Robotic arm assistance in revision total knee arthroplasty is a viable technique and can result in satisfactory alignment of components and excellent patient short term outcomes.
Dr. Kevin Steelman,
Department of Orthopaedic Surgery, Harper University Hospital, Detroit, Michigan, United States.
E-mail: krsteelman1@gmail.com
Introduction: With increasing numbers of knee arthroplasty procedures being performed, revision total knee arthroplasty (TKA) remains a challenge to orthopedic surgeons. The use of robotics in primary joint arthroplasty is also increasing due to better technology and surgeon familiarity. Robotic arms have the ability to execute bone cuts within 1 mm of a preoperative plan, can measure soft tissue gap tension, and can plan femoral and tibial augments and rotation. The use of robotic arm assistance for revision TKA, however, has not been documented in the literature.
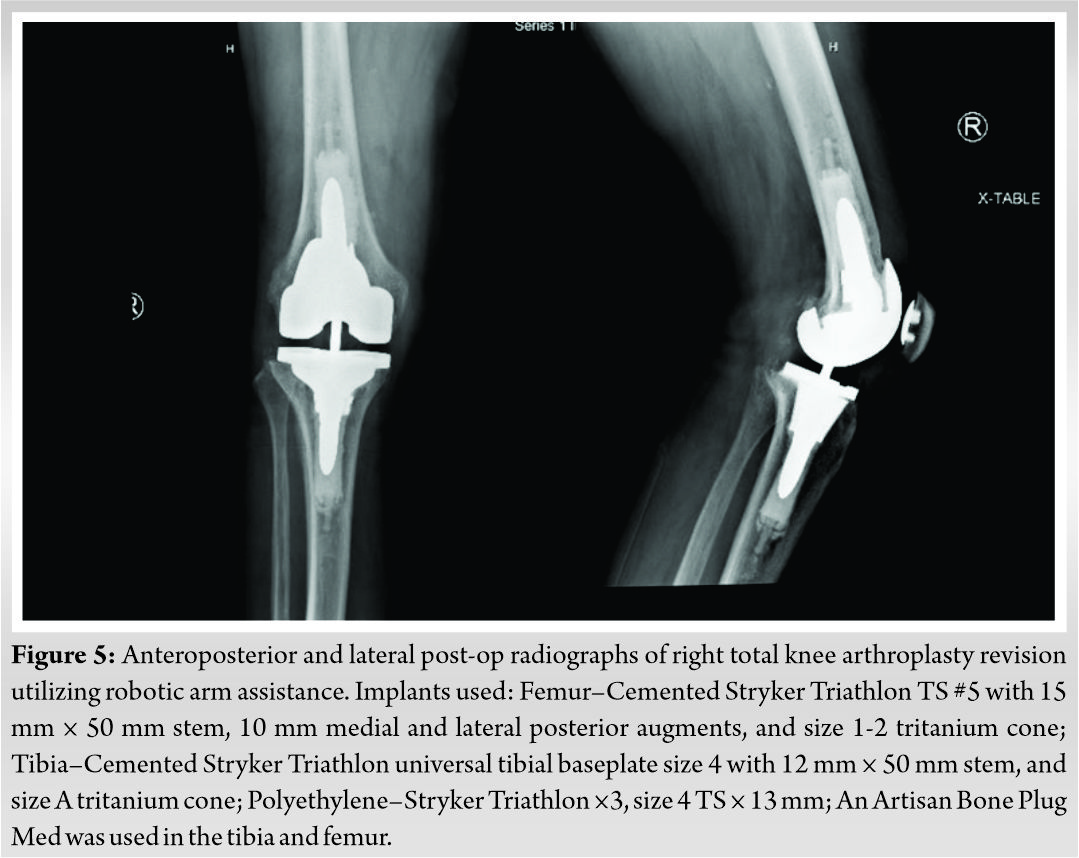
Case Report: We present a case describing a novel technique in which the Mako robot (Stryker, Ft. Lauderdale, FL) was utilized for revision of a failed primary TKA secondary to aseptic loosening. The patient is a 68-year-old Caucasian male who underwent right revision TKA with robotic assistance. Stryker Triathlon TS implants were utilized with the use of both femoral and tibial cones and medial and lateral posterior femoral augments. He had satisfactory component alignment based on postoperative radiographs, and excellent clinical outcomes 6 months postoperatively.
Conclusion: The use of robotic arm assistance in revision TKA for failed primary TKA is a novel technique and resulted in excellent operative outcomes in this case. Further study should be done to confirm its use in revision TKA.
Keywords: Total knee arthroplasty, robotic, revision, total knee arthroplasty.
Robotic arm assistance in total joint arthroplasty is becoming more popular in the orthopedic field. Recent data have shown a significant increase in robotic utilization in hip and knee arthroplasty in both hospitals and surgeons over the past decade [1]. Current applications of robotic assistance for joint arthroplasty include unicompartmental knee arthroplasty (UKA), total hip arthroplasty, and primary total knee arthroplasty (TKA). Robotic-assisted TKA has been shown to result in more accurate bone cuts [2], fewer mechanical axis outliers [3], and more optimal alignment when compared to manual TKA [4].
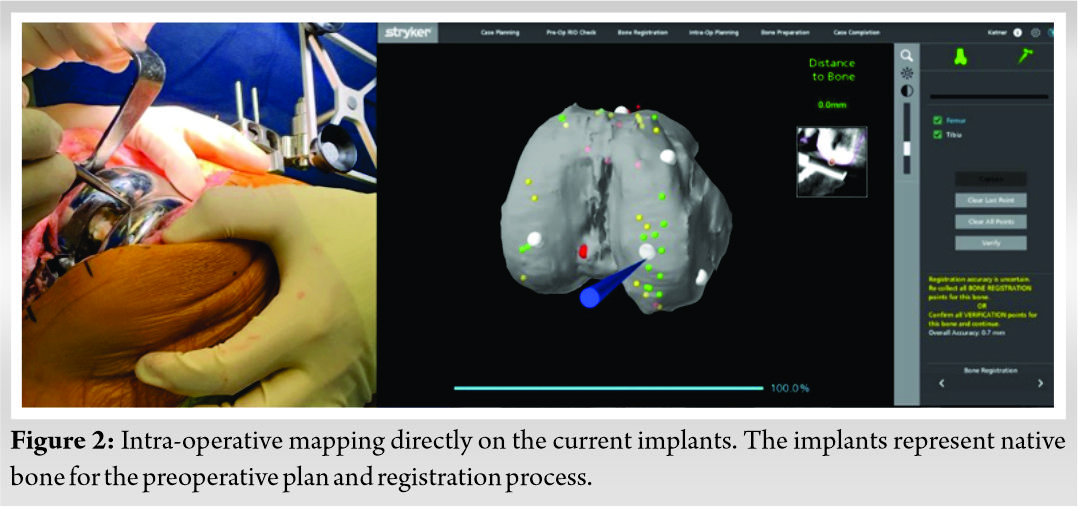
The number of revision TKA (rTKA) cases in the United States is also increasing [5]. Common reasons for rTKA include infection, aseptic loosening, and periprosthetic fracture [6]. rTKA poses numerous challenges to both the surgeon and patient. These include malrotation of components, instability, excessive loss of bone stock, and damage to nearby anatomical structures. At our institution, robotic arm-assisted surgeries are performed using Mako technology (Stryker, Ft. Lauderdale, Florida). Performing revision arthroplasty surgery with robotic arm assistance is considered “off-label” as there is no application within the Mako system to support it. However, by obtaining a preoperative computed tomography (CT) scan and using the normal preoperative Makoplasty protocol, a patient’s current implants can be treated as if they were native bone to develop a preoperative plan.
There is a paucity of literature on robotic-assisted rTKA including just one case report [7] and one retrospective review [8]. All previous studies demonstrated the use of robotics in conversion of failed UKA to TKA. To the knowledge of the authors, this is the first case of rTKA with robotic arm assistance due to failure of primary TKA.
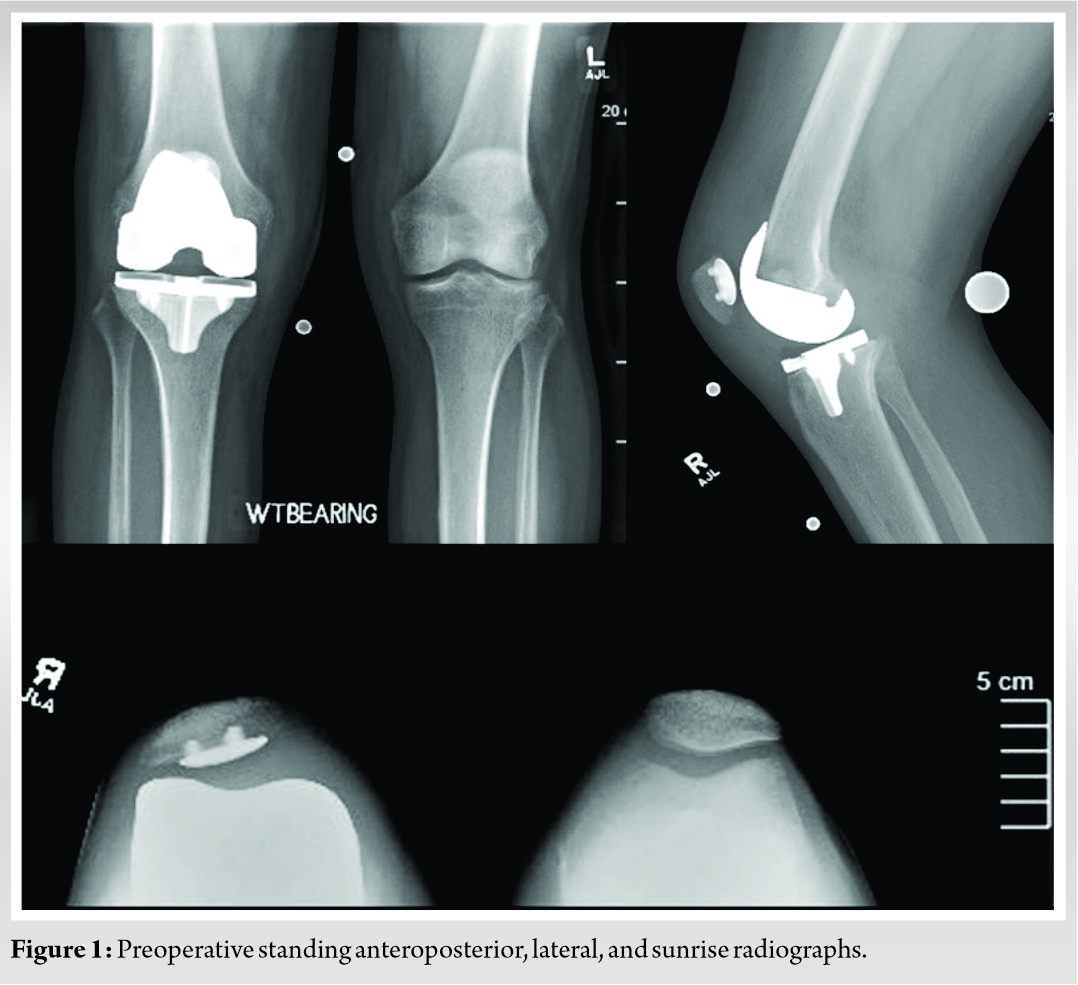
This is a case of a 68-year-old male who presented to our institution for evaluation of the right TKA. He underwent his index TKA in December 2018 at an outside institution. He did not have any significant medical history. He had a good recovery after surgery, but 6 months postoperatively he developed discomfort in the right knee. He presented to our office approximately 2 years after his index procedure for evaluation of his right knee after failing conservative management (Fig. 1). He subsequently underwent testing to rule out component loosening and infection. His clinical examination as well as a bone scan suggested loosening of the tibial component. His laboratory workup including erythrocyte sedimentation rate, C-reactive protein, white blood cell, and joint aspiration was negative for prosthetic joint infection. After a lengthy discussion regarding the risks and benefits of the procedure, he elected to proceed with right rTKA with Mako robotic assistance. A Stryker Triathlon revision knee system was planned to be used for this case.
In the operating room, the patient underwent spinal anesthesia. Physical examination confirmed a flexion stop at 105 degrees, a 15-degree extension lag, and stable varus/valgus balance. A tourniquet was used during the procedure and the limb was prepped with chlorhexidine prior to draping.
A midline incision was used over the previous surgical scar, and a medial arthrotomy was performed. On inspection of the joint, the femoral and tibial components appeared to be appropriately sized and in good rotation. The patellar button was also of appropriate size. The knee was found to be tight in flexion and somewhat loose in extension. The 9 mm polyethylene tray was first removed and then the femoral and tibial checkpoints along with the Mako array pins were secured into the distal femur and proximal tibia. Hip center of rotation was then obtained, followed by plotting the femoral and tibial reference points on the existing components (Fig. 2).
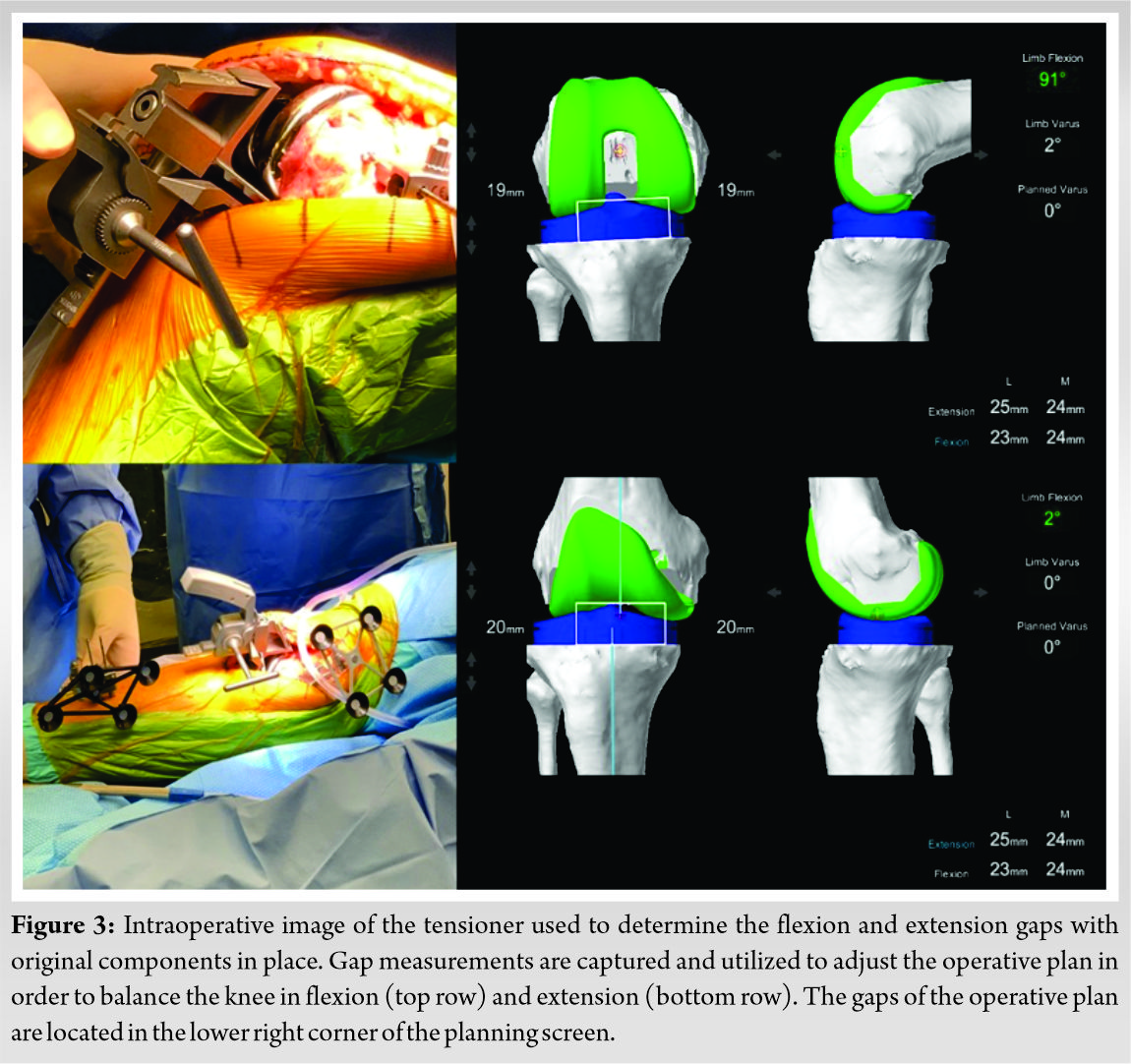
The 9 mm polyethylene insert was then placed back into the tibial tray in order to obtain our starting flexion and extension numbers. We used a tensioner (Fig. 3) with the implants in place to determine our flexion and extension gaps.
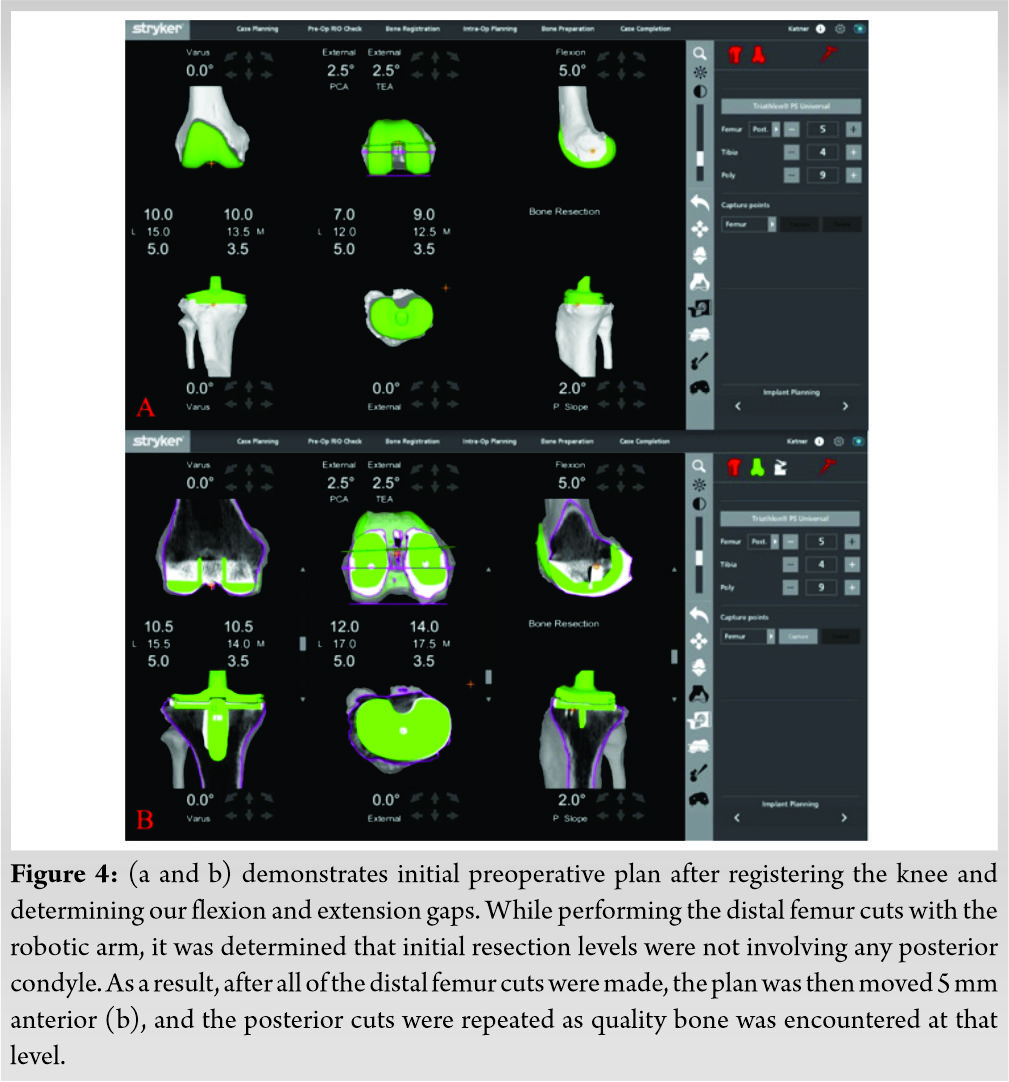
This information was used for our operative plan to determine our resections and possible needs for augmentation (Fig. 4a). The press-fit femoral and tibial components were then carefully removed with an osteotome. This did not result in any significant bone loss to either the femur or tibia. The patellar button was thoroughly examined and found to be well-fixed and in good position and was left intact. Utilizing our operative plan, the Mako robotic arm with saw attachment was used to perform very minimal fresh cuts to the distal, anterior, and posterior femur, as well as the chamfer cuts. The posterior femur cuts did not resect any bone either medially or laterally. By using robotic technology, we were able to move the plan for the posterior femoral cut 5 mm anterior in order to resect to the level of posterior bone. With this adjustment, we were able to plan to use 5 mm posterior augments both medially and laterally (Fig. 4b). We then turned our attention to the tibia and again performed a robotically assisted minimal fresh cut according to our Mako plan.
An intramedullary tibial alignment rod was used for centering the conical reamer in the tibia, and this was reamed to a size A cone. The TS femoral box cuts were performed, and conical reaming was again performed over an intramedullary guide on the femur to a size 1-2 cone. Trial components were then inserted and the knee was found to balance very well with a 13 mm trial polyethylene insert. All remaining cement was then removed from the bone surfaces, and remaining osteophytes were removed from around the patella. The joint was copiously irrigated with Irrisept (Irrimax Corp, Gainseville, FL) and normal saline. The tibial and femoral components were then cemented into place. A 13 mm polyethylene insert was used and the knee balanced quite well in full extension, mid flexion, and flexion to 90 degrees. The knee ranged from 0 to 135 degrees and had smooth and centered patellar tracking. Post-operative AP and lateral radiographs can be seen in fig5.
The patient was given a postoperative adductor canal block. His postoperative course was uneventful. He completed his hospital physical therapy regimen and was discharged home on postoperative day two in excellent condition. The patient followed up at 2 weeks, 6 weeks, 3 months, and 6 months postoperatively. He participated in 3 months of outpatient physical therapy to help with his range of motion and strength. The patient’s visual analogue scale (VAS) pain scores decreased at each clinic visit. By his 6-week appointment, his VAS pain score was 1/10 and he was not taking any narcotic pain medication. At most recent follow-up, the patient was able to ambulate without assistive devices and only took ibuprofen for occasional soreness after strenuous activity. His range of motion was 0-135 degrees, and his strength was equal to his other leg.
Robotic-assisted TKA has been and continues to be, developed to increase the accuracy, precision, and safety during knee arthroplasty [9]. There are numerous studies suggesting that robotic-assisted knee arthroplasty results in more accurate bone cuts, component placement, and deformity correction [2, 3, 10]. Several studies have also reported on decreased soft tissue complication rates associated with robotic-assisted TKA [11, 12] including one cadaver study that showed decreased damage to the PCL when comparing robotic-assisted and manual cruciate-retaining TKA [13]. In addition to accuracy and safety, a number of studies have recently been published addressing patient satisfaction after robotic TKA, many of which suggest that robotics may help improve patient satisfaction and clinical outcomes [14, 15].
Revision knee arthroplasty is an increasing challenge for the orthopedic surgeon, with rising case numbers secondary to infection, aseptic loosening and instability, peri-prosthetic fracture, and progression of arthritic disease [6]. While there continues to be an abundance of research dedicated to the use and outcomes of robotic-assisted primary UKA and TKA, there are currently only two studies focusing on the use of robotics in revision knee arthroplasty. Both of these studied UKA conversion to TKA. An exhaustive literature review utilizing PubMed was performed using the keywords: Robotic; Revision knee arthroplasty; TKA; UKA.
In 2020, Kalavrytinos et al. presented the first described case of robotic conversion of failed UKA to TKA [7]. This study presented an 87-year-old female with a stiff and painful knee with a malpositioned UKA resulting in significant varus deformity. Similar to our presented case, Kalavrytinos et al. utilized Mako technology, Stryker Triathlon implants, and they developed an operative plan that treated the patient’s current implants as native bone. The authors also utilized robotic technology to over-resect the medial tibia in order to place 10 mm augments, similar to what we did on the medial and lateral posterior femur, which also required augmentation. Their final components were a Stryker CR Triathlon knee with an 11 mm polyethylene insert and 10 mm medial tibial augment. 1 year postoperatively their patient had full knee range of motion, could ambulate without assistance and could climb stairs.
Also in 2020, Yun et al. presented the first case series of 34 failed UKAs, half of which were converted robotically to TKA, and half converted manually [8]. No revision components were used in either group. All conversions were performed using primary implants. The authors did observe a difference in the use of stems and augments, with 29% of knees manually converted requiring augments, and 0% of robotically converted knees requiring augments (P = 0.04), however, the manually converted knees utilized a system where stems and augments could be added to their primary components. The authors state they do not believe robotic assistance is inferior to a manual approach in UKA to TKA conversion surgery, however, their study did not offer any clinical outcomes or alignment statistics, only proof of concept. In contrast to our study and the case report by Kalavrytinos et al., Yun et al. did not treat the existing implants as native bone. They used the patient’s remaining bone stock after implant removal to map the bone surfaces on the CT model. Although there was scatter artifact on the pre-op CT, they state the registration passed the 0.5 mm threshold.
The use of robotic assistance in revision knee arthroplasty is not yet licensed or approved by the FDA. The success of this case report, as well as previous studies describing robotics in revision knee arthroplasty [7, 8] questions if this will happen. With frequent advances in robotic technology and software capabilities, the potential for better operative outcomes and broader indications with robotic assistance appears to be increasing. Additional applications to this technology may include shoulder arthroplasty, implantation of megaprostheses for periarticular limb reconstruction, and complex revision hip and knee surgery.
To the knowledge of the authors, this is the first case report to describe the use of robotic arm assist for revision of a failed primary TKA. The surgeon (AK) elected to use Mako technology and a Stryker Triathlon knee revision system. The patient had acceptable radiographic outcomes as assessed on postoperative radiographs by the authors, and the patient had excellent clinical outcomes 6 months postoperatively, with no complaints of knee pain, instability events, or stiffness. The use of robotic technology in rTKA for failed primary TKA is a new technique, and further study should be done to verify its use.
The use of robotic-arm assistance in revision knee arthroplasty is a new, but useful technique. Robotic technology can map over previous implants, make accurate bony cuts, tension soft tissues, and plan for augmentation in cases of bony deficiency. Its use, in this case, resulted in excellent clinical outcomes.
References
- 1.Boylan M, Suchman K, Vigdorchik J, Slover J, Bosco J. Technology-assisted hip and knee arthroplasties: An analysis of utilization trends. J Arthroplasty 2018;33:1019-23. [Google Scholar]
- 2.Hampp EL, Chughtai M, Scholl LY, Sodhi N, Bhowmik-Stoker M, Jacofsky DJ, et al. Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg 2019;32:239-50. [Google Scholar]
- 3.Yang HY, Seon JK, Shin YJ, Lim HA, Song EK. Robotic total knee arthroplasty with a cruciate-retaining implant: A 10-year follow-up study. Clin Orthop Surg 2017;9:169-76. [Google Scholar]
- 4.Park SE, Lee CT. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty 2007;22:1054-9. [Google Scholar]
- 5.Registry AJ. Annual Report. United States: American Joint Replacement Registry; 2014. [Google Scholar]
- 6.Postler A, Lützner C, Beyer F, Tille E, Lützner J. Analysis of total knee arthroplasty revision causes. BMC Musculoskelet Disord 2018;19:55. [Google Scholar]
- 7.Kalavrytinos D, Koutserimpas C, Kalavrytinos I, Dretakis K. Expanding robotic arm-assisted knee surgery: The first attempt to use the system for Knee revision arthroplasty. Case Rep Orthop 2020;2020:4806987. [Google Scholar]
- 8.Yun AG, Qutami M, Chen CM, Pasko KB. Management of failed UKA to TKA: Conventional versus robotic-assisted conversion technique. Knee Surg Relat Res 2020;32:38. [Google Scholar]
- 9.Van der List JP, Chawla H, Joskowicz L, Pearle AD. Current state of computer navigation and robotics in unicompartmental and total knmee arthroplastyu: A systematic review with meta-analysis. Knee Surg Sports Traumatol Arthrosc 2016;24:3482-95. [Google Scholar]
- 10.Khlopas A, Sodhi N, Sultan AA, Chughtai M, Molloy RM, Mont MA. Robotic arm-assisted total knee arthroplasty. J Arthroplasty 2018;33:2002-6. [Google Scholar]
- 11.Siebert W, Mai S, Kober R, Heeckt PF. Technique and first clinical results of robot-assisted total knee replacement. Knee 2002;9:173-80. [Google Scholar]
- 12.Sultan AA, Piuzzi N, Khlopas A, Chughtai M, Sodhi N, Mont MA. Utilization of robotic-arm assisted total knee arthroplasty for soft tissue protection. Expert Rev Med Devices 2017;14:925-7. [Google Scholar]
- 13.Khlopas A, Chughtai M, Hampp EL, Scholl LY, Prieto M, Chang TC, et al. Robotic-arm assisted total knee arthroplasty demonstrated soft tissue protection. Surg Technol Int 2017;30:441-6. [Google Scholar]
- 14.Marchand RC, Sodhi N, Khlopas A, Sultan AA, Harwin SF, Malkani AL, et al. Patient satisfaction outcomes after robotic arm-assisted total knee arthroplasty: A short-term evaluation. J Knee Surg 2017;30:849-53. [Google Scholar]
- 15.Liow MH, Goh GS, Wong MK, Chin PL, Tay DK, Yeo SJ. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: A 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 2017;25:2942-51. [Google Scholar]