Surgical management in the form of osteotomy is an acceptable management for patients with ichthyosis and severe bony deformities, it has the potential to drastically improve the quality of life of the patient.
Dr. Siddhartha Sinha,
Department of Orthopaedics, Hamdard Institute of Medical Sciences and Research,
New Delhi, India.
E-mail: siddharthasinha87@gmail.com
Introduction: Ichthyosis is a group of disorders typically characterized by the accumulation of large scales over the skin. Mild bony deformities due to Vitamin D deficiency are commonly associated with this group of disorders which can be successfully treated with conventional Vitamin D supplementation. Severe multiple bony deformities requiring surgical correction are rarely reported and may be associated with various other disorders.
Case Report: We report a case of a 15-year-old male with ichthyosis, short stature, and progressive multiple bony deformities since birth. The child was started on Vitamin D3 supplementation. Once biochemical parameters improved he underwent multiple corrective osteotomies in the bilateral tibia and right femur to improve gait mechanics. Our main concerns while managing the patient were regarding wound healing, secondary infection due to extensive scaling and healing at the osteotomy site. On follow-up we noted good healing at the osteotomy site without any surgical site infection or skin complications as well as improvement in gait mechanics and cosmesis.
Conclusion: Severe bony deformities due to Vitamin D deficient are rare in ichthyosis and other syndromic causes should be ruled out. Surgical management can be beneficial in improving quality of life and gait biomechanics.
Keywords: Lamellar ichthyosis, osteotomy, genetic testing, Vitamin D deficiency.
The association of ichthyosis with Vitamin D deficiency is now well documented and most authors have reported only mild deformities, which resolve with Vitamin D supplementation [1, 2, 3]. Association of ichthyosis with short stature and severe bony deformities is relatively rare and may indicate syndromic association, prolonged untreated Vitamin D dependent rickets, or possible presence of Vitamin D resistant rickets [4, 5]. We report a case of congenital ichthyosis with severe bony deformities who presented to our orthopedic outpatient.
A 15-year-old male presented to our outpatient department with complaints of multiple bony deformities, short stature, and difficulty in walking since childhood. His parents told that at the time of birth, there was a shiny adherent membrane all around his body which shed off over 2 weeks revealing reddish pink skin following which a frequent cycle of scaling and shedding of the skin occurred. Parents also noticed the development of multiple deformities involving all extremities and spine as he began to walk which worsened as the child grew. He was unable to walk long distances, play with friends and had to drop out of school due to the nature of deformities and poor cosmesis. The child was using skin creams and medications intermittently for skin condition. He has one sibling who does not have such complaints. He had not received any orthopedic management for correction of his skeletal deformities.
On physical examination, the child had a height of hundred and 22 cm and weight of 24 kg, both these parameters were below the third percentile of the Indian Academy of Pediatrics chart for height and weight for boys. Cognitive and speech functions were intact.
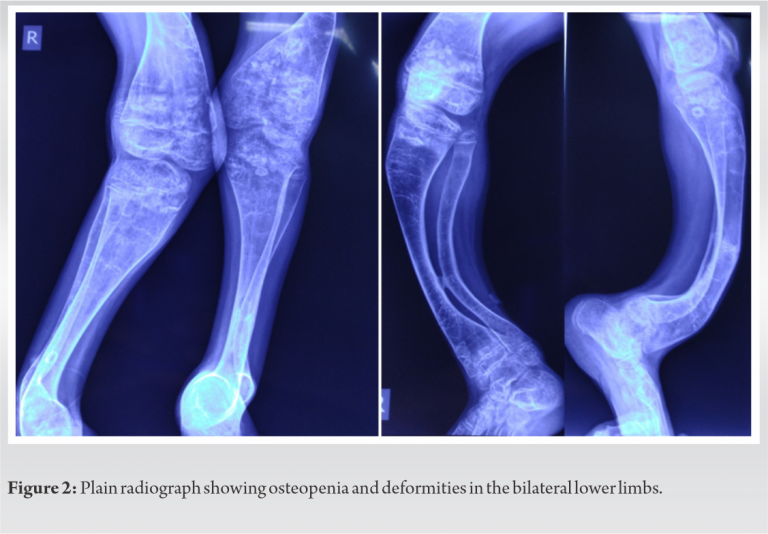
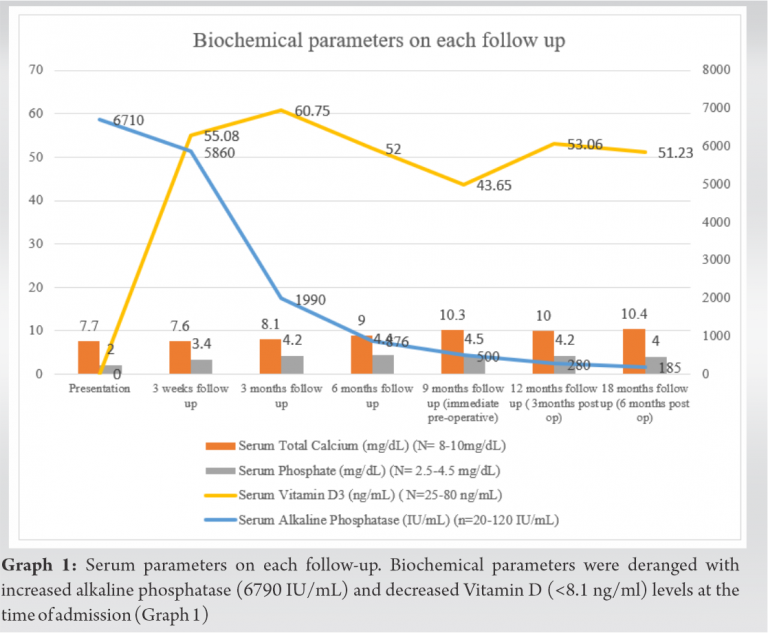
Examination revealed brown scales all over the body, including the scalp, flexural surfaces, and external auditory meatus. The scales were large in size and odorless, adherent to the skin. Thin hair was noted on the scalp with entangled fine scales. Abnormal dentition and missing teeth were also noted. There was fixed kyphoscoliosis with convexity to the right side. The right forearm showed bowing and the right upper limb appeared “S” shaped. Pronation and supination were severely restricted on the right side due to old malunited fracture in the forearm. There was anterior bowing of the right femur and lateral bowing of the left femur as well as anterolateral bowing of bilateral tibia and lateral dislocation of the right patella (Fig. 1). Plain radiographs showed multiple bony deformities in the lower limbs (Fig. 2). Skin biopsy confirmed the diagnosis of lamellar ichthyosis. Oral Vitamin D supplementation was started at 5000IU daily dose along with oral calcium supplementation [6], oral tretinoin and topical emollients were given for skin disease. Once biochemical parameters were normalized, he was planned for a staged correction of all lower limb deformities to prevent postoperative infection due to poor skin condition. We first performed a right-sided distal tibia corrective osteotomy. As there were no immediate signs of surgical site infection with good healing of surgical wound, after 1 week a right-sided supracondylar femoral osteotomy was done. Following this procedure, the patella spontaneously relocated. A third osteotomy procedure was performed after 3 weeks for correction of the left distal tibia. We followed standard pre and post-operative protocol for all procedures. All surgical sites healed without any complications and at 6 weeks follow-up assisted walking was started as the osteotomy sites were uniting on radiograph (Fig. 3).
We continued Vitamin D supplementation on a monthly basis. At 18 months follow-up, we observed improved gait mechanics, decreased pain and fatigue while mobilizing. His scaling and cosmetic appearance also improved and biochemical parameters were within normal limits (Fig. 4).
Vitamin D deficiency is common in ichthyosis and presents with mild or no deformities. Various mechanisms have been proposed for Vitamin deficiency in these patients (Table 1) [1, 7]. A small percentage of ichthyosis children manifest with severe deformities and short stature. These severe deformities can be either due to prolonged untreated nutritional rickets or due to associated syndromes (Table 2). Some authors have proposed association of some forms of ichthyosis and Vitamin D resistant rickets following large contiguous deletions of genes on the same chromosome. Deletions of 12q13 coding for keratin 1 can involve12q13-14 coding for Vitamin D receptor causing a cellular Vitamin D resistance [8]. Similarly, deletion around Xp22.31 coding for steroid sulfatase can involve Xp22.1 coding for Phosphate Endopeptidase Homolog X- linked leading to hypophosphatemic rickets which is also Vitamin D resistant [9].
Based on this hypothesis we should explore the use of genetic testing in such patients, wherever possible. Testing if done before the growth spurt may enable us to determine the sensitivity of rickets to conventional Vitamin D supplementation and may prevent the development of short stature and disabling deformities by the initiation of appropriate treatment. In cases where resources are sparse a close monitoring of biochemical parameters to Vitamin D therapy and timely referral should be considered. In our patient, the deformities were due to prolonged vitamin D deficiency as the biochemical parameters normalized with Vitamin D and calcium supplementation. Although there is no reported literature showing results of corrective osteotomy in children with ichthyosis, we faced no complication related to surgical wound infection and osteotomy site union in our patient.
Vitamin D deficiency in ichthyosis is a common phenomenon but rarely presents with severe deformities. In cases of severe deformities with ichthyosis, one should initiate appropriate treatment and attempt to rule out syndromic causes. Surgical therapy including osteotomy can be considered and has yielded good results for this child leading to an improvement in quality of life.
Vitamin D deficiency in ichthyosis rarely causes severe bony deformities. In patients presenting with severe bony deformities, syndromic involvement should be ruled out. Surgical management in the form of osteotomy is an acceptable management and improves the quality of life.
References
- 1.Deka N, Sarma D, Saikia UK. Lamellar ichthyosis with genu valgum: unfolding the link. BMJ Case Rep 2012;2012:bcr1120115136. [Google Scholar]
- 2.Ingen‐Housz‐Oro S, Boudou P, Bergot C, Ibrahim F, Souberbielle J, Dubertret L, et al. Evidence of a marked 25‐hydroxyvitamin D deficiency in patients with congenital ichthyosis. J Eur Acad Dermatol Venereol 2006;20:947-52. [Google Scholar]
- 3.Sethuraman G, Khaitan B, Dash S, Chandramohan K, Sharma V, Kabra M, et al. Ichthyosiform erythroderma with rickets: Report of five cases. Br J Dermatol 2008;158:603-6. [Google Scholar]
- 4.Barraud C, Cano A, Boulay C, Milh M, Bollini G, Chabrol B. Vitamin D deficiency rickets complicating Dorfman-Chanarin syndrome. Arch Pediatr 2015;22:414-7. [Google Scholar]
- 5.Lakhani SJ, Lakhani OJ. Short stature with congenital ichthyosis. BMJ Case Rep 2015;2015:bcr2015212610. [Google Scholar]
- 6.Balasubramanian S, Dhanalakshmi K, Amperayani S. Vitamin D deficiency in childhood a review of current guidelines on diagnosis and management. Indian Pediatr 2013;50:669-75. [Google Scholar]
- 7.Kumar V, Kalra S, Mutreja D, Arya A. Rickets associated with ichthyosis. Paediatr Int Child Health 2012;32:119-20. [Google Scholar]
- 8.El‐Khateeb EA. Bullous congenital ichthyosiform erythroderma associated with hypocalcemic Vitamin D‐resistant rickets. Pediatr Dermatol 2008;25:279-82. [Google Scholar]
- 9.Song Y, Chen J, Yi Z, Dang X, Cheng D, Wu X, et al. Genetic analysis of a 12-year-old boy with X-linked ichthyosis in association with sclerosing glomerulonephritis. Mol Med Report 2013;8:1183-7. [Google Scholar]