As posterior hip dislocations are caused by high energy mechanisms, a thorough radiological work up to rule out associated fractures and other systemic injuries should be done promptly and reduction should be done on urgent basis.
Dr. Akshay B Ingale, Department of Orthopaedics, Government Medical College and Hospital, Plot No. 34, Pathan Layout, Sambhaji Nagar, Nagpur - 440 022, Maharashtra, India. E-mail: koolakshay22@gmail.com
Introduction:Traumatic bilateral posterior hip dislocations are seldom seen. These lesions are associated with fractures of acetabulum, proximal femur, or both. With future complications of such injury, immediate closed reduction remains the mainstay of treatment. A radiographic investigation like computed tomography is very sensitive in detecting fracture fragments and thus forms an important part of hip dislocation management in modern practice. Long-term complications of hip dislocation include chondrolysis, avascular necrosis, and secondary osteoarthritis.
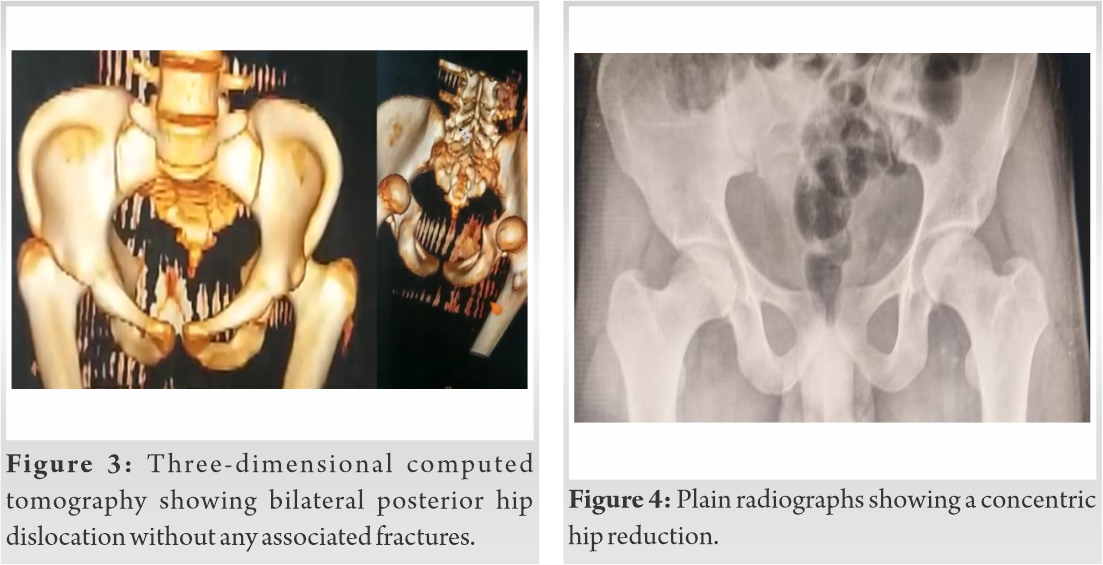
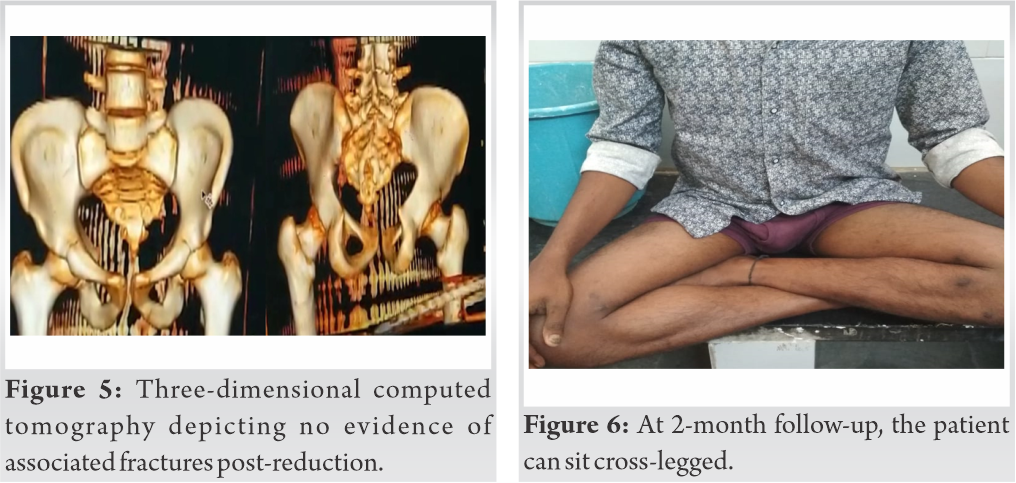
Case Report:In this case report, we present to you an unusual case 23-year-old male who presented to the emergency department with a history of fall from height with an attitude of flexion adduction and internal rotation deformity of bilateral lower limbs. After ruling out life-threatening injuries, initial radiological work-up composed of plain radiographs and computed tomography was suggestive of bilateral posterior hip dislocation without proximal femur and acetabular fractures. Immediate and prompt concentric hip reduction was achieved under general anesthesia. At 1-year follow-up, the patient had uneventful functional outcome and without radiographic complications.
Conclusion: Bilateral posterior hip dislocation is an emergency and requires urgent orthopedic management. The timely and concentric hip reduction is important as it affects the prognosis of such injuries. Computed tomography helps in identifying intra-articular fragments and changes the approach from closed reduction to open reduction. Long-term complications like avascular necrosis should be looked for at regular follow-up.
Keywords: Posterior hip, dislocation, bilateral, traumatic, symmetric.
The hip joint is intrinsically stable joint. Hip joint dislocations usually occur due to high energy trauma and often accompanied by associated injuries. Out of all traumatic dislocations, hip dislocations account for 5% [1]. Bilateral hip joint dislocations are rarely seen in emergencies and documented in the literature [2, 3]. With such high-energy mechanism involved, hip dislocations are usually associated with multisystem injuries requiring detailed evaluation and management [4]. Hip dislocation requires emergency concentric hip reduction. Predictors such as chondral damage, vascular insult, delayed time, and inaccurate reduction negatively impact the prognosis of hip dislocations. These factors are usually associated with complications such as chondrolysis, avascular necrosis, sciatic nerve injury, incarcerated fracture fragments, and heterotopic ossification and on a long-term osteoarthrosis [5]. We present to you a case of bilateral posterior hip dislocation without fracture of acetabulum and proximal femur in a young male without any neurodeficit and associated injuries due to fall from height with excellent clinical and radiological outcome, as such cases are unusual and a handful of cases have been reported.
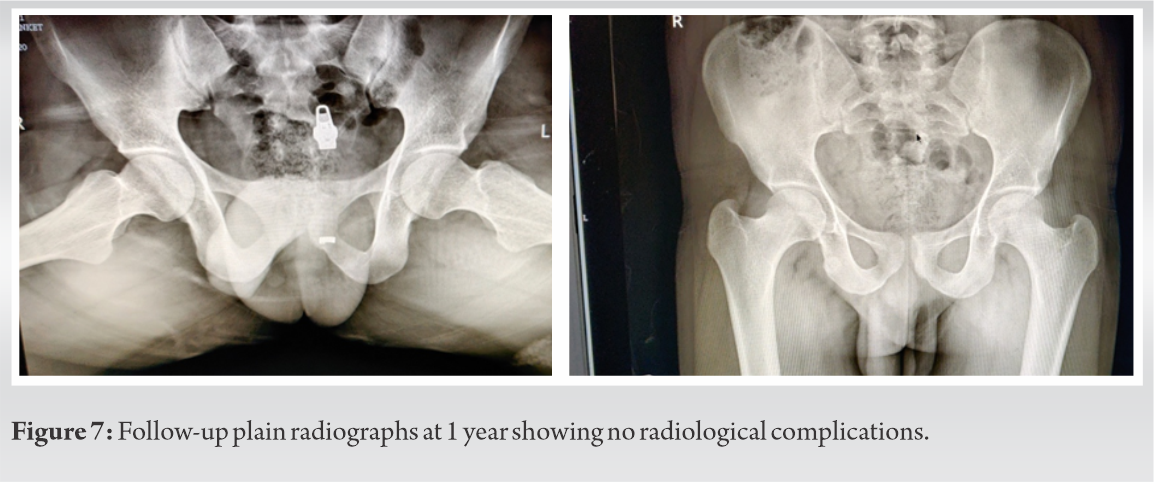
A 23-year-old male patient presented to casualty with a fall from height half an hour ago. The patient sustained trauma while flying a kite from a height of 3 m. With full attention toward flying the kite and no walls over the terrace he lost balance, the patient fell and landed with hips and knee flexed. The patient was brought in the emergency department conscious and oriented with agonizing pain and deformity over bilateral lower limbs. A detailed standard trauma evaluation, multisystem and neurologic examination was carried out to rule out the life-threatening head, chest, and pelvic abdominal injuries at the first survey. Radiological assessment was done to avoid missing injuries. The patient presented with inability to move lower limb, pain, and deformity over bilateral lower limbs. The clinical examination revealed right lower limb in the attitude of 45° of flexion, 10° of adduction, and 10° of internal rotation. The left lower limb was in an attitude of 40° of flexion, 10° of adduction, and 10° of internal rotation (Fig. 1). The range of motion actively was not possible and passively was restricted and painful. On palpation, globular prominence appreciated posteriorly in the gluteal region with intact vascular status. A secondary survey was carried out to rule out associated injuries. Anteroposterior plain radiographs of the pelvis with both hips revealed small femoral heads overlapping the roof of acetabulum confirming the diagnosis of posterior hip dislocations without any proximal femur and acetabulum fractures (Fig. 2). 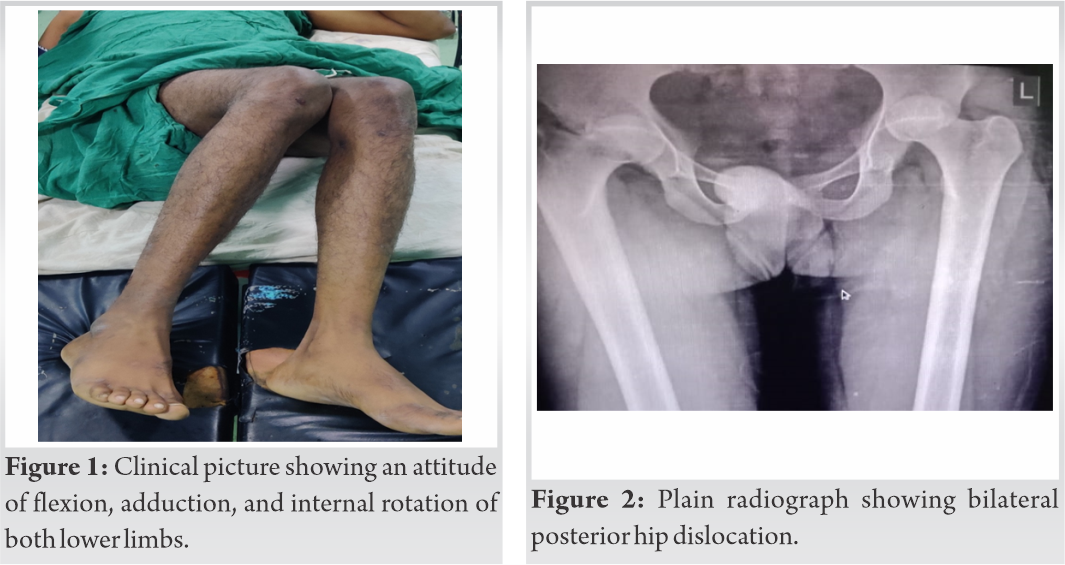
Hip dislocation is classified as anterior and posterior depending on the position of the hip, the force vector applied. Bilateral traumatic posterior hip dislocation without any associated fractures is seldom seen and very few documented in the literature [6]. Greater the flexion and adduction of the hip when a longitudinal force is applied through femur the more chances that it will be a pure dislocation [7].
The most common mode of injury is road traffic accidents followed by fall. Because of the high-energy involved multisystem injuries are common and a thorough trauma evaluation is warranted as these injuries can be missed.[4].
The plain radiograph is the main workhorse in orthopedic evaluation. In such scenarios, computed tomography plays a pivotal role as it is sensitive in detecting intra-articular fragments [8]. Chondrolysis, avascular necrosis, and labral injuries can be assessed by magnetic resonance imaging.
Management of hip dislocations requires prompt and early hip reduction. Usually, hip gets easily reduced when it is pure dislocation rarely requiring an open reduction in cases of fracture-dislocation and buttonholing under soft tissues. Various hip reduction maneuvers have been described in the literature with the principle being traction in line of deformity that relieves muscle spasm. Exaggerating the deformity with slow and steady movements reduces the hip. The reduction should usually be performed under general anesthesia as it decreases the chances of chondral injury which is common due to repeated reduction attempts [9].
Post-operative computed tomography must be performed to rule out any minor intra-articular fragments [8]. A strict physiotherapy protocol must be followed to avoid complications of hip stiffness.
Avascular necrosis is known complication of hip dislocation with time playing an important variable outcome. Other complications include sciatic nerve injury, labral injuries, chondrolysis, and heterotopic ossification in cases of open reduction. The patient should be followed up for long-term complication like osteoarthrosis [10].
Bilateral posterior hip dislocation without associated fractures is an extremely rare and true orthopedic emergency. Prompt and early hip reduction is the most important positive prognostic predictor. This should be supplemented by radiologic confirmation. Follow-up of patient remains the mainstay of treatment to watch for the dreaded complication of avascular necrosis.
Traumatic bilateral posterior hip dislocation is an extremely rare injury. Literature around the world is deficient in such case report. A prompt and timely clinical and radiological workup identifies this injury, thereby reducing time to reduction and thereby complication of avascular necrosis.
References
- 1.Brav EA. Traumatic dislocation of the hip: Army experience and results over a twelve-year period. J Bone Joint Surg Am 1962;44:1115-34. [Google Scholar]
- 2.Ashraf T, Iraqi AA. Bilateral anterior and posterior traumatic hip dislocation. J Orthop Trauma 2001;15:367-8. [Google Scholar]
- 3.Shah FA, Akhtar S, Mehsud WM, Qureshi AR. Bilateral traumatic hip dislocation: Simultaneously one hip anterior and the other posterior a case report. J Pioneering Med Sci 2016;6:113. [Google Scholar]
- 4.Suraci AJ. Distribution and severity of injuries associated with hip dislocations secondary to motor vehicle accidents. J Trauma 1986;26:458-60. [Google Scholar]
- 5.Armstrong JR. Traumatic dislocation of the hip joint. J Bone Joint Surg 1948;30:430-45. [Google Scholar]
- 6.Sahin V, Karakas ES. Traumatic dislocation and fracturedislocation of the hip: A long-term follow up study. J Trauma 2003;54:520-9. [Google Scholar]
- 7.Letournel E. Acetabulum fractures: Classification and management. Orthop Trauma Dir 2007;5:27-33. [Google Scholar]
- 8.Hougaard K, Thomsen PB. Traumatic posterior dislocation of the hip-prognostic factors influencing the incidence of avascular necrosis of the femoral head. Arch Orthop Trauma Surg 1986;106:32-5. [Google Scholar]
- 9.Schafer SJ, Anglen JO. The East Baltimore lift: A simple and effective method for reduction of posterior hip dislocations. J Orthop Trauma 1999;13:56-7. [Google Scholar]
- 10.Clegg TE, Roberts CS, Greene JW, Prather BA. Hip dislocations epidemiology, treatment and outcomes. Injury 2010;41:329-34. [Google Scholar]