Surgical intervention of fibular groove deepening with superior peroneal retinaculum reconstruction results in an excellent outcome for neglected peroneal tendon dislocation.
Dr. Pon Aravindhan A Sugumar, Department of Orthopedics, All India Institute of Medical Sciences, New Delhi, India. E-mail: madhan.ponra@gmail.com
Introduction:Neglected peroneal tendon dislocation with iatrogenic etiology has been rarely reported in the literature and its management has not been fully understood to date.
Case Report:We present a case of a 25-year-old male who presented with pain over the posterolateral aspect of his left ankle which was diagnosed to be a case of neglected peroneal tendon dislocation of iatrogenic etiology. Peroneal groove deepening with superior retinaculum repair was done in the patient along with loose body removal and osteophyte excision. Subsequent fibrosis augmented with the deepening of the groove maintained peroneal tendon position in the retromalleolar groove. On post-operative follow-up, the patient was completely satisfied with relief of pain and no complications. He also regained full range of motion and could walk without support.
Conclusion:Surgical intervention of fibular groove deepening with superior peroneal retinaculum reconstruction results in an excellent outcome for neglected peroneal tendon dislocation
Keywords:Peroneal tendon, Superior peroneal retinaculum, Fibular groove.
Peroneal tendon dislocation is usually a result of trauma with forced dorsiflexion with eversion or inversion in a dorsiflexed ankle [1]. The most common mode of injury described in literature is sports such as skiing, rugby, horse riding, and biking that result in ankle twisting [2]. Lateral sided ankle pain is the most common presenting feature that mimics ankle sprain that results in conservative management from the treating physician at initial period [2]. There might be few anatomical predisposing factors that lead to peroneal tendon subluxation or dislocation such as absence of superior peroneal retinaculum (SPR) (congenital), lateral ankle laxity, or shallow retromalleolar groove [3, 4]. SPR is considered as the most important restraint to dislocation of peroneal tendons [5]. Peroneal tendon dislocations occur mainly because of secondary disruption of the SPR from its insertion along the posterolateral margin of the fibula with or without its displacement of the associated fibrocartilaginous ridge [6]. The true incidence of this pathology is unknown. It is estimated to be around 11–37% in cadaver dissections and up to 30% in patients undergoing surgery for ankle instability [7]. The peroneal tendons have adequate vascular supply that does not cause tendon degeneration over long-term subluxation or dislocation [8].
Iatrogenic injury to SPR leading to peroneal tendon subluxation is a rare clinical entity, and to the best of our knowledge, it is still not reported in the literature to date. There are no specific treatment guidelines regarding neglected presentation following iatrogenic etiology of peroneal tendon dislocation. We describe a case of neglected peroneal tendon dislocation due to an inciting surgical procedure to the ankle.
A 25-year-old male came with complaints of pain over the posterolateral aspect of his left ankle which was present for the past 9 years. The patient was a regular sprinter and had started having pain which was insidious in onset, gradually progressive, non-radiating, and relieved with analgesics and rest. Later, he started experiencing difficulty and pain while walking. He was under conservative management for 3 years which had provided no relief in the symptoms. He was diagnosed to have a loose body in the lateral compartment of the ankle after adequate clinical examination and radiographic analysis (X-rays and computed tomography [CT] scan), for which the surgeon had performed operative excision. Post-surgery, he did not have any relief of symptoms and additionally started noticing a prominent cord-like structure anterior to the fibula. He was kept on symptomatic treatment with physiotherapy by the treating surgeon. After 5 years from the date of surgery, the patient presented to us with pain around the left fibular region and an abnormal cord-like structure anterior to the fibula. On examination, he had an operative scar over the posterolateral aspect of the ankle. There was mild tenderness over the lateral aspect of the ankle below the lateral malleolus. Peroneal tendons were palpated as a cord-like structure anterior to the fibula. These tendons were able to displace posteriorly but again dislocated anteriorly as soon as manual pressure is taken out. There was no obvious structural deformity of the foot. The neurovascular function of the foot and ankle was normal. Signs of posterior impingement were also present. Radiographs disclosed no fractures or dislocations of bony structures (Fig. 1).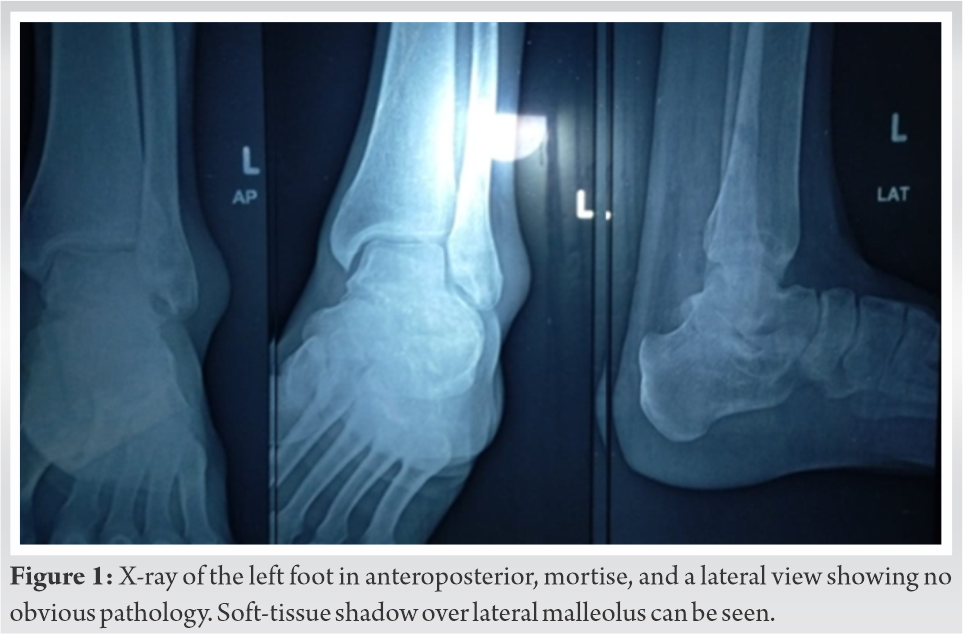
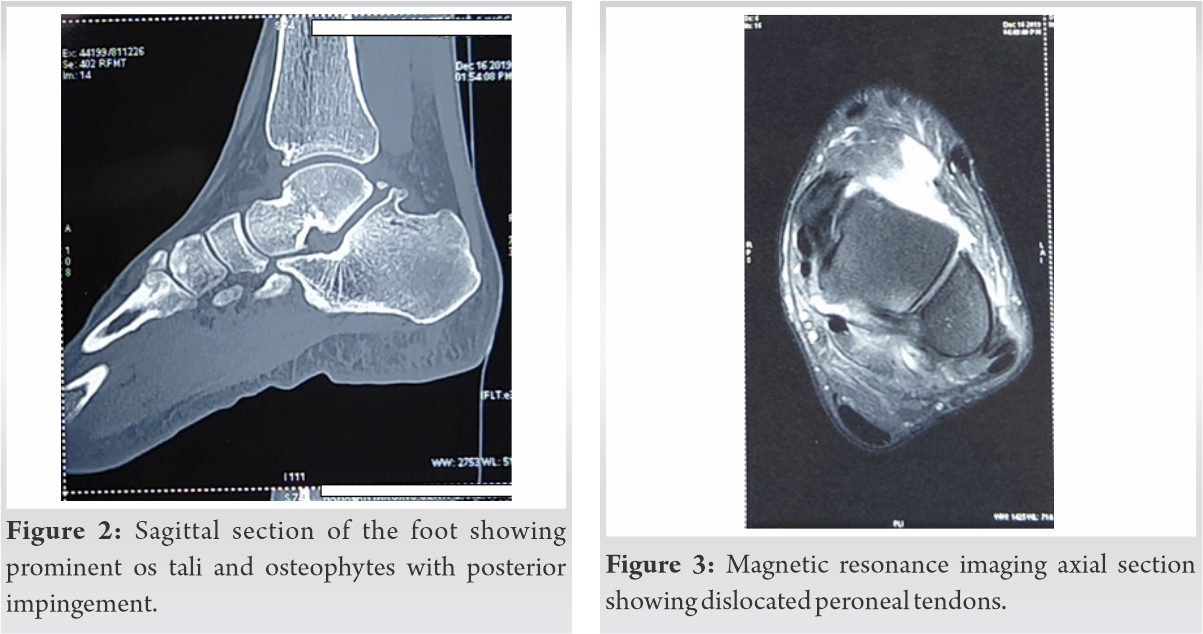
The patient was explained about the need for surgery to stabilize the peroneal tendon and remove the loose body. It was decided to go forward with posterior ankle arthroscopy to recreate the fibular groove for the peroneal tendons as well as to address the posterior impingement syndrome and removal of the loose body. Consent for surgical management was obtained. The patient was positioned prone and standard posterolateral and posteromedial portals were used to debride the fibrofatty tissue. Burring of osteophyte along with prominent os tali was done. A loose body from the lateral gutter was removed (Fig. 4).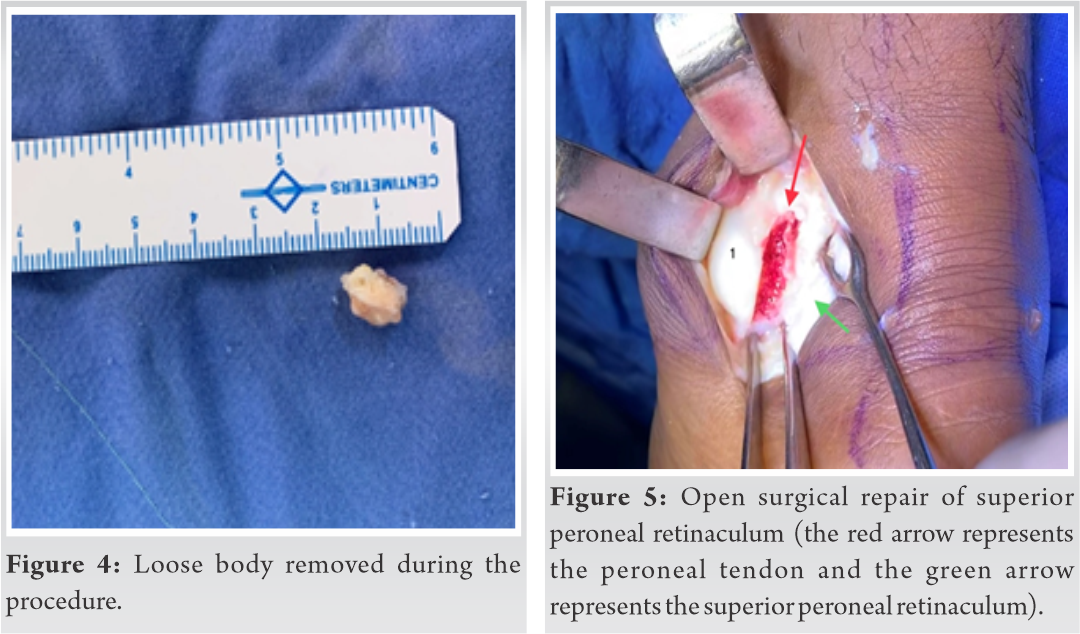
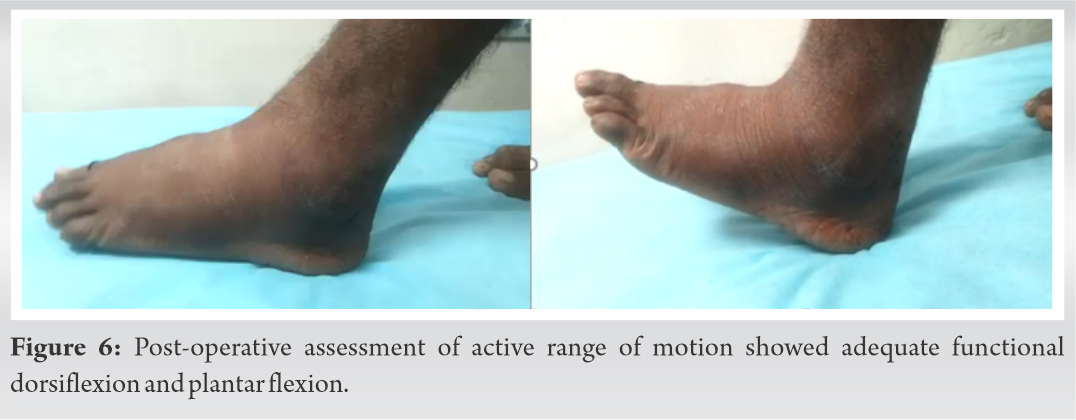
Postoperatively, the patient was mobilized on day 1. The slab was removed and he was started on physiotherapy with a range of motion exercises after 2 days. Partial weight-bearing mobilization with crutches was advised for 2 weeks followed by full weight-bearing mobilization. At the latest follow-up at 2 years, the patient is completely satisfied with relief of pain and no complications. He has the full range of motion and can walk without support without pain.
Peroneal muscles are dynamic stabilizers of ankle and incompetent peroneal renders the mechanically stable ankle into a dynamically unstable one that precludes the patient in enjoying sporting activities. Hence, operative management to be undertaken if the symptoms persists even after adequate trial of conservative management in an appropriately selected physically demanding patient. Radiographic evaluation should consist of weight-bearing anteroposterior (AP) and lateral films according to Ottawa ankle guidelines. In case of any pathology, oblique views should also be done. Roentgenograms usually appear normal though an avulsion flake can be sometimes seen on an internally rotated film. A CT scan can be helpful to evaluate the morphology of the retromalleolar sulcus and the position of the peroneal tendons. An MRI gives a clear picture of the soft-tissue structures and can also detect peroneal tendons in abnormal positions which is common in this condition. Dynamic ultrasound has been recognized to be the most accurate tool for diagnosing peroneal tendon dislocation [9].
Treatment of peroneal tendon dislocation is based on the timing of injury – acute or chronic and the activity level of the patient – athlete or non-athlete. Non-athletes with acute dislocation can be considered for non-operative management though there is a 50% chance of recurring dislocation [10]. Surgical management is advised in case of unsuccessful conservative treatment or chronic instability is present. Acute dislocation in an athlete and chronic dislocation is usually managed surgically.
Various surgical methods are available for peroneal tendon relocation. No specific approach has been proven superior in the available literature. There are five different surgical repair methods which are (1) anatomic reattachment of the retinaculum, (2) reinforcement of the SPR with local tissue transfers, (3) rerouting the tendons behind the calcaneofibular ligament, (4) bone block procedures, and (5) groove deepening procedures. These procedures resulted in excellent outcomes, low recurrence rates, and a high rate of return to sports according to a systematic review [11]. A modified approach for the treatment of chronic subluxation of the peroneal tendons using posteromedial peroneal tendon groove deepening combined with repair of tendon showed satisfactory results [12]. Ziai et al. reported that combined treatment of peroneal tendon dislocation and medial ligamentous laxity following arthroscopy results in excellent outcomes and patient satisfaction [13].
The patient was operated with arthroscopic assisted mini-open approach to get rid of the loose body from the posterolateral gutter of ankle. We anticipated an extensive dissection and exposure if open approaches were to be used to remove the same. The loose body was the causative factor for occasional discomfort felt by patient. There were also osteophytes over the posterior aspect of os tali that caused impingement of peroneal that added to symptoms. Arthroscopy successfully removed the loose body. However, we could not remove the fibrofatty tissue over posterolateral aspect of fibula. Hence, minimally invasive open approach was used to dissect off fibrous tissue as well as to deepen the retromalleolar groove. We noted a false compartment that developed over the posterolateral aspect of fibula that developed due to stripping of periosteum. This finding was also reported in previous case series and was denoted as an equivalent to Bankart lesion [14]. The SPR was noted attenuated that precluded anatomical repair due to prolonged period from injury. Anatomically, SPR is continuous with the periosteum of distal posteromedial aspect of fibula. The periosteum was repaired to fibula with drill holes made to it that obliterated the false compartment to which peroneal was dislocating. The remnant of the periosteum was also repaired with remnant of SPR and fibrous tissue over lateral aspect. To augment this, retromalleolar groove deepening was also performed. A burr was used to deepen the fibrocartilaginous groove. Various methods have been described to augment and repair the SPR. Few authors used to reinforce the retinaculum by passing sutures through drill holes in the distal fibula [14, 15]. The use of Achilles tendon to augment the SPR has been successfully advocated by few surgeons [16, 17]. The deepening of retromalleolar groove has clear advantages in recent literature [2, 18]. The repair or augmentation of SPR along with groove deepening has been proved to be excellent in terms of recurrence of the subluxation [18, 19]. We also performed augmentation of SPR along with groove deepening procedure. The rationale behind the combined procedure was that chronically neglected dislocation could have resulted the shallowness of the fibular groove. Besides, reconstruction of SPR was necessary as there was iatrogenic disruption of the retinaculum during the previous operative procedure (as evident by sharp cut at the remnant of the SPR). There was some distinct difference from the other cases described in literature. The injury to SPR was iatrogenic. There was moderate fibrosis over the lateral fibula that was revealed with lateral radiograph as well as intraoperatively. The fibrocartilaginous rim of groove was completely non-existent in our case with smoothening of the margins. This may be due to prolonged period (5 years) of recurrent subluxation that attenuated the rim (Fig. 6). The associated symptoms of ankle impingement with peroneal tendon subluxation were not reported in any case described previously.
Complications such as recurrent subluxation leading to failure of repair or augmentation, non-return to previous level of activity, and persistent pain have been reported in the literature [2, 6, 14]. Few authors undertook the procedure of groove deepening in revision surgery after failure of SPR repair as initial surgery. However, we did not experience such complications. We addressed all the pathology in the same time (impingement, ligament repair, and groove deepening). We believe that successful outcome depends on addressing of the appropriate pathology not on duration of the symptoms.
Although peroneal tendon dislocations can be seen occasionally in a clinical setting, it is very rare to find a dislocation caused iatrogenically and at the same neglected presentation is a very rare scenario. Surgical intervention is the only treatment option available and a combined procedure consisting of fibular groove deepening with SPR augmentation results in an excellent outcome and return to the pre-injury daily activity levels.
Surgeons should be cautious while treating any case of lateral ankle pain with a history of injury and should always rule out peroneal tendon dislocations with SPR disruption while operating the same. Reconstruction of SPR with groove deepening is a viable option and suturing of periosteum with SPR should be considered while operating a case of chronic neglected peroneal tendon dislocation.
References
- 1.Heckman DS, Reddy S, Pedowitz D, Wapner KL, Parekh SG. Current concepts review: Operative treatment for peroneal tendon disorders. J Bone Joint Surg Am 2008;90:404-18. [Google Scholar]
- 2.Saragas NP, Ferrao PN, Mayet Z, Eshraghi H. Peroneal tendon dislocation/subluxation-case series and review of the literature. Foot Ankle Surg 2016;22:125-30. [Google Scholar]
- 3.Selmani E, Gjata V, Gjika E. Current concepts review: Peroneal tendon disorders. Foot Ankle Int 2006;27:221-8. [Google Scholar]
- 4.Purnell ML, Drummond DS, Engber WD, Breed AL. Congenital dislocation of the peronealtendons inthe calcaneovalgus foot. J Bone Joint Surg Br 1983;65:316-9. [Google Scholar]
- 5.Niemi WJ, Savidakis J Jr., de Jesus JM. Peroneal subluxation: A comprehensive review of the literature with case presentations. J Foot Ankle Surg 1997;36:141-5. [Google Scholar]
- 6.Oesman I, Kurniawan D, Wikanjaya R. Peroneal groove deepening as the treatment of peroneal tendon subluxation: A case report. Int J Surg Case Rep 2019;65:333-8. [Google Scholar]
- 7.Squires N, Myerson MS, Gamba C. Surgical treatment of peroneal tendon tears. Foot Ankle Clin 2007;12:675-95. [Google Scholar]
- 8.Krause JO, Brodsky JW. Peroneus brevis tendon tears: Pathophysiology, surgical reconstruction, and clinical results. Foot Ankle Int 1998;19:271-9. [Google Scholar]
- 9.Pesquer L, Guillo S, Poussange N, Pele E, Meyer P, Dallaudière B. Dynamic ultrasound of peroneal tendon instability. Br J Radiol 2016;89:20150958. [Google Scholar]
- 10.Eckert WR, Davis EJ. Acute rupture of the peroneal retinaculum. J Bone Joint Surg Am 1976;58:670-2. [Google Scholar]
- 11.Suh JW, Lee JW, Park JY, Choi WJ, Han SH. Posterior fibular groove deepening procedure with low-profile screw fixation of fibrocartilaginous flap for chronic peroneal tendon dislocation. J Foot Ankle Surg 2018;57:478-83. [Google Scholar]
- 12.Hu M, Xu X. Treatment of chronic subluxation of the peroneal tendons using a modified posteromedial peroneal tendon groove deepening technique. J Foot Ankle Surg 2018;57:884-9. [Google Scholar]
- 13.Ziai P, Sabeti-Aschraf M, Fehske K, Dlaska CE, Funovics P, Wenzel F, et al. Treatment of peroneal tendon dislocation and coexisting medial and lateral ligamentous laxity in the ankle joint. Knee Surg Sports Traumatol Arthrosc 2011;19:1004-8. [Google Scholar]
- 14.Das De S, Balasubramaniam P. A repair operation for recurrent dislocation of peroneal tendons. J Bone Joint Surg Br 1985;67:585-7. [Google Scholar]
- 15.Alm A, Lamke LO, Liljedahl SO. Surgical treatment of dislocation of the peroneal tendons. Injury 1975;7:14-9. [Google Scholar]
- 16.Jones E. Operative treatment of chronic dislocation of the peroneal tendons. J Bone Joint Surg 1932;14:574-6. [Google Scholar]
- 17.Thomas JL, Sheridan L, Graviet S. A modification of the Ellis Jones procedure for chronic peroneal subluxation. J Foot Surg 1992;31:454-8. [Google Scholar]
- 18.van Dijk PA, Vopat BG, Daniel G, Alastair G, DiGiovanni CW. Retromalleolar groove deepening in recurrent peroneal tendon dislocation: Technique tip. Orthop J Sports Med 2017;5:2325967117706673. [Google Scholar]
- 19.Karlsson J, Eriksson BI, Sward L. Recurrent dislocation of the peroneal tendons. Scand J Med Sci Sports 1996;6:242-6. [Google Scholar]