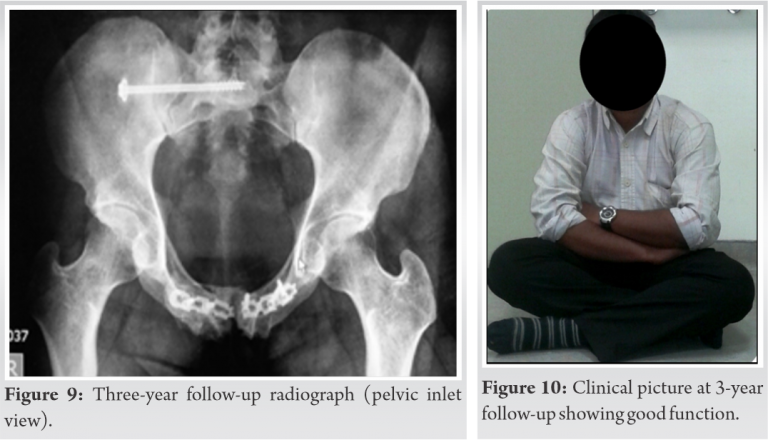
The post-operative period was uneventful. Gluteal sets, TFL stretching, and isometric quadriceps exercises were started from the 2nd post-operative day. Mobilization with partial weight-bearing and strengthening of the rectus was initiated at 8 weeks with progression to full weight-bearing at 3 months. The patient underwent micturating cystourethrogram at 10 weeks followed by penile urethral repair. The fracture healed with no secondary displacement in 3–4 months’ time. He resumed routine activities of daily living at 4 months and sports activities after 6 months. There was breakage of implant and heterotopic ossification in subsequent follow-up; however, the patient did well without any symptoms of hardware breakage and the implant was not removed. At 3-year follow-up (Fig. 7, 8, 9, 10), the patient has not reported any pubic discomfort (osteomyelitis and non-infective osteitis pubis), urinary problems, and/or sexual problems.
Egger [2] in 1952 was the first to describe locking of the symphysis pubis without injury to the other parts of the pelvic ring. A proposed mechanism of injury for this involves forced hyperextension, hyperadduction, and internal rotation of the hip due to lateral compression of the pelvis [3, 5]. OPSD occurs more commonly in men than women [1]. The reasons postulated are that the female pubic symphysis has a thicker cartilaginous disc, also female pelvis has greater mobility and larger inner diameter than male pelvis [5]. OPSD can be associated with posterior pelvic ring injury ranging from buckle fracture of sacrum to complete sacroiliac disruption [11]. Shanmugasundaram [6] in 1970 reported a case of symphysis pubis dislocation without locking into the obturator foramen. It was associated with urethral injury which was repaired later. Closed reduction failed, hence open reduction was undertaken. The author maintained the reduction with hip spica for 4 weeks. Webb [9] also described a similar case of OPSD along with the urethral injury. Closed reduction achieved a stable symphysis pubis in this case and urethral injury required delayed repair. Robinson et al. [5] described a method of closed reduction of a similar symphysis pubis dislocation without urethral injury following a parachuting related trauma. The injury was hypothesized to have been caused by either side-to-side compression or hyperextension. Cannada and Reinert [11] reported the use of external fixators for maintenance of reduction in their series, as the patients had undergone previous suprapubic catheterization. However, in our case, no infection was observed with anterior plate fixation even when the patient had SPC insitu. In addition, they hypothesized that there may be a rotational component along with the lateral compression forces to produce an OPSD. Thulasiraman et al. [7] proposed a radiological classification system for locked pubic symphysis. The first type describes a locked pubis just posterior to the opposite side pubis, within 2.5 cm from the midline. The second type shows displacement of the pubis to the opposite side of more than 2.5 cm, but yet to engage into the obturator foramen. In the third type, the pubis is herniated into the contralateral obturator foramen. Maqungo et al. [12] also graded OPSD on the basis of severity and instability of the pelvic ring. In Grade 1, closed reduction can be achieved and maintained, whereas in Grade 2, OPSD open reduction is required. Grade 3 describes locked symphysis pubis where pubis is incarcerated into the opposite obturator foramen. Each grade has been further subclassified into two types: Type A is without a significant posterior ring injury, whereas type B involves a significant posterior ring injury. Achieving reduction is always difficult in locked pubic symphysis and most of these cases require open reduction. O’Toole et al. [3] first described acontralateral suprapubic osteotomy for reduction of locked pubic symphysis as all the closed and open reduction methods were unsuccessful. However, they used external fixator as fixation modality. There was associated sacral ala fracture which was treated conservatively. Li et al. [1] in 2013 reported a case of a 42-year-old female, managed by vertical osteotomy of the contralateral superior pubic ramus and plate fixation. Associated sacral fracture was also fixed with transiliac plate. Both the authors report acute urethral injury in their cases; however, patients did well at the final follow-up. Pushpasekaran et al.[4] also used similar technique of reduction as used by us and other two authors but they fixed the osteotomy site in buttress mode instead of neutral mode; their reason behind this mode of fixation being the prevention of implant failure by decreasing the stresses in the pelvis caused by plastic deformation. Posterior ring injury involving plastic deformation of sacrum and minimal sacroiliac joint injury was treated conservatively and there was no urinary injury at presentation in their case, but the patient developed secondary urethral stricture which required urethroplasty.
Locked OPSD is a rare injury and is usually associated with urethral and posterior pelvic ring injuries. Reduction can be challenging and distraction osteotomy of the contralateral superior pubic ramus helps by reducing the stiffness of the closed pelvis and thereby helping it mobilize.
Distraction osteotomy of the contralateral superior pubic ramus can be a savior in irreducible OPSD cases and minimizes further soft-tissue injury. Furthermore, anterior plate fixation can be safely done with SPC insitu.
References
- 1.Li KH, Sun BH, Zhu Y, Long HT. Locked pubic symphysis into the obturator foramen: A rare case presentation and literature review. Orthop Traumatol Surg Res 2013;99:106-10. [Google Scholar]
- 2.Eggers GW. Dislocations of the os coxae. Am J Surg 1952;83:300-7. [Google Scholar]
- 3.O’Toole RV, Sagebien C, Andersen RC, Nascone JW. Superior pubic ramus osteotomy to treat locked pubic symphysis: A case report. J Bone Jt Surg Ser A 2006;88:1609-14. [Google Scholar]
- 4.Pushpasekaran N, Thampy S, Khaleel VM, Joseph S. Treatment of locked pubic symphysis by distraction osteotomy of the superior pubic ramus: A case report. J Coll Physicians Surg Pak 2020;10:e0196. [Google Scholar]
- 5.Robinson D, Hendel D, Halperin N. An overlapping pubic dislocation treated by closed reduction: Case report and review of the literature. J Trauma 1989;29:883-5. [Google Scholar]
- 6.Shanmugasundaram TK. Unusual dislocation of symphysis pubis with locking. A case report. J Bone Joint Surg Am 1970;52:1669-71. [Google Scholar]
- 7.Thulasiraman V, Pandian TR, Ashok S. Locked pubic symphysis a case series. Injury Extra 2010;41:20-4. [Google Scholar]
- 8.Sreesobh KV, Sageer AM, Raffic M. Locked overlapping dislocation of the pubic symphysis into the obturator foramen: A case report. J Orthop Surg (Hong Kong) 2006;14:200-3. [Google Scholar]
- 9.Webb P. Overlapping dislocation of the symphysis pubis: A case report. J Bone Joint Surg Ser A 1977;59:839. [Google Scholar]
- 10.Tadros AM, Lunsjo K, O’Brien P. Overlapping dislocation of the pubic symphysis: Report of three cases and review of the literature. Arch Orthop Trauma Surg 2009;129:679-83. [Google Scholar]
- 11.Cannada LK, Reinert CM. Case report: Locked pubic symphysis: An open reduction technique. Clin Orthop Relat Res 2009;467:2192-5. [Google Scholar]
- 12.Maqungo S, Koller IR. Overlapping pubic symphysis dislocation: A case report and proposal of a classification system. SA Orthop J 2010;9:74-7. [Google Scholar]