Surgeons should work with other specialists to normalize parathyroid hormone levels in patients with secondary hyperparathyroidism to optimize the likelihood of achieving bony union following insufficiency fractures.
Dr. Kenneth A Egol,
301 E 17th Street, Suite 1402 New York, NY 10003, United States.
E-mail: kenneth.egol@nyulangone.org
Introduction: Insufficiency fractures are uncommon injuries, but may occur in the lower extremity due to repetitive stress on abnormal bone tissue. Management of these injuries may include weight bearing restrictions, bracing, or even surgical intervention. In addition, a proper metabolic healing environment is required to encourage healthy bone growth following an injury.
Case Presentation: This case report discusses a patient who underwent surgical repair of a closed nondisplaced proximal tibia insufficiency fracture. Several reoperations were required due to hardware failure and bone resorption following operative nonunion repair. It was determined that her elevated PTH due to end-stage renal disease (ESRD) likely inhibited bone regeneration during the course of her treatment. A successful kidney transplant rapidly normalized the patient’s PTH levels and permitted bony healing of her tibial stress fracture.
Conclusion: Several studies have demonstrated a relationship between metabolic abnormalities and fracture healing. We are the first to present a case where bony union in an ESRD patient with secondary hyperparathyroidism was only achieved following a kidney transplant. Surgeons should be cognizant of the effect that metabolic abnormalities may have in the development of insufficiency fractures and subsequently achieving bony union following such fractures.
Keywords: Fracture, non-union, intramedullary nail, hyperparathyroidism, end-stage renal disease.
Stress fractures are a painful condition caused by repetitive stresses associated with weight-bearing and cyclical loading [1]. In the literature, stress fractures can be characterized as either fatigue or insufficiency fractures. Fatigue fractures result from repetitive stresses on normal bone tissue, while insufficiency fractures are a type of fracture secondary to a normal stress applied to abnormal bone tissue [1]. Treatment for these injuries is dependent on the location and severity of the fracture, but it typically includes restraint from physical activity with analgesic medication for pain coverage [1, 2]. In addition, these injuries may require surgery if the fracture goes on to nonunion or if the patient suffers from repetitive insufficiency fracture injuries [2]. Elderly individuals and postmenopausal women have an increased risk of sustaining insufficiency fractures due to their increased predisposition to osteoporosis [1].
At a cellular level, bone healing and homeostasis are dependent on hormones and growth factors to properly balance osteoblast and osteoclast activity [3]. One of these hormones, parathyroid hormone, is crucial to this balance. Chronic hyperparathyroidism leads to increased bone remodeling and resorption through increased stimulation of osteoclasts [4]. We present a case of tibial nonunion in a patient with end-stage renal disease (ESRD) and secondary hyperparathyroidism that did not heal until the patient received a renal transplant.
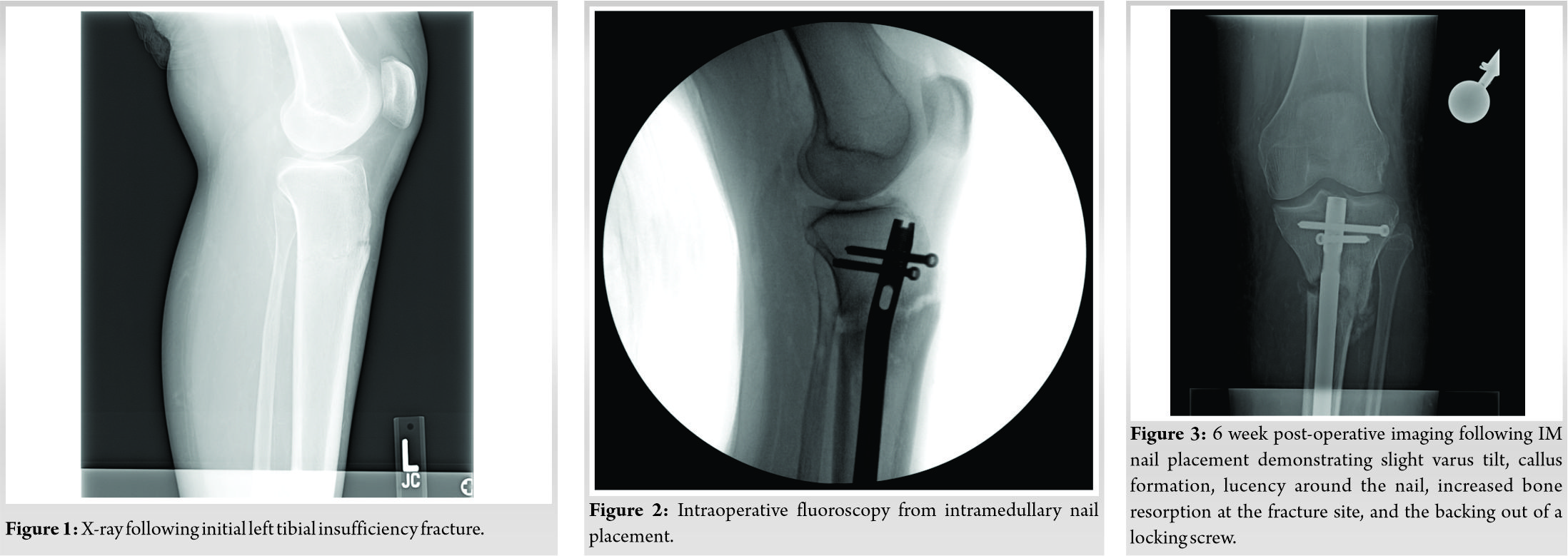
A 44-year-old female with a history of ESRD secondary to Type 1 diabetes mellitus on hemodialysis presented to clinic with left leg pain 3 weeks after injuring her knee stepping out of her car. Immediately following the injury, she presented to an urgent care center, where plain radiographs demonstrated an anterior unicortical tibial disruption. Following appropriate orthopedic referral, additional X-rays, a computerized tomography (CT) scan, and magnetic resonance imaging were obtained, which confirmed a nondisplaced “stress” fracture of the left proximal tibia (Fig. 1). After a thorough discussion of treatment options in clinic, she elected non-operative treatment and was placed in a patella tendon bearing (PTB) brace.
The patient utilized the brace for 6 weeks without resolution of symptoms. At this time, plain radiographs revealed progression and widening of the tibial fracture line. She continued to have pain in her left leg and was indicated for surgical repair. She underwent a reamed tibial intramedullary nail (IMN) 6 days later. The surgery was uncomplicated and adequate hardware placement was confirmed with intraoperative fluoroscopy (Fig. 2). At the time of surgery, the surgeon was satisfied with the fixation. She was discharged later that day with a posterior plaster splint.
At 6 weeks post-operative, the patient reported persistent pain over her left proximal tibia and a sensation that her left leg was bowing out making it difficult for her to walk. X-rays were suggestive of a slight varus tilt and also demonstrated callus formation, lucency around the nail, increased bone resorption at the fracture site, and the backing out of a locking screw (Fig. 3). The patient and surgeon decided it was best to pursue a revision surgery the following week with an additional lateral plate to increase construct stability. It was also discovered at the time that the patient’s PTH was over 1200 pg/ml, which was thought to be secondary to her ESRD. Her nephrologist was consulted. Discussion was centered around the need for a parathyroidectomy to correct her PTH levels in addition to supporting healthy bone formation.
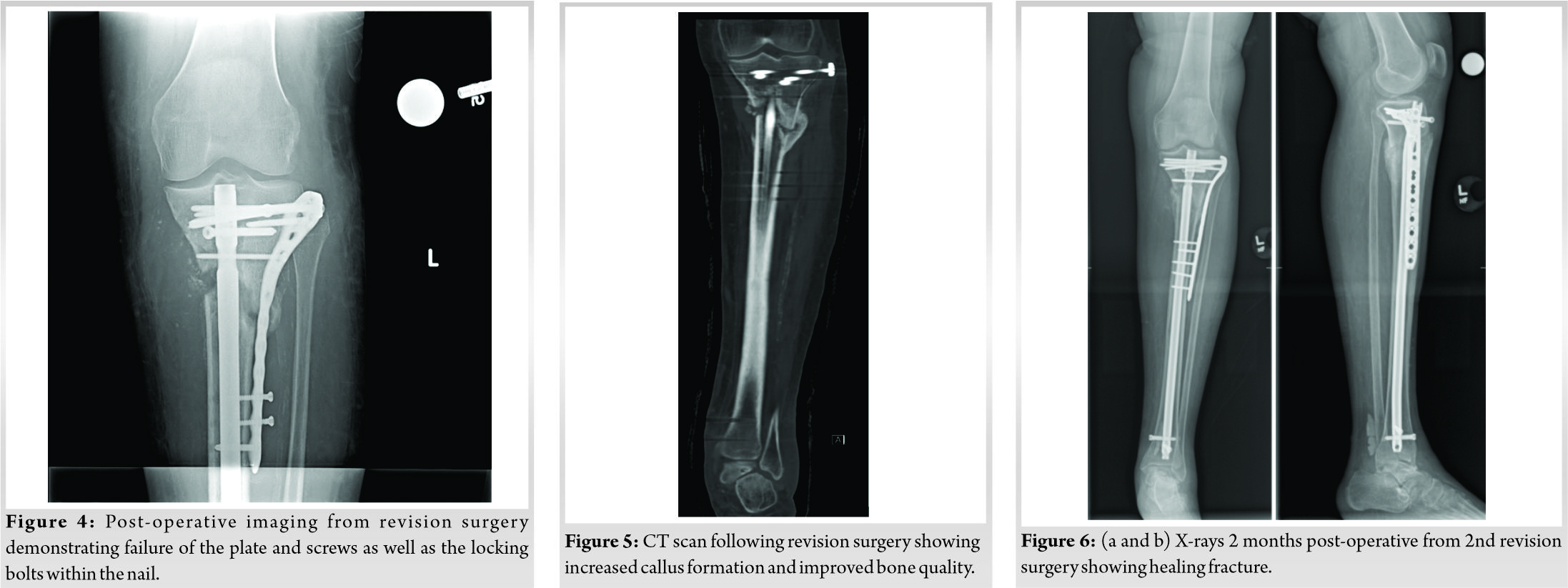
At the revision operation, the fracture was grossly mobile around the IM nail and screws. The patient underwent an additional locking plate with linkage of the plate screws and IM nail. In addition, an iliac crest aspirate was combined with demineralized bone matrix that was packed at the fracture site. The patient was kept non-weight bearing. Over the next month, radiographs demonstrated failure of the plate and screws as well as the locking bolts within the nail (Fig. 4). Once this secondary failure was identified, she was placed in a PTB cast, which was changed every few weeks.
Shortly after her revision surgery, she received a renal transplant which ultimately resulted in her PTH declining to 107 pg/ml. Over the next several months following transplant, she continued to improve clinically with regard to her fracture. She underwent multiple CT scans, which revealed increased callus formation, but incomplete healing at the fracture site with some varus alignment (Fig. 5). Using the CT scans, in consultation with a musculoskeletal radiologist, it was determined that the overall bone quality in the proximal tibia had improved significantly. A discussion was had with the patient as to pursuing another surgery, now that her bone health had improved. The patient elected to pursue operative management for the nonunion. At 6 months post-operative from her revision surgery and 8 months following her initial surgery, she underwent a second revision with revision plate placement at the nonunion site as well as exchange of locking bolts in the IM nail. The patient returned to clinic at 1, 2, and 3 months post-operative from this 2nd revision surgery, where she reported her pain was well controlled and she was ambulating with one crutch. Radiographs demonstrated a radiographically healing fracture, good tibial alignment, and no signs of hardware failure (Fig. 6a, b). At the patient’s 1 year follow-up visit from her initial IMN surgery (9 months after 1st revision and 3 months after 2nd revision), she was pain free and ambulating without difficulty. X-rays at this visit showed that her fracture had fully healed (Fig. 7a, b).
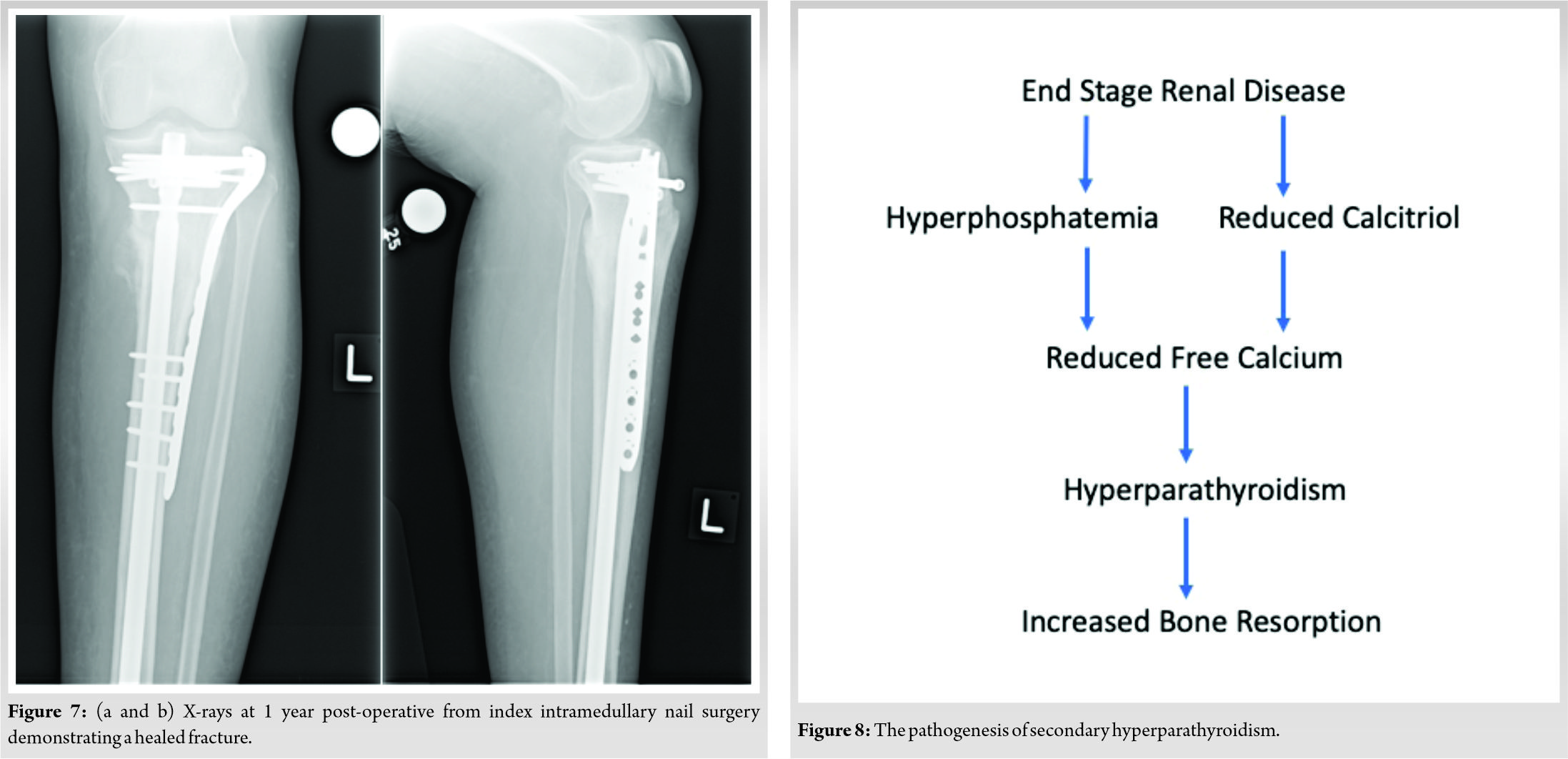
In this case report, we present a patient with ESRD and renal osteodystrophy induced by secondary hyperparathyroidism who sustained a left tibial insufficiency fracture and subsequent nonunion requiring multiple surgeries. The issues with healing seen in this patient are consistent with our understanding of the relationship between elevated PTH levels and bone regeneration. Under normal physiological circumstances, the parathyroid gland releases PTH in response to low circulating calcium levels. PTH acts on bone to increase reabsorption of calcium and the kidneys to convert Vitamin D to its most active form calcitriol (1,25 dihydroxyvitamin D). Calcitriol then mainly functions to increase calcium absorption in the gut. In ESRD, the kidneys have trouble converting Vitamin D to calcitriol, which leads to less calcium absorption in the gut and eventually low circulating calcium levels (Fig. 8). In addition, the excess of circulating phosphate seen in ESRD binds to free calcium, and thus further lowers calcium levels. The low circulating calcium levels then cause continuous secretion of PTH, leading to continuous calcium reabsorption from bone and subsequent poor bone health as seen in our patient [5].
Daily exogenous of a PTH fragment have been shown to have an anabolic effect on healing which has led to its FDA approval for prevention of osteoporotic fractures [6]. Several small studies in humans have even shown that daily injections of a PTH analogue may be an effective treatment for delayed union and nonunion [7]. However, it is known that constant chronically elevated PTH levels support bone resorption [4], and thus gives PTH inhibitory properties against bone regeneration as seen in this case. In our patient who had PTH levels consistently elevated over 1000 pg/nl during the several months following her initial injury, we suspect her hyperparathyroidism played a major role in the development of her fracture, which was secondary to a normal stress activity and ultimately preventing her fracture from healing.
Several retrospective studies have demonstrated a link between metabolic abnormalities and fracture healing. In one retrospective study, 31 of 37 patients who were referred to an endocrinologist for persistent nonunion were subsequently diagnosed with a metabolic or endocrine abnormality including Vitamin D deficiency, calcium imbalances, central hypogonadism, thyroid disorders, and parathyroid hormone disorders [8]. In another study, 30 patients with tibial nonunion were matched by fracture type, surgical treatment, sex, age, and body mass index to 32 patients with normal bone healing following a low energy tibial fracture. The authors showed a statistically significant difference in Vitamin D levels between both groups, with the nonunion group having lower Vitamin D levels [9]. The study also showed a higher prevalence of hyperparathyroidism in the non-union group [9]. While none of these studies are able to demonstrate a causal relationship between these lab abnormalities and nonunion, they support our hypothesis that our patient’s lab abnormalities played a role in her failed bone regeneration.
There are several medical treatments that can be explored for secondary hyperparathyroidism in ESRD including a low phosphate diet, phosphate binders, Vitamin D derivatives, and calcimimetics [5]. Lowering phosphate levels frees up phosphate-bound calcium, while Vitamin D derivatives help with absorption of calcium in the gut [5]. Calcimimetics work by increasing the sensitivity of calcium sensing receptors on the parathyroid gland [5]. Surgical management with parathyroidectomy is indicated when patients do not respond to medical treatment [5]. Our patient was able to receive a kidney transplant, so she was ultimately able to avoid parathyroidectomy. We believe restoration of our patient’s metabolic homeostasis following her kidney transplant, specifically 10-fold decrease of her PTH levels, played a crucial role in allowing her tibial nonunion to heal. Despite still being just below twice normal levels, it was felt that for her kidney transplant status, the number was sufficient for proper kidney health and further lowering could have been problematic.
There have been several other case reports in the literature where patients with hyperparathyroidism went on to develop nonunion following long bone fractures [10, 11, 12, 13]. One of these case reports describes resolution of nonunion after the patient underwent a parathyroidectomy [13]. To the best of our knowledge, we are first to present a patient with ESRD and secondary hyperparathyroidism with a nonunion that healed following a kidney transplant. While there are limits to any conclusions that can be made from a case report, ours supports the existing literature regarding the role that metabolic abnormalities have in nonunion. Further large-scale prospective studies examining the relationship between these metabolic abnormalities and nonunion are required to draw any major conclusions.
We present a case where a patient with ESRD and renal osteodystrophy induced by secondary hyperparathyroidism sustained an insufficiency fracture and subsequent nonunion. Only after receiving a kidney transplant, her tibial fracture was able to achieve bony union. Her PTH levels normalized following transplantation, which played a crucial role in her fracture healing.
Surgeons treating patients with similar hormone imbalances should be cognizant of the effects that metabolic imbalances may have on the rate of bony union. Therefore, these patients should be counseled on their elevated risk of nonunion and the importance of consistent follow-up to assess radiographic fracture healing. Finally, surgeons treating these patients should work with other specialists to mitigate hormone imbalances and optimize fracture healing..
References
- 1.Matcuk G, Mahanty S, Skalski M, Patel DB, White EA, Gottsegen CJ. Stress fractures: Pathophysiology, clinical presentation, imaging features, and treatment options. Emerg Radiol 2016;23:365-75. [Google Scholar]
- 2.Patel D, Roth M, Kapil N. Stress fractures: Diagnosis, treatment, and prevention. Am Fam Physician 2011;83:39-46. [Google Scholar]
- 3.Siddiqui J, Partridge N. Physiological bone remodeling: Systemic regulation and growth factor involvement. Physiology (Bethesda) 2016;31:233-45. [Google Scholar]
- 4.Wein M, Kronenberg H. Regulation of bone remodeling by parathyroid hormone. Cold Spring Harb Perspect Med 2018;8:a031237. [Google Scholar]
- 5.Busaidy NL, Lahoti A, Hanley DA. Secondary hyperparathyroidism. In: Khan A, Clark O, editors. Handbook of Parathyroid Diseases. Boston, MA: Springer; 2012. [Google Scholar]
- 6.Campbell EJ, Campbell GM, Hanley DA. The effect of parathyroid hormone and teriparatide on fracture healing. Expert Opin Biol Ther 2015;15:119-29. [Google Scholar]
- 7.Canintika AF, Dilogo IH. Teriparatide for treating delayed union and nonunion: A systematic review. J Clin Orthop Trauma 2020;11 Suppl 1:S107-12. [Google Scholar]
- 8.Brinker MR, O’Connor DP, Monla YT, Earthman TP. Metabolic and endocrine abnormalities in patients with nonunions. J Orthop Trauma 2007;21:557-70. [Google Scholar]
- 9.Pourfeizi HH, Tabriz A, Elmi A, Aslani H. Prevalence of Vitamin D deficiency and secondary hyperparathyroidism in nonunion of traumatic fractures. Acta Med Iran 2013;51:705-10. [Google Scholar]
- 10.Kinoshita M, Naito K, Aritomi K, , Sugiyama Y, Nagura N, Goto K, et al. Forearm nonunion caused by hyperparathyroidism with 7 years follow up: A case report. Int J Surg Case Rep 2017;38:158-62. [Google Scholar]
- 11.Juliano JS, Juliano PJ. Hyperparathyroidism presenting as a nonunion of the femur: Case report and review of the literature. Mil Med 2000;165:569-71. [Google Scholar]
- 12.Sauvé PS, Suliman IG, Calder JD. Primary hyperparathyroidism presenting as delayed fracture union. Knee Surg Sports Traumatol Arthrosc 2009;17:551-4. [Google Scholar]
- 13.Lee F, Lee JJ, Liu TP, Cheng SP. Parathyroidectomy improves fracture nonunion in hyperparathyroidism. Am Surg 2015;81:E36-7. [Google Scholar]








