Osteochondrosis of humeral capitellum though rare is a known condition in young children. High level of awareness is required to adequately diagnose and treat appropriately.
Dr. Sumant Chavda,
Department of Orthopaedics,
RAK Medical and Health Sciences University,
Ras al Khaimah, United Arab Emirates.
E-mail: sumant@rakmhsu.ac.ae
Introduction: Osteochondrosis of humeral capitellum (Panner’s disease) is a rare condition. Very few cases are reported in the literature and may be overlooked or misdiagnosed. Most cases are unilateral in distribution and occur in young boys during the first decade of life. It is often difficult to distinguish osteochondrosis from osteochondritis dissecans of the humeral capitellum that occurs in older children and adolescents in the second decade of life.
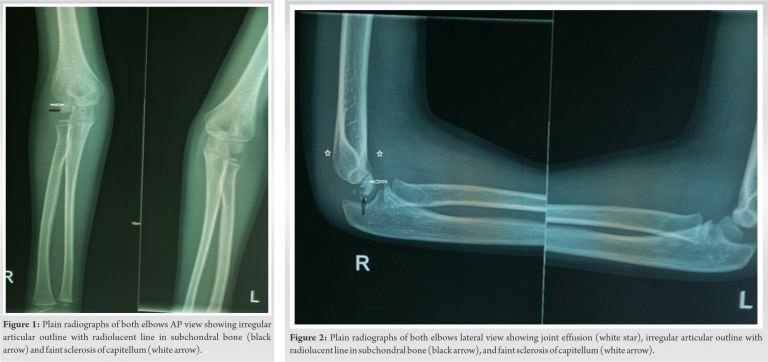
Case Report: We describe a case of a 6-year-old boy who presented with pain, subtle swelling and limited extension in his right elbow following a fall. Diagnosis of Panner’s disease was made 2 weeks later on follow-up based on classical features on plain radiograph of joint effusion, irregular delineation of the articular contour, and faint sclerosis of the capitellum with a radiolucent line in the subchondral bone. The patient had uneventful full functional recovery with conservative treatment: Rest, temporary immobilization, and subsequent remobilization.
Conclusion: Osteochondrosis of humeral capitellum though rare is a known condition. It may be overlooked or misdiagnosed. High degree of awareness is required and diagnosis can be made with utmost care based on the age of presentation, clinical signs and clearly recognizable plain radiographic features of joint effusion, irregular articular outline with radiolucent line in subchondral bone and faint sclerosis of capitellum.
Keywords: Osteochondrosis, humerus capitellum, Panner’s disease.
Osteochondrosis of humeral capitellum (Panner’s disease) is not a common condition seen in orthopedic clinic [1]. Very few cases are reported in the literature and may often be overlooked or misdiagnosed. Most cases are unilateral in distribution and occur in young boys during the first decade of life [1]. It is often difficult to distinguish osteochondrosis from osteochondritis dissecans (OCD) of the humeral capitellum that occurs in older children and adolescents in the second decade of life [2]. We are reporting such a case in a 6-year-old boy.
A 6-year-old boy was brought by his mother in the outpatient clinic with complains of pain and difficulty in moving his right elbow following a fall while playing with his siblings at home. There was no history of any constitutional symptoms. The medical and family history was unremarkable. Since initial examination was near normal with minimal tenderness over elbow, diagnosis of contusion was made. He was treated with long arm splint and pain medication. At 2-week follow-up visit, he had persistent pain and elbow examination revealed mild swelling, subtle tenderness over lateral side of elbow and limitation of extension by 20°. A repeat radiograph of both the elbows in AP and lateral view was ordered. It showed joint effusion (star) (Fig. 2), irregular delineation of the articular contour of the capitellum with a radiolucent line in the subchondral bone (black arrows) and faint sclerosis of the capitellum (white arrows) (Fig. 1, 2).
These are the classical radiological features of osteochondrosis of humeral capitellum (Panner’s disease).
Her mother was explained about the condition and its prognosis. The boy was treated with continued elbow immobilization for further 2 weeks and advised to come for follow-up but unfortunately, he was lost to the follow-up. Almost after 5 years, we could communicate on telephone with her mother but they were unable to visit the hospital for follow-up examination and X-ray. She said that her son has completely recovered and has no pain, swelling, deformity, or limitation of movement. He is back to his normal activity.
Osteochondrosis of humeral capitellum is a rare disease and it affects the growing immature skeleton [3]. The humeral capitellum is the most frequent site of osteochondrosis in the elbow [3]. Dr. Dane Panner, a Danish Orthopedic surgeon, first described the radiological changes of the capitellum in young adult, in 1927 and thereafter, it began to be known as Panner’s disease [4]. Although its etiology and pathogenesis are not very well understood, he considered the etiology of these radiographic changes in the capitellum of the humerus to be similar to osteochondrosis of the hip epiphysis (Legg–Calvé–Perthes) described 17 years earlier [5]. Some author believe that primary etiological factor of the Panner’s disease is an endocrine disturbance causing disordered endochondral ossification while other believes it to be due to overuse and repetitive abnormal valgus compressive forces exerted across the radiocapitellar joint in pediatric elbow causing microvascular trauma leading to possible ischemic injury of capitellum [6]. However, trochlea is not affected in Panner’s disease though it derives from the same cartilaginous mass as the capitellum [7]. Ruch and Poehling suggested that Panner’s disease and OCD are a continuum of disordered endochondral ossification, with overall outcome dependent on age and severity of the lesion [8]. It is most prevalent in the first decade of life and primarily unilateral in distribution affecting dominant extremity. It typically affects boys because of delayed appearance and maturation of secondary ossification centers and increased susceptibility to trauma and stresses of early childhood activities [9]. Claessen et al. in one review article reported that 90% of patients were boys. Onset may be insidious; however, there is often history of mild trauma or repetitive stress more typically a valgus stress or increased axial load to the elbow. He reported such history in 43% of cases and were involved in sports-related activities such baseball, gymnastic and handball. Pain, swelling, and limitation of elbow movements are the most common presenting clinical symptoms. Claessen et al. reported pain in 66%, swelling in 55%, and limitation of elbow movement in 62% of patients in his review article. Typically, there is a limitation of extension movement approximately by 20° rather than flexion movement deficit. The symptoms are exacerbated by activity and relieved by rest. Both radiologically and histologically, the involved sites possess several features of the ischemic necrosis. The changes in the morphology, contour irregularities, flattening of articular surface, fragmentation and collapse, radiolucent areas, and increased density of the capitellum are the typical radiological features on plain X-ray. To reduce the errors in diagnosis, it is wise to use uniform names and description of radiographic signs for Panner’s disease. MRI is more sensitive and may be helpful in diagnosing this condition before obvious radiographic changes become apparent. It may also be useful to differentiate from other conditions such as OCD or tuberculous osteomyelitis [10]. T1 images show decreased signal intensity of capitellum with dark rim and T2 images show increased intensity, cortical irregularity and elbow effusion [10]. A useful diagnostic feature on CT scan though rare is the detection of a subchondral vacuum phenomenon [11]. It represents a gas accumulation within the subchondral cleft and it is a sign of bone ischemia. It may indicate avascular necrosis and impending articular collapse, similar to the Legg–Calvé–Perthes disease. The vacuum phenomenon disappears when repair and reossification eventually occurs [11]. The radiological improvement occurs over 1–3 years [12]. Studies to date agree that osteochondrosis passes through stages, similar to Legg–Calvé–Perthes disease [12]. Panner’s disease is probably underdiagnosed, because the symptoms may be overlooked and findings on radiographs can be subtle [12]. It is a self-limiting condition and natural history typically involves regeneration and reconstitution of the capitellum in most of the patients with full functional recovery without any residual morbidity or deformity. In general, conservative treatment is advised. Splinting for a short period (3–6 weeks), anti-inflammatory medication, and reduction of elbow activities that increase valgus stress may help relieve pain and return to normal elbow motion and function in most of the cases [13]. Sometimes, if the symptoms fail to resolve with conservative measures, arthroscopic assessment of the articular cartilage has been recommended. If the articular surface is intact, drilling of epiphyseal subchondral bone may stimulate healing. It should, however, be stressed that surgical treatment of Panner’s disease is extremely uncommon [14]. Panner’s disease is often confused with OCD of the humeral capitellum in initial stages due to similar clinical presentation. The similarities between these diseases are sex ratio (male preponderance), location of lesion (capitellum), dominant hand affection, similar causes (repeated injuries and ischemia), and early diagnosis facilitating full recovery. However, they differ in terms of patient’s age, course of the disease, morphology of lesions, duration, treatment, and resultant prognosis. Panner’s disease is reported to occur in boys younger than 10 years (7–12 years) while OCD occurs in older children and adolescent (10–15 years) [14]. Pain, swelling, and limitation of elbow movements are the common symptoms in both entities; however, mechanical symptoms such as intermittent catching and locking of elbow are seen more commonly in OCD due lesion instability or formation of loose bodies [14]. On plain radiograph, capitellum shows irregular contour, flattening, lytic defect with sclerotic borders, and fragmentation. These changes are more generalized and central involving whole capitellum in Panner’s disease while in OCD, these are more localized and peripheral located on surface resulting into loose body formation [14]. These differences are more striking and clear on MRI. Panner’s disease is considered as benign and self-limiting condition. It is commonly treated conservatively with short duration of splinting (3–6 weeks), pain medication, and modification of activities that reduce lateral elbow stresses. On the other hand, treatment of OCD depends on size and stability of the lesion. Small and stable lesion has potential to heal with conservative treatment. Unstable small lesions (≤12 mm) may require arthroscopic debridement or loose body removal and subchondral bone drilling [14]. Unstable large lesions (≥12 mm) require reconstruction of articular surface with osteochondral autograft transplantation or bone peg fixation [14]. Prognosis in case of Panner’s disease is much better with expectant full functional recovery without any residual deformity in most cases. While in OCD, prognosis is less favorable. Bauer et al. reported that in 31 patients with OCD at a mean follow-up of 23 years, 50% had persistent elbow symptoms and radiographic osteoarthritis [15].
Osteochondrosis of humeral capitellum though rare is a known condition. It may be overlooked or missed in the initial encounter with the patient. High degree of awareness is required and diagnosis can be made with utmost care based on age of presentation, clinical signs, and clearly recognizable plain radiographic features of joint effusion, irregular articular outline with radiolucent line in subchondral bone and faint sclerosis of capitellum. Confusion with OCD can be avoided that occurs at a little later stage of childhood.
Osteochondrosis of humeral capitellum though rare in young children high level of vigilance and awareness is required to adequately diagnose and treat appropriately.
References
- 1.Claessen FM, Louwerens JK, Doornberg JN, van Dijk CN, Eygendaal D, van den Bekerom MP. Panner’s disease: Literature review and treatment recommendations. J Child Orthop 2015;9:9-17. [Google Scholar]
- 2.Sakata R, Fujioka H, Tomatsuri M, Kokubu T, Mifune V, Inui A, et al. Treatment and diagnosis of Panner’s disease. A report of three cases. Kobe J Med Sci 2015;61:E36-9. [Google Scholar]
- 3.Kobayashi K, Burton KJ, Rodner C, Smith B, Caputo AE. Lateral compression injuries in the pediatric elbow: Panner’s disease and osteochondritis dissecans of the capitellum. J Am Acad Orthop Surg 2004;12:246-54. [Google Scholar]
- 4.Panner HJ. An affection of the capitulum humeri resembling Calve Perthes’ disease of the hip. Acta Radiol 1929;10:234-42. [Google Scholar]
- 5.Sty JR, Boedecker R. Panner’s disease (osteonecrosis of the capitellum). Clin Nucl Med 1978;3:117. [Google Scholar]
- 6.Kim DH, Kim TG, Heo YM, Hwang CM, Jun JB, Yi JW. Panner’s disease occurred in a five-year-old child: A preliminary case report. Clin Shoulder Elbow 2016;19:176-8. [Google Scholar]
- 7.Heller CJ, Wiltse LL. Avascular necrosis of the capitellum humeri (Panner’s disease). A report of a case. J Bone Joint Surg Am 1960;42:513‑42 [Google Scholar]
- 8.Ruch DS, Poehling GG: Arthroscopic treatment of Panner’s disease. Clin Sports Med 1991;10:629-36. [Google Scholar]
- 9.Duthie RB, Houghton GR: Constitutional aspects of the osteochondroses. Clin Orthop 1981;158:19-27. [Google Scholar]
- 10.Davis KW. Imaging pediatric sports injuries: Upper extremity. Radiol Clin North Am 2010;48:1199‑48:. [Google Scholar]
- 11.Anisau A, Posadzy M, Vanhoenacker F. Panner’s disease: The vacuum phenomenon revisited. J Belgian Soc Radiol 2018;102:67. [Google Scholar]
- 12.Stoane JM, Poplausky MR, Haller JO, Berdon WE. Panner’s disease: X-ray, MR imaging findings and review of the literature. Comput Med Imaging Graph 1995;19:473-6. [Google Scholar]
- 13.Smith MG. Osteochondritis of the humeral capitulum. J Bone Joint Surg Br 1964;46:50-4. [Google Scholar]
- 14.Mishra M, Agarwal A. Think beyond tuberculosis: It can be Panner’s disease in the Child’s Elbow. J Orthop Traumatol Rehabil 2018;10:79-82. [Google Scholar]
- 15.Bauer M, Jonsson K, Josefsson PO, Lindén B. Osteochondritis dissecans of the elbow. A long-term follow-up study. Clin Orthoc Relat Res 1992;284:156-60. [Google Scholar]